
Humor me with calcium: a case report of humoral hypercalcemia of malignancy secondary to cholangiocarcinoma
Highlight box
Key findings
• Humoral hypercalcemia of malignancy (HHM) due to cholangiocarcinoma is associated with poor clinical course, with surgery or chemotherapy being the mainstay of treatment.
What is known and what is new?
• HHM due to cholangiocarcinoma is extremely rare, with only a few cases documented in the literature.
• Despite early detection and rapid correction of the hypercalcemia, disease progression remains poor in the absence of definitive oncologic treatment.
What is the implication, and what should change now?
• Clinicians should maintain a high index of suspicion for HHM in cases of unexplained hypercalcemia, especially in patients with gastrointestinal malignancies. Additionally, further research is needed to explore earlier detection methods and more targeted therapies for HHM due to cholangiocarcinoma.
Introduction
Malignancy-associated hypercalcemia is the most common paraneoplastic syndrome. Hypercalcemia occurs in 2% to 30% of malignancy and is associated with more advanced cases (1). Humoral hypercalcemia of malignancy (HHM) is defined as an overproduction of parathyroid hormone related peptide (PTHrP) from malignant cells and has been described as an overall poor prognostic indicator (1). HHM can be associated with multiple cancers, including squamous cell carcinoma of head and neck, esophagus, lung, breast, ovarian, human T-cell lymphotropic virus-1 lymphoma, and some endocrine tumors (2,3). However, HHM has been rarely associated with cholangiocarcinoma, with few cases reported (2). Symptoms of HHM due to cholangiocarcinoma included gastrointestinal, neurological, renal, and constitutional symptoms (4). Cholangiocarcinoma is the most common malignancy arising from the biliary tree and the second most common hepatic malignancy. This malignancy is defined as an epithelial tumor and accounts for 3% of all gastrointestinal tumors (5). Intrahepatic cholangiocarcinoma is primarily located in the hepatic parenchyma, only accounting for 10% of all cholangiocarcinoma (5,6). Intrahepatic cholangiocarcinoma is divided into various subtypes including conventional, bile ductular, or intraductal neoplasm type (5). Here we present a rare case originally presented at the 2024 American College of Gastroenterology conference on October 17, 2024 with its abstract published in the American Journal of Gastroenterology October 2024 supplement of HHM secondary to cholangiocarcinoma in a 55-year-old woman and discuss the importance of identifying HHM and evaluating for possible gastrointestinal sources in patients with HHM. We present this case in accordance with the CARE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-2024-986/rc).
Case presentation
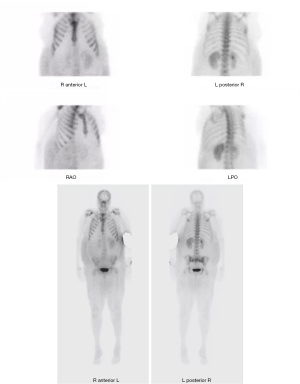
A 55-year-old woman with a history of hypertension, coronary artery disease, and tobacco dependence presented to the hospital with 2 months of worsening weakness and abdominal distension. Additionally, she noted weight loss, despite her expanding abdomen, dizziness, malaise and constipation over this timeframe. Initial labs were notable for a calcium corrected for albumin of 15.8 mg/dL (reference range, 8.4–10.5 mg/dL), total bilirubin 1.0 mg/dL, alkaline phosphatase of 442 U/L, aspartate transaminase (AST) 301 U/L, and alanine transaminase (ALT) 13 U/L. Further testing showed phosphorus 1.5 mg/dL, parathyroid hormone (PTH) was suppressed at <6.0 pg/mL and 25-hydroxy (OH) vitamin D also decreased at 7.0 ng/dL. The hypercalcemia subsequently improved with aggressive intravenous (IV) fluids with 0.9% normal saline initially at a rate of 125 mL/hour, which was then switched to 5% dextrose with 0.45% normal saline at a rate of 150 mL/hour, and 60 mg IV pamidronate. Given the concern for malignancy of unknown primary as a source of hypercalcemia, computed tomography (CT) abdomen/pelvis was ordered, which showed multiple hepatic metastases and ascites, as shown in Figure 1. Diagnostic and therapeutic paracentesis was performed removing 2,320 mL of clear yellow fluid. Cytology showed no evidence of malignancy with serum albumin-ascites gradient (SAAG) of 1.4, indicating portal hypertension, but ascitic fluid protein of 1.6, not indicative of cirrhosis. Further laboratory testing showed serum alpha-fetoprotein (AFP), carcinoembryonic antigen (CEA) and cancer antigen (CA) 19-9 were all normal. Nuclear medicine bone survey showed increased activity in the liver but no osseous activity concerning for malignancy, as highlighted in Figure 2. A liver biopsy revealed metastatic adenocarcinoma positive for cytokeratin-7 (CK7), as shown in Figure 3. Due to re-accumulation of peritoneal fluid, the patient underwent repeat therapeutic paracentesis with removal of 2,500 mL of cloudy red fluid. Subsequent molecular analysis of the liver biopsy demonstrated 90% probability for cholangiocarcinoma. PTHrP was ordered but never collected and given high suspicious for HHM with no metastasis present in the bones, HHM secondary to her active cholangiocarcinoma was the leading diagnosis. The following day, the patient was discharged with close follow up with oncology with plans for further imaging and to consider chemotherapy pending biopsy results. However, due to subsequent hospitalizations, the patient was unable to follow up with oncology outpatient. Patient continued to decline with multiple hospitalizations at an outside facility, ultimately being intubated on her last admission. Due to her functional status, she was not considered a candidate for palliative chemotherapy and unfortunately, around a month after initial diagnosis, the patient passed due to cardiopulmonary arrest.


All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent for publication of this report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Discussion
HHM has been associated with multiple malignancies, especially in those with squamous etiology, including head and neck squamous cell carcinoma, lung, esophageal, breast, ovarian, bladder, and renal cancers (3,7). HHM due to cholangiocarcinoma has been rarely described in literature (3). This condition has been described biochemically as hypercalcemia, hypophosphatemia with decreased levels of PTH and vitamin D 1,25(OH) (8). Currently the main mechanism described for HHM involves overproduction of PTHrP from malignant tissues with suppression of PTH (9). One study has shown that PTHrP is elevated in 80% of HHM (3). PTHrP works by acting on PTH/PTHrP receptors mediating reabsorption of calcium in the renal tubules and stimulates osteoclastic bone activity (3). Through these activities, patients become hypercalcemic due to decreased excretion in combination with increased circulating serum calcium through the osteoclast activity. Our patient was found to be severely hypercalcemic, with decreased levels of PTH and vitamin D 25-OH suggesting likely malignant etiology of these lab values warranting further investigation.
From the few descriptions in the literature of HHM due to cholangiocarcinoma symptoms of HHM secondary to cholangiocarcinoma of 25 patients reported gastrointestinal, renal, neurologic, and constitution symptoms (4). Of these symptoms the majority presented with nonspecific gastrointestinal symptoms with 66%, including 44% due to abdominal pain and 24% with nausea (4). These gastrointestinal symptoms are likely due to the combination of hypercalcemia and the tumor itself. The most common neurologic symptom is disturbances in consciousness with 28%, with the most common renal manifestation being polyuria with 24% (4). Furthermore, 8% had no symptoms at presentation (4). Currently, treatment of choice for HHM due to cholangiocarcinoma is surgical resection; however, for patients who are not surgical candidates, chemotherapy alongside anti-resorptive medications, such as bisphosphonates, aggressive IV fluid hydration with 0.9% normal saline 200–500 mL per hour and calcitonin, is often the treatment (10). Treatments with bisphosphonates include zoledronic acid 4 mg IV, which can be repeated after 7 days and then every 3–4 weeks after, and pamidronate 90 mg IV, which can be repeated every 2–3 weeks (10). For treatment resistant HHM, receptor activator nuclear-kB ligand (RANK-L) inhibitor, denosumab, has been shown to be an alternative (10). HHM due to cholangiocarcinoma tends to have poor outcomes with median survival times between 2–15 months with the use of chemotherapy in unresectable malignancy (9). Often hypercalcemia in HHM due to cholangiocarcinoma is hard to control, as patients remain hypercalcemic or only achieve transient resolution (9). Currently, for patients with more advanced cholangiocarcinoma who are not surgical candidates, first line treatment is combination chemotherapy with gemcitabine and cisplatin (5,11). One study has shown promising results with the addition of nab-paclitaxel, with a single-arm phase 2 trial showing increased median progression free survival time of 19.2 months compared to 11.8 months with control group (11).
This patient’s hypercalcemia with low phosphorus, PTH and vitamin D levels warranted investigation for malignancy. The elevation in alkaline phosphatase, normal ALT and elevated AST revealed a cholestatic pattern of injury, despite imaging demonstrating no evidence of biliary dilatation nor gallbladder pathology. Dilatation of the biliary tract can be a common finding in cholangiocarcinoma, but this patient lacked those characteristic features making for a very mixed presentation. Although a PTHrP level was unavailable, the combination of hypercalcemia, suppressed PTH, and no other malignancy beyond cholangiocarcinoma made HHM the leading diagnosis. Her biopsy showed CK7 positive markers showing likely adenocarcinoma due to cholangiocarcinoma. One study has shown that CK7 expression is correlated with a poorer prognosis, especially in the setting of intrahepatic cholangiocarcinoma (12). This worsened prognosis is likely due to correlation with positive biomarker and aggressive tumor phenotypes, especially in combination with CK19 expression. High expression of either CK7 or CK19 in this tumor after surgical removal has been shown to have a worse postoperative mortality (12). Additionally, while cytological analysis of ascitic fluid is an important diagnostic tool, sensitivity for detecting malignancy has been shown to be around 60%, often leading to false-negative results influenced by various factors such as peritoneal carcinomatosis (13). Highlighting the importance of further investigations for intraabdominal malignancies, as was performed in our patient. Her case warranted a multi-disciplinary approach between endocrinology, oncology, and gastroenterology. Surgical resection may be curative for cholangiocarcinoma but unlikely in metastatic disease (11). The few case reports of PTHrP-secreting cholangiocarcinoma all had poor outcomes, even with chemotherapy treatment. This was similar to our patient, as she died within a month after her initial presentation, further underscoring the value of identifying hypercalcemia etiologies and cholangiocarcinoma in a timely fashion.
Conclusions
HHM is a very rare presentation in cholangiocarcinoma and has been shown to be a poor prognostic factor in this malignancy. Moreover, CK7 and CK19 expression have also been shown to have negative affect on survival in patients with intrahepatic cholangiocarcinoma. Given the complexity these cases can present as, a multi-disciplinary approach should be utilized to assure appropriate management of these patients. Various specialties, such as oncology, endocrinology, and gastroenterology, can provide input for optimal care for these patients. This patient had an atypical presentation and underscores the importance of considering gastrointestinal sources of malignancy when hypercalcemia is significant in labs. HHM can be an indicator of poor prognosis, thus it is important to further risk stratify and initiate a proper workup and treatment, if intervention is possible. Overall, HHM in cholangiocarcinoma has been poorly studied due to the rarity; however, further research in detecting these processes earlier and improved treatments is warranted as all cases of this process have had poor outcomes.
Acknowledgments
This case’s abstract was initially presented at the 2024 American College of Gastroenterology conference on October 17, 2024, and published in the American Journal of Gastroenterology October 2024 supplement.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-2024-986/rc
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-2024-986/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-2024-986/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent for publication of this case report and accompanying images was not obtained from the patient or the relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- El-Hajj Fuleihan G, Clines GA, Hu MI, et al. Treatment of Hypercalcemia of Malignancy in Adults: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 2023;108:507-28. [Crossref] [PubMed]
- Harsch IA, Konturek PC. Humoral Hypercalcemia in a Patient with Cholangiocellular Carcinoma - Effective Therapy with Denosumab. Am J Case Rep 2019;20:1325-30. [Crossref] [PubMed]
- Lim S, Han J, Park KH, et al. Two cases of humoral hypercalcemia of malignancy in metastatic cholangiocarcinoma. Cancer Res Treat 2013;45:145-9. [Crossref] [PubMed]
- Ito J, Sakai K, Yamamoto Y, et al. Recurrent distal cholangiocarcinoma and humoral hypercalcemia of malignancy: report of a rare case and literature review. Endocr J 2023;70:375-84. [Crossref] [PubMed]
- Rodrigues PM, Olaizola P, Paiva NA, et al. Pathogenesis of Cholangiocarcinoma. Annu Rev Pathol 2021;16:433-63. [Crossref] [PubMed]
- Harrison JM, Visser BC. Cholangiocarcinoma. Surg Clin North Am 2024;104:1281-93. [Crossref] [PubMed]
- Almuradova E, Cicin I. Cancer-related hypercalcemia and potential treatments. Front Endocrinol (Lausanne) 2023;14:1039490. [Crossref] [PubMed]
- Xynos ID, Sougioultzis S, Zilos A, et al. Hypercalcemia in a patient with cholangiocarcinoma: a case report. Int Arch Med 2009;2:35. [Crossref] [PubMed]
- Ashihara N, Nakajima K, Nakamura Y, et al. Denosumab is Effective for Controlling Serum Calcium Levels in Patients with Humoral Hypercalcemia of Malignancy Syndrome: A Case Report on Parathyroid Hormone-related Protein-producing Cholangiocarcinoma. Intern Med 2016;55:3453-7. [Crossref] [PubMed]
- Mc Donald D, Drake MT, Crowley RK. Treatment of hypercalcaemia of malignancy in adults. Clin Med (Lond) 2023;23:503-7. [Crossref] [PubMed]
- Moris D, Palta M, Kim C, et al. Advances in the treatment of intrahepatic cholangiocarcinoma: An overview of the current and future therapeutic landscape for clinicians. CA Cancer J Clin 2023;73:198-222. [Crossref] [PubMed]
- Liu LZ, Yang LX, Zheng BH, et al. CK7/CK19 index: A potential prognostic factor for postoperative intrahepatic cholangiocarcinoma patients. J Surg Oncol 2018;117:1531-9. [Crossref] [PubMed]
- Jackson K, Frew K, Johnston R, et al. Indwelling Peritoneal Catheter for Ascites Management in a UK District General Hospital: A Cohort Study. Healthcare (Basel) 2021;9:1254. [Crossref] [PubMed]


