The frequency of histologically confirmed Barrett’s esophagus varies by the combination of ethnicity and gender
Introduction
The incidence of esophageal adenocarcinoma (EAC) has dramatically increased over the last several decades in the United States, primarily in males (1,2). Barrett’s esophagus (BE), the accepted metaplastic precursor of EAC, has an incidence rate highest in the non-Hispanic white (nHw) population (3). In addition, BE predominately affects men compared to women (3-6). Other risk factors for development of BE and EAC are gastroesophageal reflux disease (GERD), obesity, and tobacco smoking while H. pylori colonization and regular aspirin or non-steroidal anti-inflammatory drugs reduce risk (7-15).
The mechanisms for the disparity seen in BE and EAC incidence across ethnic and gender groups remain unclear. A common hypothesis regarding BE formation suggests that years of unrecognized GERD results in damage to the squamous esophageal mucosa secondary to acidic gastric contents resulting in a metaplastic change. Females with reflux symptoms have less esophageal acid exposure than males on average (16). However, females and males with BE had similar reflux severity (16). Conversely, data indicate that not all with BE have a history of reflux symptoms, nor do the majority of GERD patients develop BE (17). Interestingly, evaluations similar to the above between nHw and African American (AA) patients with reflux or BE has not occurred to date.
In addition, minimal information exists evaluating BE using the combination of race and gender specifically. Only a single study to date has assessed the impact of ethnicity and gender in combination as risk factors for BE (18). Unfortunately, one ethnic group studied by Ford and colleagues was a composite group called “Afro-Caribbean” rather than individuals of only African descent. We therefore decided to retrospectively assess the frequency of histologically confirmed BE to determine if the combination of ethnicity and gender impacts this outcome at an urban United States tertiary care facility that cares for a significant number of female and AA patients.
Methods
A single center retrospective study was performed by reviewing all upper endoscopies performed at the University of Florida College of Medicine-Jacksonville (UFCOM-Jacksonville) between September 2002 and August 2007. The study was approved by the UFCOM-Jacksonville Institutional Review Board. All patients, at least of 18 years of age with self-reported nHw or AA ethnicity, who underwent upper endoscopy (EGD) and found to have salmon colored esophageal mucosa endoscopically during the study period were eligible for inclusion. The appearance of the esophagogastric junction (EGJ), defined as the junction of the proximal gastric folds with the tubular esophagus was carefully noted to assess for the presence of an irregular z-line or salmon colored mucosa arising from the EGJ. Then, biopsies were performed on any tongues measuring at least 1 cm of salmon-colored mucosa arising from the EGJ suspicious for BE. In addition, four-quadrant biopsies were taken from all areas of suspected intestinal metaplasia every 1 cm of the length of the salmon colored mucosa. All EGDs were performed by six board-certified faculty attending gastroenterologists or gastroenterology fellows under direct supervision of faculty in the Division of Gastroenterology.
Exclusion criteria included patients who did not have specialized intestinal metaplasia on biopsy as well as insufficient or inconclusive biopsies. Histologic BE was diagnosed only if endoscopy revealed salmon colored mucosa at least 1 cm above the top of the gastric folds and intestinal metaplasia with goblet cells identified by hematoxylin-eosin and confirmed by Alcian blue on biopsy. Long-segment BE (LSBE) was defined as ≥3 cm of salmon colored mucosa on endoscopy and histologic confirmation as described above. Short-segment BE (SSBE) was defined as 1–3 cm of salmon colored mucosa on endoscopy and histologic confirmation as described above. If salmon colored mucosa was observed measuring at least 1 cm but an overall length not recorded with histologic confirmation described above, those individuals were classified as SSBE.
Data collected for all patients with histologic BE included age at diagnosis, gender, ethnicity, previous history of gastroesophageal reflux, atypical symptoms (chronic cough, aspiration, chest pain), cigarette smoking (by patient report), alcohol use (by patient report), body mass index (BMI), proton pump inhibitor (PPI) use, endoscopic length of BE, presence or absence of hiatal hernia, stricture or ulcer, presence or absence of dysplasia, and if present the grade of dysplasia.
Statistical analysis
Continuous data were compared using two sided Student t tests or ANOVA for normally distributed continuous data. Categorical data were analyzed using appropriate chi-square testing. Prevalence was recorded as a percent of the total group and for each ethnicity. Logistic regression modeling was also performed using male sex and nHw race as the basis of comparison to derive odds ratios of histologic BE. Differences between groups were considered significant if P<0.05. Data analysis was performed using the IBM SPSS statistics statistical analysis program (version 22, IBM Corporation, Armonk, NY, USA).
Results
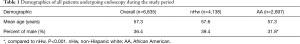
During the 5-year period between September 1, 2002 and August 31, 2007, a total of 11,163 EGDs were performed on 7,308 total patients. Of this amount, 6,835 patients were self-identified as either nHw [4,138] or AA [2,697] ethnicity and eligible for the investigation. Demographic information of the overall population as well as nHw and AA groups are listed in Table 1. Mean patient age of those undergoing endoscopy was 57.3 years and 36% of the overall patient population were male. No difference was seen in mean age between the overall population and either ethnic group studied. AA had fewer males undergoing EGD compared to nHw during the study interval (P<0.001, Table 1).
Full table
A total of 456 EGDs with salmon colored esophageal mucosa were retrieved from the endoscopic database, corresponding to 391 patients with findings suggestive of BE on EGD (5.4% of the population undergoing EGD during the study period). The ethnic distribution of patients with salmon colored esophageal mucosa was as follows: 306 (76%) nHw and 85 (21%), AA. Histologically confirmed BE was present in 111 patients (1.5% of the population undergoing EGD during the study interval, 28.4% of patients with salmon colored esophageal mucosa); 95 (83%) were nHw while 16 (14%) were AA. A summary of the demographic and clinical information of the histologic BE group overall as well as by ethnicity is seen in Table 2. Mean age was similar between both groups with histologically confirmed BE. A higher proportion of nHw and AA males than females had histologically confirmed BE (Table 2). However the gender variation observed between the two ethnic groups did not reach significance.

Full table
The frequency of histologic confirmation of BE varied by the combination of gender and ethnicity (Table 3). The difference observed in the frequency of histologic BE was significant between nHw men compared to either nHw or AA females, P<0.005. Although AA men had a reduced frequency of histologic confirmation compared to nHw men, this variation did not achieve significance. Odds ratios for histologic confirmation based on ethnicity and gender are also indicated in Table 3. Compared to nHw males (reference), all combinations of ethnicity and gender were less likely to have histologic confirmation of BE with odds ratios for both nHw and AA females reaching significance [nHw females 0.327 (95% CI, 0.195 to 0.547); AA females 0.191 (95% CI, 0.081 to 0.448)].

Full table
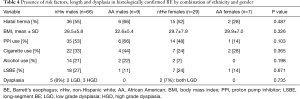
Comparison of risk factors and dysplasia presence by the combination of ethnicity and gender are indicated in Table 4. Interestingly, in spite of the histologic confirmation frequency differences seen above, no variation was observed in the presence of common risk factors for BE between ethnic and gender combinations. This also occurred assessing dysplasia presence by the same parameters.
Full table
Discussion
Minimal data exists on the prevalence of BE when considering the combination of gender and ethnicity in the United States. The aim of this investigation was to determine whether the frequency of histologically confirmed BE varies by both ethnicity and gender at an urban United States tertiary care facility caring for a significant number of female and AA patients. In this retrospective study of BE at such a center, the frequency of histologically confirmed BE varies by the combination of gender and ethnicity. nHw males had the highest frequency of histologically confirmed BE while AA females had the lowest.
Several groups have evaluated histologically confirmed BE by gender in multiethnic populations (3,6,17-23). However, only three of the investigations report prevalence in detail using ethnicity and gender as measurable variables (6,17,23). AA and nHw were the only groups evaluated or the two largest ethnic populations assessed in these studies (6,17,23). Khoury and associates indicated that AA and females had a lower prevalence than nHw and males, respectively, of histologically confirmed BE (6). Fan and Snyder reported that the rate of histologically conformed BE in males was significantly higher than females irrespective of GERD symptoms (17). Interestingly, Fan and Snyder did not discover a significant difference in confirmed BE prevalence between nHw, AA, and Hispanic Americans (17). In a recent assessment of BE risk factors between AA and nHw at a large Veterans Affairs Medical Center, AA prevalence was lower than nHw and not accounted for by risk factor differences between groups (23). Males comprised more than 90% of individuals as expected from investigations from the Veterans Affairs system while our AA group was comprised of 44% females allowing for assessment by gender. In our cohort, no difference was seen in the presence of hiatal hernia, BMI, as well as PPI, cigarette and alcohol use across ethnic/gender combinations confirming the previous results while adding assessment of a female component, missing previously, to the BE literature.
Sex hormones, in combination with obesity, may be responsible for the disparities seen in BE and EAC by gender and ethnicity (3,8,9,24-27). Theories regarding the impact of these hormones consist of either estrogen protection, androgen carcinogenic effect and/or consequences of alterations in the ratio of androgen to estrogen. At present, two studies have assessed circulating sex hormones in either BE or EAC (28,29). Awan and colleagues performed a small case control investigation assessing serum testosterone in male EAC patients compared to age matched benign surgical controls (28). Preoperative serum testosterone was significantly higher in the EAC group compared with those having benign surgery. Cook et al. evaluated, in case control fashion, circulating sex hormones in men with BE versus matched endoscopic controls (29). Elevated free testosterone and dihydrotestosterone were positively associated with BE risk while elevated estrone sulfate was associated with reduced risk. Regrettably, both investigations did not evaluate women or report on ethnic differences in serum sex hormone levels among men. Assessment of sex hormones by the combination of ethnicity and gender in those suspected to have BE endoscopically as well as those with histologic confirmation of BE may provide further evidence explaining the findings of the present investigation.
There are limitations to the present study that should be mentioned. Rates of H. pylori colonization were not included as such data was not available for all cases. H. pylori colonization is associated with a decreased risk of BE (30). The prevalence of H. pylori is higher among AA compared to nHw and this factor may contribute to the observed differences in BE seen among ethnic groups (31). In addition, males are known to have higher rates of H. pylori colonization than females after controlling for the influence of race/ethnicity (32). The number of males in the AA group undergoing endoscopy was significantly less than observed in the nHw group in the present investigation. It is well known that males, especially AA males, have decreased health seeking behavior as well as significant medical mistrust, which can contribute to the diminished frequency observed (33). Individual statin and aspirin use was not recorded for all subjects. Both statin and aspirin use have been associated with reduced risk of BE formation (34). Recent data indicate that AA men and all races/ethnicities of women are less likely to report use of these drugs (35). This finding suggests that the decreased rate of histologically confirmed BE observed presently in AA men as well as AA/nHw females could be even further reduced if use of those agents was recorded and found to be equal between groups. The present study was a single center retrospective evaluation, which could reduce the generalizability of our findings in other patient populations. Finally, the small number of AA with biopsy proven BE in our investigation limits the impact of any observations noted and warrants confirmation in larger studies.
To conclude, histologically confirmed BE frequency varies by ethnicity and gender with nHw males having the highest frequency/risk and AA females the lowest. Investigation to improve understanding of the impact of ethnicity and gender in BE formation should be performed including assessment of sex hormones, wound healing and H. pylori infection on those at risk or currently with the disease.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This research was approved by the University of Florida College of Medicine-Jacksonville Institutional Review Board (No. UFJ 2007-150).
References
- Thrift AP, Whiteman DC. The incidence of esophageal adenocarcinoma continues to rise: analysis of period and birth cohort effects on recent trends. Ann Oncol 2012;23:3155-62. [Crossref] [PubMed]
- Cook MB, Chow WH, Devesa SS. Oesophageal cancer incidence in the United States by race, sex, and histologic type, 1977-2005. Br J Cancer 2009;101:855-9. [Crossref] [PubMed]
- Cook MB, Wild CP, Forman D. A systematic review and meta-analysis of the sex ratio for Barrett's esophagus, erosive reflux disease, and nonerosive reflux disease. Am J Epidemiol 2005;162:1050-61. [Crossref] [PubMed]
- Ronkainen J, Aro P, Storskrubb T, et al. Prevalence of Barrett's esophagus in the general population: an endoscopic study. Gastroenterology 2005;129:1825-31. [Crossref] [PubMed]
- Edelstein ZR, Bronner MP, Rosen SN, et al. Risk factors for Barrett's esophagus among patients with gastroesophageal reflux disease: a community clinic-based case-control study. Am J Gastroenterol 2009;104:834-42. [Crossref] [PubMed]
- Khoury JE, Chisholm S, Jamal MM, et al. African Americans with Barrett's esophagus are less likely to have dysplasia at biopsy. Dig Dis Sci 2012;57:419-23. [Crossref] [PubMed]
- Lagergren J, Bergström R, Lindgren A, et al. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med 1999;340:825-31. [Crossref] [PubMed]
- Hoyo C, Cook MB, Kamangar F, et al. Body mass index in relation to oesophageal and oesophagogastric junction adenocarcinomas: a pooled analysis from the International BEACON Consortium. Int J Epidemiol 2012;41:1706-18. [Crossref] [PubMed]
- Kubo A, Cook MB, Shaheen NJ, et al. Sex-specific associations between body mass index, waist circumference and the risk of Barrett's oesophagus: a pooled analysis from the international BEACON consortium. Gut 2013;62:1684-91. [Crossref] [PubMed]
- Cook MB, Kamangar F, Whiteman DC, et al. Cigarette smoking and adenocarcinomas of the esophagus and esophagogastric junction: a pooled analysis from the international BEACON consortium. J Natl Cancer Inst 2010;102:1344-53. [Crossref] [PubMed]
- Cook MB, Shaheen NJ, Anderson LA, et al. Cigarette smoking increases risk of Barrett's esophagus: an analysis of the Barrett's and Esophageal Adenocarcinoma Consortium. Gastroenterology 2012;142:744-53. [Crossref] [PubMed]
- Liao LM, Vaughan TL, Corley DA, et al. Nonsteroidal anti-inflammatory drug use reduces risk of adenocarcinomas of the esophagus and esophagogastric junction in a pooled analysis. Gastroenterology 2012;142:442-452.e5; quiz e22-3.
- Anderson LA, Johnston BT, Watson RG, et al. Nonsteroidal anti-inflammatory drugs and the esophageal inflammation-metaplasia-adenocarcinoma sequence. Cancer Res 2006;66:4975-82. [Crossref] [PubMed]
- Whiteman DC, Parmar P, Fahey P, et al. Association of Helicobacter pylori infection with reduced risk for esophageal cancer is independent of environmental and genetic modifiers. Gastroenterology 2010;139:73-83; quiz e11-2.
- Thrift AP, Pandeya N, Smith KJ, et al. Helicobacter pylori infection and the risks of Barrett's oesophagus: a population-based case-control study. Int J Cancer 2012;130:2407-16. [Crossref] [PubMed]
- Banki F, Demeester SR, Mason RJ, et al. Barrett's esophagus in females: a comparative analysis of risk factors in females and males. Am J Gastroenterol 2005;100:560-7. [Crossref] [PubMed]
- Fan X, Snyder N. Prevalence of Barrett's esophagus in patients with or without GERD symptoms: role of race, age, and gender. Dig Dis Sci 2009;54:572-7. [Crossref] [PubMed]
- Ford AC, Forman D, Reynolds PD, et al. Ethnicity, gender, and socioeconomic status as risk factors for esophagitis and Barrett's esophagus. Am J Epidemiol 2005;162:454-60. [Crossref] [PubMed]
- Abrams JA, Fields S, Lightdale CJ, et al. Racial and ethnic disparities in the prevalence of Barrett's esophagus among patients who undergo upper endoscopy. Clin Gastroenterol Hepatol 2008;6:30-4. [Crossref] [PubMed]
- Wang A, Mattek NC, Holub JL, et al. Prevalence of complicated gastroesophageal reflux disease and Barrett's esophagus among racial groups in a multi-center consortium. Dig Dis Sci 2009;54:964-71. [Crossref] [PubMed]
- Corley DA, Kubo A, Levin TR, et al. Race, ethnicity, sex and temporal differences in Barrett's oesophagus diagnosis: a large community-based study, 1994-2006. Gut 2009;58:182-8. [Crossref] [PubMed]
- Balasubramanian G, Singh M, Gupta N, et al. Prevalence and predictors of columnar lined esophagus in gastroesophageal reflux disease (GERD) patients undergoing upper endoscopy. Am J Gastroenterol 2012;107:1655-61. [Crossref] [PubMed]
- Nguyen TH, Thrift AP, Ramsey D, et al. Risk factors for Barrett's esophagus compared between African Americans and non-Hispanic Whites. Am J Gastroenterol 2014;109:1870-80. [Crossref] [PubMed]
- Cook MB, Dawsey SM, Freedman ND, et al. Sex disparities in cancer incidence by period and age. Cancer Epidemiol Biomarkers Prev 2009;18:1174-82. [Crossref] [PubMed]
- Löfdahl HE, Lu Y, Lagergren J. Sex-specific risk factor profile in oesophageal adenocarcinoma. Br J Cancer 2008;99:1506-10. [Crossref] [PubMed]
- Chandanos E, Lagergren J. The mystery of male dominance in oesophageal cancer and the potential protective role of oestrogen. Eur J Cancer 2009;45:3149-55. [Crossref] [PubMed]
- Cronin-Fenton DP, Murray LJ, Whiteman DC, et al. Reproductive and sex hormonal factors and oesophageal and gastric junction adenocarcinoma: a pooled analysis. Eur J Cancer 2010;46:2067-76. [Crossref] [PubMed]
- Awan AK, Iftikhar SY, Morris TM, et al. Androgen receptors may act in a paracrine manner to regulate oesophageal adenocarcinoma growth. Eur J Surg Oncol 2007;33:561-8. [Crossref] [PubMed]
- Cook MB, Wood SN, Cash BD, et al. Association between circulating levels of sex steroid hormones and Barrett's esophagus in men: a case-control analysis. Clin Gastroenterol Hepatol 2015;13:673-82. [Crossref] [PubMed]
- Fischbach LA, Nordenstedt H, Kramer JR, et al. The association between Barrett's esophagus and Helicobacter pylori infection: a meta-analysis. Helicobacter 2012;17:163-75. [Crossref] [PubMed]
- Epplein M, Signorello LB, Zheng W, et al. Race, African ancestry, and Helicobacter pylori infection in a low-income United States population. Cancer Epidemiol Biomarkers Prev 2011;20:826-34. [Crossref] [PubMed]
- Replogle ML, Glaser SL, Hiatt RA, et al. Biologic sex as a risk factor for Helicobacter pylori infection in healthy young adults. Am J Epidemiol 1995;142:856-63. [Crossref] [PubMed]
- Cheatham CT, Barksdale DJ, Rodgers SG. Barriers to health care and health-seeking behaviors faced by Black men. J Am Acad Nurse Pract 2008;20:555-62. [Crossref] [PubMed]
- Goldberg A, Gerkin RD, Young M. Medical Prevention of Barrett's Esophagus: Effects of Statins, Aspirin, Non-aspirin NSAIDs, Calcium, and Multivitamins. Dig Dis Sci 2015;60:2058-62. [Crossref] [PubMed]
- Johansen ME, Hefner JL, Foraker RE. Antiplatelet and Statin Use in US Patients With Coronary Artery Disease Categorized by Race/Ethnicity and Gender, 2003 to 2012. Am J Cardiol 2015;115:1507-12. [Crossref] [PubMed]


