Metachronous pancreatic metastasis of an ovarian serous papillary adenocarcinoma after 8 years
Introduction
The majority of pancreatic tumours are primary. Pancreatic metastases are rare (3,8% of pancreatic lesions) (1), and are more commonly reported in patients with renal cell carcinoma. Metastases of ovarian cancer to the pancreas are very rare but have been reported in the literature (2).
We report a very unusual case of a metachronous pancreatic metastasis from an ovarian cancer occurred 8 years after the first diagnosis.
Case report
We describe a 70 year-old Caucasian female with a prior history (8 years previously) of bilateral hysteroannesiectomy because of ovarian and uterine serous papillary adenocarcinoma poorly differentiated G3 (pT1c, N0), that presented with jaundice.
Her past medical history revealed hypertension, Wegener Granulomatosis and bronchial asthma.
Laboratory test results included the following: bilirubin 10.1 mg/dL (normal 0.3-1.2 mg/dL); alanine aminotransferase 478 IU/L (0-40 IU/L); alkaline phosphatase 2667 IU/L (70-290 IU/L); γGT 2853 IU/L (0-50 IU/L); Ca19-9 35,3 U/mL (0.0-37 IU/mL); CA 125 90,8 U/mL (0.0-35 IU/mL).
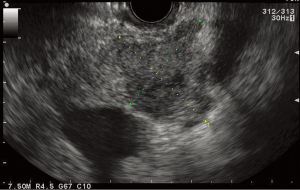
Abdominal ultrasound revealed common bile duct (CBD) dilation (20 mm diameter) with concomitant dilatation of intrahepatic biliary tree.
The abdominal CT scan showed a 2.5 cm × 3 cm hypodense pancreatic head lesion involving the portal vein (Figure 1).
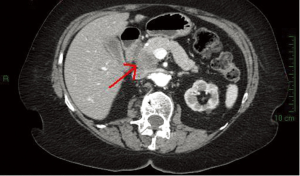
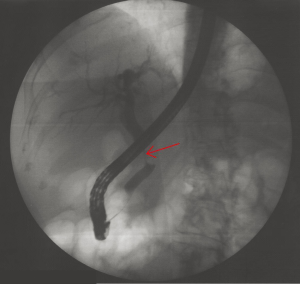
An EUS (Figure 2) confirmed the presence of the pancreatic mass involving the portal vein with CBD stenosis; fine needle aspiration (FNA) was therefore performed with subsequent therapeutic ERCP (Figure 3) with biliary stenting.
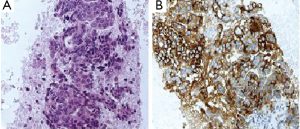
Pathology revealed the presence of adenocarcinoma with CA 125 expression at immunohistochemistry (Figure 4), compatible with ovarian pancreatic metastasis.
The patient is currently receiving repeat chemotherapy with carboplatin and taxol and is now in stable conditions.
Discussion
Tumours metastasizing to the pancreas are unusual and published series are limited by few patients (3). Pancreatic metastases are quite rare, usually found incidentally, and are more commonly reported in patients with renal cell carcinoma, melanoma, lung, colon or breast cancer (4). Due to the low incidence of pancreatic metastasis, most masses of the pancreas are assumed to be primary pancreatic neoplasms (5).
Tissue diagnosis is imperative because imaging alone is incapable of differentiating metastases from primary pancreatic tumours. EUS-FNA allows cytodiagnosis and can have a decisive influence on the selection of appropriate therapeutic strategies (6).
Therefore, a tissue biopsy should be always required particularly in patients with past medical history of neoplasia, to truly differentiate between primary and secondary tumours in order to avoid misdiagnosis and delay in possible treatment.
Our case describes a rare case of a metachronous pancreatic metastasis from an ovarian cancer occurred 8 years after the first diagnosis. There are only few case reports in the literature of ovarian adenocarcinoma metastsis to the pancreas (7,8) and to our knowledge this is the first description of one occurred 8 years after the first diagnosis.
The patient presented with jaundice and imagine techniques revealed a pancreatic head lesion infiltrating the portal vein, initially assumed to be a primary pancreatic tumour.
Because of the previous history of ovarian neoplasia, EUS-FNA of the pancreatic lesion was performed and positive immunohistochemestry with anti CA-125 revealed the presence of a pancreatic metastasis from ovarian cancer and specific chemotherapy with carboplatin and taxol was therefore started.
In conclusion, although rare, pancreatic metastasis is an important cause of focal pancreatic lesions.
Tissue biopsy should be always obtained in order to differentiate primary from secondary pancreatic tumours and to rapidly direct a patient’s appropriate therapy, both in terms of chemotherapy and surgery.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Volmar KE, Vollmer RT, Jowell PS, et al. Pancreatic FNA in 1000 cases: a comparison of imaging modalities. Gastrointest Endosc 2005;61:854-61. [PubMed]
- Pingpank JF Jr, Hoffman JP, Sigurdson ER, et al. Pancreatic resection for locally advanced primary and metastatic nonpancreatic neoplasms. Am Surg 2002;68:337-40; discussion 340-1. [PubMed]
- Konstantinidis IT, Dursun A, Zheng H, et al. Metastatic tumors in the pancreas in the modern era. J Am Coll Surg 2010;211:749-53. [PubMed]
- Robbins EG 2nd, Franceschi D, Barkin JS. Solitary metastatic tumors to the paqncreas: a case report and review of the literature. Am J Gastroenterol 1996;91:2414-7. [PubMed]
- Fritscher-Ravens A, Sriram PV, Krause C, et al. Detection of pancreatic metastases by EUS-guided fine-needle aspiration. Gastrointest Endosc 2001;53:65-70. [PubMed]
- Sparks DA, Chase DM, Forsyth M, et al. Late presentation of a mucinous ovarian adenocarcinoma which was initially diagnosed as a primary pancreatic carcinoma: a case report and review of the literature. J Med Case Rep 2010;4:90. [PubMed]
- Kumar V. eds. Robbins and Cotran Pathologic Basis of disease. Philadelphia: Saunders, 7, 2004.
- Schumacher A. Delayed diagnosis of ovarian cancer with metastasis to the pancreas. Zentralbl Gynakol 1993;115:568-9. [PubMed]