Treatment outcome of gastric extra-nodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type in the Hong Kong Chinese population: a single centre experience
Introduction
Extra-nodal marginal zone B-cell lymphoma of mucosa-associated lymphoid tissue type (EMZBL-MALT) in stomach was commonly related to Helicobacter pylori (HP) infection. In the past, gastrectomy was a prevalent treatment for this disease but nowadays, HP eradication therapy is considered first-line treatment for HP-positive subjects while single-agent chemotherapy (oral alkylating agents) or radiotherapy would be considered for HP-negative subjects with localized disease (1-9). Having an indolent lymphoma, patients with gastric EMZBL-MALT have a relatively good prognosis and the 5-year survival rate was reported to be over 90% by some authors (1,10). This study was conducted to review local data on clinical features and treatment outcome in patients with this disease.
Materials and methods
This is a retrospective study of patients in Caritas Medical Center (CMC), a hospital serving mainly the Sham Shui Po district, Hong Kong Special Administration Region. The pathology database of CMC was searched for patients with the diagnosis of “MALT lymphoma” or “EMZBL-MALT” in stomach made between 1st July 1997 and 30th June 2009. Totally 30 subjects were included in this study. Clinical data were collected until the time of death (if applicable), the last date of attendance for those defaulted follow-up, or 30th June 2009, whichever came earlier. Diagnosis of EMZBL-MALT was made on the basis of histological and immunophenotypic analysis of gastric biopsies, and supplemented by molecular study using polymerase chain reaction to demonstrate clonal proliferation in equivocal cases. Helicobacter status (HP or H. Heilmanni), at time of diagnosis and after antibacterial therapy, was determined by histopathologic examination of gastric biopsies in all subjects. Subjects were staged according to the Lugano staging system (11) using clinical examination, endoscopy, chest X-ray, abdominal ultrasound or computerized tomography (CT) scan, bone marrow biopsy, endoscopic ultrasound and/or positron emission tomography (PET) scan.
Choice of treatment was mainly determined by subjects’ Helicobacter status. Those infected with Helicobacter were given a course of proton pump inhibitor (PPI)-based triple therapy for one week to eradicate the microbe as first-line therapy. Those, who were free of Helicobacter infection, were mainly treated with single-agent chemotherapy. In early phase of the study period, a few patients underwent gastrectomy, which was a prevalent treatment at that time, as first-line or second-line therapy. No subject received radiotherapy or Rituximab in this series. After initiation of treatment, oesophageogastroduodenoscopy (OGD) was performed periodically until endoscopic and histological remission. If there was persistent histological evidence of EMZBL-MALT, according to endoscopic appearance, any subsequent large cell transformation and patients’ preference, either a “wait-and-watch” approach with regular OGD monitoring or referral to other units for more aggressive treatment (e.g., combination chemotherapy or gastrectomy) would be made. All subjects were provided with long-term follow-up in CMC unless they were referred to oncology centers, defaulted follow-up or died. After disease remission, OGD would be arranged from time to time as surveillance and once suspicion of relapse was raised.
Statistical analysis was performed using SAS 9.1.3 software package. Overall survival was calculated from time of diagnosis to time of death of any cause or last follow-up. Survival curves were estimated by the method of Kaplan-Meier. P values of 0.05 or less were taken as statistically significant.
Results
Characteristics of patients
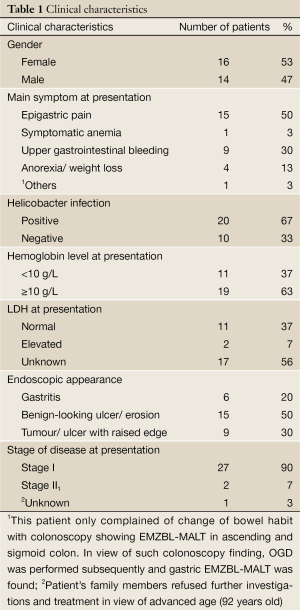
30 subjects with gastric EMZBL-MALT were included in this study. In all cases, gastric biopsies for initial diagnosis were obtained through OGD. The median follow-up time was 6.4 years (IQR 3.9 to 8.9 years). At time of diagnosis, median age was 71.5 years (IQR 64 to 81 years). Systemic B symptoms and beta-2-microglobulin level were not checked in most subjects and its significance could not be analyzed. Helicobacter was identified in 20 subjects (67%), including 19 HP infection and 1 H. Heilmanni infection. Of these 20 subjects, Helicobacter was missed in gastric biopsies from first OGD in 3 subjects, who were subsequently diagnosed to have Helicobacter infection in second OGD. Characteristics of patients are summarized in Table 1.
Full table
Treatment outcome
Only 29 patients received treatment and one patient, whose gastric biopsy did not demonstrate Helicobacter, refused any kind of treatment in view of advanced age (92 year old). This patient was still alive at the end of study period (4-year follow-up) and admitted to hospital twice in this period because of bleeding from the gastric tumour, which showed no significant interval enlargement in serial OGD examination.
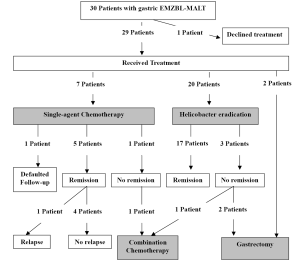
In this case series, two patients (one HP-positive and one HP-negative) underwent gastrectomy as first-line treatment while another two HP-positive patients underwent gastectomy for persistence of gastric EMZBL-MALT after Helicobacter eradication. These four patients were diagnosed to have disease in the era when surgery was still a prevalent treatment option for gastric lymphoma and all of them did not suffer from relapse of lymphoma afterwards. Treatment outcome for those receiving Helicobacter eradication or single-agent chemotherapy as first-line treatment would be discussed in detail in the following paragraphs. Different treatment modalities and outcome were summarized in Figure 1.
Helicobacter eradication
As first-line treatment for gastric EMZBL-MALT, PPI-based triple therapy was given to 20 subjects, whose gastric biopsies showed Helicobacter. For this group, median age was 71.5 years (IQR 54 to 81 years) and median follow-up time was 7.7 years (IQR 3.7 to 9 years). Disease remission happened within 6 months in fifteen subjects and within 15 months in another two subjects. Therefore, totally, Helicobacter eradication induced disease remission in seventeen Helicobacter-positive patients (85%). No relapse of disease was observed in these responders. Three subjects, with successful Helicobacter eradication, did not have endoscopic or histological improvement all along. They were referred out and finally, free from disease after either gastrectomy or combination chemotherapy.
Single-agent chemotherapy
Seven Helicobacter-free subjects received single-agent chemotherapy as first-line treatment. Cyclophosphamide was the choice in all cases. At time of diagnosis, median age was 72 years (IQR 67 to 85 years) and median follow-up time was 4 years (IQR 3.1 to 7 years). Disease remission was observed in five subjects (71%) while response could not be evaluated in one subject, who defaulted follow-up around 6 weeks after starting cyclophosphamide. One of the responders had local relapse 27 months after stopping cyclophosphamide. This subject was diagnosed to have hepatocellular carcinoma (HCC) in the same period and opted not for treatment for both diseases in view of advanced age (89 years old).
One subject, who had stage I disease initially, did not show any response to cyclophosphamide. She was subsequently referred to oncology centre for combination chemotherapy (CHOP regime) because of progressive tumour growth. She eventually died 46 months after initial diagnosis due to disease progression (stage IV disease before death).
Overall survival
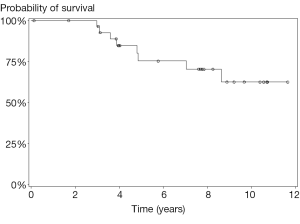
In this case series, eight patients passed away during the study period (mortality rate 27%) but only one of them died apparently from progression of gastric EMZBL-MALT as mentioned above. Causes of death in other subjects included acute coronary syndrome (three subjects), chest infection (two subjects), cholangiocarcinoma (one subject) and rupture HCC (one subject). The median age at death was 86 years (IQR 76 to 88 years). The overall survival rate was 75% (95% CI: 58% to 93%) at 5 years and 62.5% (95% CI: 40% to 85%) at 10 years after diagnosis (Figure 2).
Discussion
Two third of subjects (67%) had Helicobacter infection in this series. This figure was quite similar to that in a local study (12), which reported 62% of subjects were HP-positive using histopathologic examination. However, higher proportion of HP-positive subject was found in other Asian and Western series, ranging from 76% to 91% (4,10,13). This discrepancy could be partially explained by the reason that two or more methods were applied to detect HP in these series while in the present study, only histopathologic examination was used. The accuracy of histopathologic examination was affected by inter-observer variation and sampling error, especially in patients taking anti-secretory agents or antibiotics. In this study, Helicobacter infection was only found after subsequent but not initial OGD in 3 subjects, revealing that it was not uncommon to miss this microbe. Since Helicobacter status affects treatment option of gastric EMZBL-MALT significantly, it is advisable to consider additional non-invasive means of HP detection, like urea breath test or serology test, if HP is not identified in gastric biopsy.
We found that remission of gastric EMZBL-MALT was achieved after Helicobacter eradication in 85% of Helicobacter-positive subjects. This figure was comparable to the result of several reported large series from Western and Asian regions, ranging from 89-94% (1-5). Delayed histological regression of lymphoma after successful Helicobacter eradication is not uncommonly encountered in clinical practice. In this series, one subject, with early resolution of endoscopic abnormality, only achieved histological regression around 15 months after antibacterial treatment. Such delay was also described in different studies and could be more than 30 months (13). Hence, a wait-and-watch approach seems reasonable if there is persistent histological evidence of lymphoma in patients whose clinical and endoscopic manifestations improve after successful HP eradication. However there is no consensus on the period of observation before declaration of treatment failure. In this series, histological regression was found within 6 months in the majority of responders (15/17 or 88%). Wundish reported that histological regression rates at 3 months and 1 year were 61% and 88% respectively (1) while Hong found response rates of 78% and 93% at 6 months and 1 year respectively (2). In view of these findings, some authors suggested physicians to observe for at least one year after successful HP eradication before making conclusion of treatment failure (2,10,13).
In this series, there were eight mortality cases (mortality rate 27%) but gastric EMZBL-MALT was apparently the direct cause of death in one subject only. Lower mortality rates were reported in Pinotti’s and Nakamura’s series (11% and 8% respectively) (4,14), in both of which no subject died of disease progression. These observations were compatible with the indolent nature of this disease as well as the availability of effective treatment. Higher mortality rate in the present cohort could be related to larger proportion of elderly subjects, with a median age of 71.5 years at time of diagnosis (63 and 57 years respectively in Pinotti’s and Nakamura’s series). We estimated that the 5-year and 10-year survival rates were 75% and 62.5% respectively. Other authors reported better survival, with 5-year figure at around 90% and 10-year figure at around 80% (1,9,10). Similarly, age difference was likely the main reason for the discrepancy because in those series with more favorable result, the median age was lower (range, 53.5 to 64 years).
There were several limitations in this study. First of all, because of the retrospective nature of this study, there were lots of missing data in LDH level, beta-2 microglobulin level, systemic B symptoms and performance status, all of which were frequently included in other lymphoma studies. Secondly, as mentioned previously, lack of use of additional tests to detect HP in the present cohort led to underestimation of the proportion of HP-positive subjects. In addition, the endoscopic changes might be so subtle that endoscopists did not take biopsies accurately from abnormal sites. This sampling error would lead to over-diagnosis of disease remission. Mehra and Agarwal mentioned several methods to decrease sampling error including use of jumbo forcep, endoscopic mucosal resection and endoscopic ultrasound guidance for biopsy (15). Lastly, the small sample size limited the power of this study in determination of response rate of different treatment modalities and survival analysis.
Conclusions
This study supported the close association between HP infection and gastric EMZBL-MALT. At least one additional test for HP (such as urea breath test or serology test) is recommended in subjects whose gastric biopsy did not show HP. Helicobacter eradication and single-agent chemotherapy were effective treatment modalities for localized disease, inducing disease remission in 85% of HP-positive subjects and 71% of HP-negative subjects respectively. Prognosis was favorable, with 5-year and 10-year survival rates at 75% and 62.5% respectively.
Acknowledgements
Disclosure: The author declares no conflict of interest.
References
- Wündisch T, Thiede C, Morgner A, et al. Long-term follow-up of gastric MALT lymphoma after Helicobacter pylori eradication. J Clin Oncol 2005;23:8018-24.
- Hong SS, Jung HY, Choi KD, et al. A prospective analysis of low-grade gastric malt lymphoma after Helicobacter pylori eradication. Helicobacter 2006;11:569-73.
- Fischbach W, Goebeler ME, Ruskone-Fourmestraux A, et al. Most patients with minimal histological residuals of gastric MALT lymphoma after successful eradication of Helicobacter pylori can be managed safely by a watch and wait strategy: experience from a large international series. Gut 2007;56:1685-7.
- Nakamura T, Seto M, Tajika M, et al. Clinical features and prognosis of gastric MALT lymphoma with special reference to responsiveness to H. pylori eradication and API2-MALT1 status. Am J Gastroenterol 2008;103:62-70.
- Chung SJ, Kim JS, Kim H, et al. Long-term clinical outcome of helicobacter pylori-negative gastric mucosa-associated lymphoid tissue lymphoma is comparable to that of h. pylori-positive lymphoma. J Clin Gastroenterol 2009;43:312-7.
- Schechter NR, Portlock CS, Yahalom J. Treatment of mucosa-associated lymphoid tissue lymphoma of the stomach with radiation alone. J Clin Oncol 1998;16:1916-21.
- Park HC, Park W, Hahn JS, et al. Low grade MALT lymphoma of the stomach: treatment outcome with radiotherapy alone. Yonsei Med J 2002;43:601-6.
- Tsang RW, Gospodarowicz MK, Pintilie M, et al. Localized mucosa-associated lymphoid tissue lymphoma treated with radiation therapy has excellent clinical outcome. J Clin Oncol 2003;21:4157-64.
- Thieblemont C, Dumontet C, Bouafia F, et al. Outcome in relation to treatment modalities in 48 patients with localized gastric MALT lymphoma: a retrospective study of patients treated during 1976-2001. Leuk Lymphoma 2003;44:257-62.
- Stathis A, Chini C, Bertoni F, et al. Long-term outcome following Helicobacter pylori eradication in a retrospective study of 105 patients with localized gastric marginal zone B-cell lymphoma of MALT type. Ann Oncol 2009;20:1086-93.
- Rohatiner A, d’Amore F, Coiffier B, et al. Report on a workshop convened to discuss the pathological and staging classifications of gastrointestinal tract lymphoma. Ann Oncol 1994;5:397-400.
- Xu WS, Ho FC, Ho J, et al. Pathogenesis of gastric lymphoma: the enigma in Hong Kong. Ann Oncol 1997;8 Suppl 2:41-4.
- Lee SK, Lee YC, Chung JB, et al. Low grade gastric mucosa associated lymphoid tissue lymphoma: treatment strategies based on 10 year follow-up. World J Gastroenterol 2004;10:223-6.
- Pinotti G, Zucca E, Roggero E, et al. Clinical features, treatment and outcome in a series of 93 patients with low-grade gastric MALT lymphoma. Leuk Lymphoma 1997;26:527-37.
- Mehra M, Agarwal B. Endoscopic diagnosis and staging of mucosa-associated lymphoid tissue lymphoma. Curr Opin Gastroenterol 2008;24:623-6.