
Biomarker-driven therapeutic strategies in advanced gastric cancer: a case series of curative responses
Highlight box
Key findings
• Four patients with initially unresectable/metastatic gastric cancer (UMGC) achieved pathologic complete response or sustained clinical response following biomarker-driven therapy.
• Dual blockade with anti- human epidermal growth factor receptor 2 (HER2) and immune checkpoint inhibitors plus chemotherapy led to significant tumor regression and, in some cases, curative surgery.
What is known and what is new?
• Advanced GC has traditionally been treated with palliative chemotherapy.
• Biomarker-driven therapies, including HER2-targeted agents and programmed cell death ligand 1 (PD-L1) inhibitors, are now expanding curative options for select UMGC patients.
What is the implication and what should change now?
• Biomarker-driven therapies, particularly dual HER2 and PD-L1 blockade, can transform the treatment landscape for advanced GC by converting unresectable cases into surgically treatable ones, offering a potential path to cure rather than palliative care.
• Routine biomarker testing (including HER2, PD-L1, and microsatellite instability status) should be implemented early in the diagnostic process for GC to guide personalized treatment strategies, ensuring that eligible patients receive targeted neoadjuvant therapies with curative intent.
Introduction
Gastric cancer (GC) is the fifth leading cause of cancer-related deaths globally, with more than 659,000 fatalities and over 900,000 million cases reported in 2022 (1). In the United States alone, more than 22,000 new cases and approximately 10,800 GC-related deaths occurred in 2024 (2). While surgery remains the primary curative option, the advanced stage at which GC is often diagnosed results in poor prognoses.
Perioperative chemotherapy has been shown to improve survival in resectable GC cases by downstaging tumors (3). However, there is no standardized management approach for patients with locally advanced, unresectable, non-metastatic GC due to the heterogeneity in molecular characteristics and responses to treatment. The question remains whether patients with limited metastatic GC or advanced unresectable GC who respond to systemic treatment should be considered for curative surgery.
In this manuscript, we present four cases of advanced GC in patients treated with neoadjuvant chemotherapy, incorporating anti-programmed cell death ligand 1 (PD-L1) and human epidermal growth factor receptor 2 (HER2)-targeted therapies, achieving either pathologic complete responses (pCR) or significant sustained responses. These cases illustrate how biomarker-driven treatments are changing the landscape of advanced GC management. We present this article in accordance with the AME Case Series reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-825/rc).
Case presentation
Case 1
A 54-year-old female with a past medical history of diabetes, hypothyroidism, and anemia, presented to the emergency department with complaints of early satiety and abdominal pain. On presentation, her complete blood count (CBC) showed a hemoglobin (Hgb) of 9.1 g/dL. A computed tomography (CT) scan of the abdomen revealed a 4.4-cm mass along the lesser curvature of the stomach with evidence of regional perigastric/gastrohepatic lymph nodes up to 10 mm in size. Esophagogastroduodenoscopy (EGD) and endoscopic ultrasound (EUS) demonstrated a 5 cm × 6 cm mass at the level of the distal fundus and proximal body, extending circumferentially along both the greater and lesser curvatures of the stomach. Additionally, three gastric polyps and malignant appearing perigastric nodes were identified.
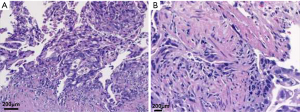
Biopsy of the mass confirmed a moderately differentiated adenocarcinoma infiltrating the gastric mucosa and extending into the smooth muscle. Immunohistochemistry (IHC) showed microsatellite stability (MSS) and HER2 overexpression (3+ by IHC) (Figure 1), with background findings of chronic gastritis and goblet cell metaplasia. The tumor extended into the subserosal connective tissue without invasion of the visceral peritoneum or adjacent structures. Fine needle aspiration (FNA) biopsy of the lymph nodes was not performed. A repeat CT scan 1 month later showed an increase in tumor size to approximately 6 cm. Diagnostic laparoscopy with peritoneal washings showed no evidence of metastatic disease in the abdomen. Further staging with positron emission tomography/computed tomography (PET-CT) did not reveal any distant metastasis. After laparoscopy the stage was determined to be cT3N2M0. Her Eastern Cooperative Oncology Group (ECOG) status was 2. Genetic testing was conducted and revealed no clinically significant variants.
The patient received perioperative systemic chemotherapy with one cycle of FLOT regimen [oxaliplatin 85 mg/m2, fluorouracil 2,400 mg/m2, leucovorin 20 mg/m2, docetaxel 50 mg/m2 intravenously (IV)]. Notably, her hospital course was complicated by diabetic ketoacidosis and streptococcal bacteremia. Docetaxel was removed from cycle 2 given her previous complications. She tolerated and completed a total of 4 cycles of chemotherapy with fluorouracil, leucovorin, oxaliplatin (FLO). Restaging CT abdomen/pelvis demonstrated an increase in the primary mass. Due to disease progression, including primary tumor enlargement and potential involvement of regional lymph nodes and suboptimal performance status, the patient was deemed unsuitable for surgery.
Therefore, the patient received folinic acid, fluorouracil, oxaliplatin (FOLFOX)/pembrolizumab/trastuzumab (pembrolizumab 200 mg once every 3 weeks, trastuzumab at a dose of 6 mg/kg intravenously once every 3 weeks following an initial loading dose of 8 mg/kg). Notably, combined positive score (CPS) or tumor proportion score (TPS) scores were not obtained on pathology as the combination regimen was approved at the time of the patient’s treatment regardless of PD-L1 testing. Restaging CT scan showed significant improvement: the gastric fundal mass was no longer visualized, the previously noted perigastric lymph nodes had resolved, and no suspicious soft tissue or osseous lesions were identified.
Given these findings, the patient was reevaluated for surgical resection. A diagnostic laparoscopy revealed no distant or peritoneal disease and an EGD showed tumor regression below the esophagogastric junction. She subsequently underwent a total gastrectomy with extended D2 lymphadenectomy, Roux-en-Y esophagojejunostomy, and omentectomy. The surgery was successful with negative proximal margins. Pathologic analysis showed no residual carcinoma in the tumor bed and no definite dysplasia in the background of intestinal metaplasia (Figure 2). All lymph nodes in the stomach/omentum [22], porto-hepatic [8], and porto-venous [3] resections margins were negative. A new IHC HER2 score was not repeated on the surgical specimen. The patient achieved complete pathological response and recovered well from surgery. She remained disease-free following curative surgery since 2020.

Case 2
A 68-year-old male, with no prior past medical history, presented to the emergency department with fatigue and dysphagia with a CBC revealing a Hgb of 6.5 g/dL. A CT scan of the chest, abdomen, and pelvis indicated a gastric mass near the cardia/fundus with lymphadenopathy of the retroperitoneal, perihepatic, peripancreatic, nodal stations as well as prominent mediastinal, right iliac, and left perirectal nodes. Subsequent EGD, revealed a fungating mass in the gastric cardia, and pathologic examination confirmed invasive, poorly differentiated adenocarcinoma. Staging PET/CT demonstrated widespread lymph node metastases, involving the lower neck, thorax, abdomen, and pelvis, consistent with stage IV disease. As a result, exploratory laparotomy at this point was deemed unnecessary. IHC showed the tumor had MSS and biomarker analysis revealed HER2+/fluorescence in situ hybridization (FISH) positive, PD-L1 CPS of 45, and a low tumor mutational burden (TMB) of less than 10 mutations per million base pairs. The patient’s ECOG status was 0, and given the data, the patient was deemed not resectable.
The patient was started on the KN811 regimen which included pembrolizumab (200 mg every 3 weeks), trastuzumab (6 mg/kg intravenously every 3 weeks following an initial 8 mg/kg loading dose), capecitabine (1,000 mg/m2 orally twice daily on days 1–14 of each 3-week cycle), and oxaliplatin (130 mg/m2 administered intravenously every 3 weeks). After 6 months of treatment, the patient displayed a positive response in both primary and metastatic sites and achieved clinical complete response (CR) after 12 months of therapy. Following multidisciplinary tumor board discussion, trastuzumab was discontinued and the patient was de-escalated to capecitabine monotherapy for an additional 12 months, during which no evidence of disease (NED) was noted. The patient remains on pembrolizumab.
However, the reappearance of dysphagia prompted a repeat EGD, which revealed a recurrent cardia mass with invasive poorly differentiated adenocarcinoma. Restaging PET/CT showed new hypermetabolic activity in the proximal stomach [5.9 cm × 3.4 cm, standardized uptake value (SUV) 20]. The patient was rechallenged with the KN811 regimen for four cycles, resulting in stable disease at the primary site with no evidence of distant metastasis. Surgical re-evaluation and diagnostic laparoscopy indicated no peritoneal disease, making him a potential candidate for resection.
The patient subsequently underwent a total gastrectomy with D2 lymph node dissection and Roux-en-Y esophagojejunostomy, performed using robotic assistance (Xi RA model). Final pathology demonstrated ypT3N0M0, with 0 out of 64 lymph nodes positive for malignancy and removal of the portacaval lymph nodes. Intraoperative findings also revealed extensive retroperitoneal fibrosis in the regional nodal stations. Postoperatively, the tumor tested HER2-negative, MSS, and PD-L1 CPS 30, HER2 IHC 0. At 12 months post-surgery follow-up, the patient remained without radiographic evidence of disease.
Case 3
A 66-year-old male, with no prior past medical history, presented to his primary care physician with abdominal distention and an unintentional weight loss of twenty pounds. CBC revealed a Hgb of 10.8 g/dL. A CT scan of the abdomen and pelvis identified multiple peritoneal nodules and the presence of ascites, raising suspicions of peritoneal carcinomatosis. The patient’s condition deteriorated, leading to an emergency room visit. CT imaging revealed substantial ascites, prompting a paracentesis the following day, yielding 4.4 liters of blood-tinged fluid. Two weeks later, a CT scan of the chest, abdomen, and pelvis confirmed disseminated peritoneal malignancy, characterized by moderate volume ascites, widespread retroperitoneal involvement, and nodal metastases in the gastrohepatic ligament. Ascites cytology was consistent with adenocarcinoma, leading to a diagnosis of stage IV gastric adenocarcinoma with peritoneal involvement. His ECOG status was 1.
Biomarker analysis revealed HER2 positivity IHC 3+ with a CPS of 2. The patient was initiated on FOLFOX (oxaliplatin 85 mg/m2, fluorouracil 2,400 mg/m2, leucovorin 20 mg/m2) combined with trastuzumab (6 mg/kg intravenously every 3 weeks after an initial loading dose of 8 mg/kg) every 2 weeks, along with pembrolizumab (200 mg) every 4 weeks for a total of nine cycles. Due to neuropathy and oxaliplatin toxicity, the regimen was adjusted to 5-fluorouracil, leucovorin, pembrolizumab, and trastuzumab, every 4 weeks, for an additional six cycles.
Subsequent laparoscopy revealed no evidence of peritoneal disease and PET/CT showed no distant metastasis aside from the primary tumor in the gastric body. After 12 months of systemic therapy with no radiographic evidence of metastatic disease, the patient underwent robotic-assisted distal gastrectomy with Roux-en-Y reconstruction. Pathological analysis of the gastrectomy specimen revealed poorly differentiated invasive adenocarcinoma of the solid type, with invasion through the muscularis propria and extension into the subserosa, with less than 0.5 mm proximity to the serosa. A partial treatment response was noted, with a score of 2. Metastatic adenocarcinoma was identified in 3 of 32 lymph nodes (3/32), while the surgical margins were negative. Pathological examination of the gastric mucosa revealed both complete and incomplete types of intestinal metaplasia, alongside mild chronic inactive gastritis. Pathological staging per American Joint Commission on Cancer (AJCC) 8th edition classified the tumor as ypT3N1. No peritoneal disease was found, with fibroadipose tissue negative for malignancy. Repeat IHC for HER2 was 1+. The patient completed two years of adjuvant pembrolizumab and trastuzumab. Serial CT scans show NED.
Case 4
An 80-year-old female with a medical history of diabetes, gastroesophageal reflux, hypertension, and hyperlipidemia presented to the emergency department with a near-syncopal episode and coffee-ground emesis in 2019. She was found to have severe anemia, with a CBC revealing a Hgb level of 5.7 g/dL. A CT scan of the abdomen and pelvis revealed possible gastric thickening, although evaluation was limited by non-distension as well as nonspecific sub-centimeter perigastric lymph nodes. An EGD revealed a large 3–4 cm ulcerated, friable gastric mass located 5 cm below the Z-line along the greater curvature of the gastric body. A EUS demonstrated two indeterminate regional lymphadenopathies, with the mass penetrating beyond the muscularis propria and extending into the adventitia but without invasion of the visceral peritoneum or adjacent structures. Biopsy of the gastric mass confirmed ulcerated, moderate-to-poorly differentiated adenocarcinoma of intestinal type. Staging PET-CT did not reveal distant metastasis, leading to a clinical staging of cT3N1M0. Her ECOG status was 2.
Biomarker analysis revealed microsatellite instability-high (MSI-H), PD-L1 with a CPS of 70, and the tumor was negative for HER2 amplification. MSI-H status was confirmed by Idylla reverse transcription-polymerase chain reaction (rtPCR). Given her suboptimal performance status, the patient received 7 cycles of FOLFOX chemotherapy (oxaliplatin 85 mg/m2, fluorouracil 2,400 mg/m2, leucovorin 20 mg/m2) in the perioperative setting given suboptimized performance status.
Four additional cycles of nivolumab (240 mg every 2 weeks) were administered in combination with FOLFOX. Although HER2-negative, the patient’s MSI-H biomarker status predicted a favorable response, and she achieved pCR.
After completing a total of 11 cycles of FOLFOX and 4 cycles of nivolumab, she underwent a partial gastrectomy with extended D1 lymph node dissection. Intraoperative EGD revealed marked treatment response, and laparoscopy confirmed no evidence of peritoneal carcinomatosis. Pathologic examination of the resected specimen showed no residual adenocarcinoma in the tumor bed. Both proximal and distal margins were negative for tumor involvement. A liver core biopsy was negative for metastasis, and excisional biopsy of five hepatic artery lymph nodes showed no evidence of metastatic carcinoma (0/5). Additionally, none of the 56 perigastric lymph nodes contained tumor deposits.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent for publication of this case series and accompanying images was not obtained from the patients or the relatives after all possible attempts were made.
Discussion
Recent advancements in systemic therapy, including the use of HER2-targeted agents and immune checkpoint inhibitors (ICIs), offer the possibility of converting unresectable disease into surgical candidates, leading to improved survival outcomes (4,5). Neoadjuvant therapy, particularly in combination with biomarker-guided treatments, has emerged as a valuable tool for downstaging tumors in some cases. The 4th case was treated prior to the publication of the NEONIPIGA study (6). Ideally, given the patient’s advanced age, treatment with ICI alone in the neoadjuvant setting might have been a preferable approach. PD-L1, MSI, and HER2 status are essential biomarkers that can inform treatment decisions in advanced GC (7).
The variability in responses among patients, despite similar regimens, highlights the influence of factors such as tumor biology (HER2, PD-L1, MSI status), tumor microenvironment (immune cell infiltration, stromal composition), and baseline disease burden (tumor size, nodal involvement, metastatic sites). Additionally, patient-specific factors, including age, performance status, and comorbidities, may further modulate treatment efficacy and tolerability.
More patients with unresectable GC are benefiting from treatments targeting HER2, fibroblast growth factor receptor 2 (FGFR2), and Claudin 18.2 (CLDN18.2), combined with chemotherapy and ICI (8). These treatments are showing better responses, which may lead to longer survival for many patients. Additionally, the potential for conversion to surgical candidacy may depend significantly on the sites of metastasis (9).
Conclusions
Here, we present a case series of advanced gastric adenocarcinoma patients who achieved sustained responses through biomarker-driven systemic treatment combined with ICI and chemotherapy. Initially deemed unsuitable for surgery, both patients received tailored neoadjuvant therapies based on their molecular profiles. The first patient, with MSI-H and PD-L1 positivity, underwent four cycles of nivolumab plus FOLFOX, while the second, with HER2 overexpression, received pembrolizumab, trastuzumab, and FOLFOX. Both achieved pCR, highlighting the efficacy of these regimens. These outcomes align with the U.S. Food and Drug Administration’s (FDA) recent approvals of nivolumab (April 2021) and pembrolizumab (March 2021) as first-line treatments for locally advanced GC in combination with systemic therapy.
Acknowledgments
None.
Footnote
Reporting Checklist: The authors have completed the AME Case Series reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-825/rc
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-825/prf
Funding: None.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-825/coif). C.T.H. serves as an unpaid editorial board member of Journal of Gastrointestinal Oncology from January 2025 to December 2026. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration and its subsequent amendments. Written informed consent for publication of this case series and accompanying images was not obtained from the patients or the relatives after all possible attempts were made.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024;74:229-63. [Crossref] [PubMed]
- Siegel RL, Giaquinto AN, Jemal A. Cancer statistics, 2024. CA Cancer J Clin 2024;74:12-49. [Crossref] [PubMed]
- Yıldız İ, Özer L, Şenocak Taşçı E, et al. Current trends in perioperative treatment of resectable gastric cancer. World J Gastrointest Surg 2023;15:323-37. [Crossref] [PubMed]
- Högner A, Moehler M. Immunotherapy in Gastric Cancer. Curr Oncol 2022;29:1559-74. [Crossref] [PubMed]
- Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 2010;376:687-97. [Crossref] [PubMed]
- André T, Tougeron D, Piessen G, et al. Neoadjuvant Nivolumab Plus Ipilimumab and Adjuvant Nivolumab in Localized Deficient Mismatch Repair/Microsatellite Instability-High Gastric or Esophagogastric Junction Adenocarcinoma: The GERCOR NEONIPIGA Phase II Study. J Clin Oncol 2023;41:255-65. [Crossref] [PubMed]
- Pereira MA, Ramos MFKP, Dias AR, et al. Expression Profile of Markers for Targeted Therapy in Gastric Cancer Patients: HER-2, Microsatellite Instability and PD-L1. Mol Diagn Ther 2019;23:761-71. [Crossref] [PubMed]
- Inamoto R, Takahashi N, Yamada Y. Claudin18.2 in Advanced Gastric Cancer. Cancers (Basel) 2023;15:5742. [Crossref] [PubMed]
- Al-Batran SE, Goetze TO, Mueller DW, et al. The RENAISSANCE (AIO-FLOT5) trial: effect of chemotherapy alone vs. chemotherapy followed by surgical resection on survival and quality of life in patients with limited-metastatic adenocarcinoma of the stomach or esophagogastric junction - a phase III trial of the German AIO/CAO-V/CAOGI. BMC Cancer 2017;17:893. [Crossref] [PubMed]


