Tumor stage in patients operated for rectal cancer: a comparison of the pre-operative MR and the resection specimen, with specific attention to the effect of neo-adjuvant radiotherapy
Introduction
Colorectal cancer is one of the most occurring malignancies in the western world (1,2). Surgery is the only curative option, with risk of (local) recurrence being a large concern as it is responsible for significant morbidity and mortality (3).
Patients presenting with rectal cancer undergo radiologic staging at the time of diagnosis to determine the extent of disease in order to decide on optimal treatment. The tumor/node/metastasis (TNM) system is used to describe numerically the anatomical extent of cancer (4). Magnetic resonance (MR) tomography and, to a lesser extent, endorectal ultrasound in addition to endoscopy are used to evaluate the extent of the primary tumor in relation to the mesorectal fascia, and the invasion of surrounding lymph nodes pre-operatively (5,6). These examinations help determine the optimal surgical approach, and the need for neo-adjuvant radiotherapy and chemotherapy (CRT).
In daily practice, it appeared that the post-operative tumor stage, as determined by the histological examination of the resection specimen (the only true gold standard), can differ from the pre-operative staging. Is this an effect of down-staging as a result of CRT or simply a misinterpretation of MR?
A study by Akasu et al. shows the MR to be highly accurate in patients undergoing resection without neo-adjuvant CRT for predicting T-stage, though only moderately effective in detecting lymph node metastases (6). Down staging could result in the need for less invasive surgery and thus reduced peri-operative morbidity without harming prognosis (7,8). However, the role of restaging through MR after CRT is controversial as the diagnostic accuracy is low, presumably due to reactive changes after therapy that are hard to distinguish from residual tumor (9).
A study was done in normal daily practice, in patients with rectal cancer who underwent curative surgery. The purpose was evaluated the preoperative TN stage with MR and the postoperative stage with the histological investigation of the resection specimen. The findings were correlated with the application of neo-adjuvant therapy.
Methods
All consecutive patients diagnosed with rectal cancer in the period 2002–2015 in the Zaans Medical Centre, the community hospital of the Zaanstreek region in the Netherlands, were included. An extensive chart review was done in order to obtain data on pre-operative work-up, neo-adjuvant treatment, surgery and post-operative examination of the resection specimen.
Only patients in whom a pre-operative MR was done were included in the present study. In the first years of the study period the circumferential margin was not described in the routine MR. For this reason, the circumferential margin was not scored in the present study. Pathology reports were evaluated for the correct post-operative tumor stage.
Down staging was defined as a lower disease stage and lower T- and/or N-stage in the resection specimen compared with the pre-operative MR. Upgrading (“progression”) was defined as a higher disease stage and T- and/or N-stage in the resection specimen as determined by the pre-operative MR.
Statistical analysis was done with chi-square testing for contingency tables. A value below 0.05 was considered statistical significant.
The study was approved by the ethical committee of the Zaans Medisch Centrum.
Results
In the study period a total of 343 patients were diagnosed with rectal cancer. Of these 67.6% underwent surgical resection. The remainder already had metastatic disease (stage 4), rendering surgery futile or were in a very poor clinical condition due to co-morbidity.
From 176 patients (75.8%) a pre-operative MR was available for evaluation. One hundred forty-two patients (80.7%) underwent neo-adjuvant treatment, the remainder 19.3% underwent immediate surgery.
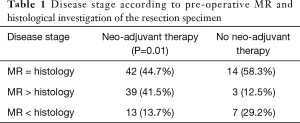
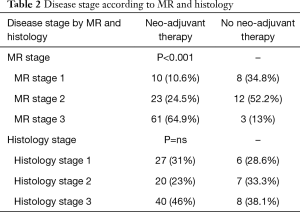
Neo-adjuvant therapy resulted in significant down staging as shown in Table 1. However, despite the neo-adjuvant treatment almost 14% of patients had a higher TN stage as determined by the pre-operative MR. In patients who underwent surgery without neo-adjuvant therapy the percentage with “progression” was almost 30%. Down staging also occurred, however, only in three patients. Table 2 shows the different tumor stages in both groups of patients. As to be expected the number of patients with stage 1 and 2 were higher in the group not treated with neo-adjuvant therapy. There was no significant difference in definite tumor stage as determined by histological examination of the resection specimen.
Full table
Full table
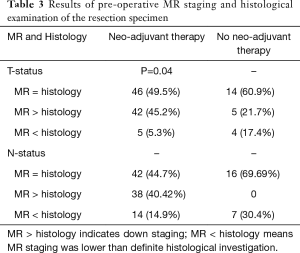
Table 3 shows the results of comparison of pre-operative MR-staging and histological examination of the resection specimen.
Full table
In 7 patients, no viable tumor was present anymore in the surgical resection specimen after neo-adjuvant therapy. This was not the case in any one of the patients who underwent immediate surgery.
Discussion
The work-up and treatment of rectal cancer has changed in the past decennium. Especially since the results of neo-adjuvant radiotherapy on recurrence and overall survival has been published (10). Short term radiotherapy followed by resection is the mainstay of treatment. Whether a long or short waiting period after radiotherapy is necessary still is a matter of debate (11,12). In the cohort diagnosed and treated in the Zaans Medisch Centrum, a longer waiting period results in a better outcome (13).
The present study is part of a much larger study on disease free survival, recurrence, and co-morbidity in patients with colorectal cancer (14). The study population of patients with rectal cancer was extended with all patients diagnosed in the period 2009–2015.
The majority of cases were discussed in a multi-disciplinary meeting of gastroenterologists, oncologists, surgeons, radiotherapists, radiologists, and pathologists. On basis of all available data the best treatment for the patient was chosen.
In the present study, a number of patients did not receive neo-adjuvant radiotherapy, mostly due to the low tumor stage as assessed by the pre-operative MR. This presented the unique opportunity to study the pre-operative staging using MR in comparison with the definite resection specimen as gold standard.
There are several MR parameters required to optimize staging of rectal cancer. Important aspects are the circumferential resection margin, extramural vascular invasion, and lymphnodes (15). In the present study, the TN stage was specifically noted.
In the literature, several studies have been published on the accuracy of pre-operative MR of the pelvic region. Overestimation as well as underestimation of the TN stage has been reported. Halefoglu et al. report a diagnostic accuracy of 75% for T-stage and 62.4% for N stage. Moriones et al. report similar findings with an accuracy of 72% and 60% respectively (16,17).
The goal of radiotherapy is down-staging and down-sizing the tumor. It allows for less extensive surgical resections and reduces the risk of local recurrence (18-20). Yang et al. studied the significance of tumor volume and its change after concurrent CRT. The TN stage was down staged in 60% of patients, including 23.3% with complete responses. All tumors showed volume reduction (21).
As to be hoped and expected, the present study showed significant down staging of neo-adjuvant therapy. However, MR underestimated the T/N stage in a number of patients. The final histological examination did not show a difference between both groups of patients. This indirectly indicates important down staging.
In conclusion, the present study shows significant down staging as a result of neo-adjuvant therapy. However, a higher tumor stage was present in 13.8% of patients despite the neo-adjuvant radiotherapy. Given the normal biological character of cancer this can be expected. Tumors grow and spread towards lymph nodes.
The diagnostic accuracy of the MR is not perfect. This could be cause for concern as earlier reports of diagnostic accuracy could be an overestimation of daily practice due to the expertise of participating radiologists. Underestimation as well as overestimation of the tumor occurred both in the patients treated with radiotherapy as well as those who underwent immediate operation. As such, MR results should be interpreted with caution when devising a treatment strategy. Nevertheless, the beneficial effect of radiotherapy is irrefutable with some patients even showing complete pathologic response.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical statement: The study was approved by ethical committee of the Zaans Medisch Centrum.
References
- Ferlay J, Steliarova-Foucher E, Lortet-Tieulent J, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries in 2012. Eur J Cancer 2013;49:1374-403. [Crossref] [PubMed]
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- Räsänen M, Carpelan-Holmström M, Mustonen H, et al. Pattern of rectal cancer recurrence after curative surgery. Int J Colorectal Dis 2015;30:775-85. [Crossref] [PubMed]
- Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010;17:1471-4.
- Bipat S, Glas AS, Slors FJ, et al. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging—a meta-analysis. Radiology 2004;232:773-83. [Crossref] [PubMed]
- Akasu T, Iinuma G, Takawa M, et al. Accuracy of high-resolution magnetic resonance imaging in preoperative staging of rectal cancer. Ann Surg Oncol 2009;16:2787-94. [Crossref] [PubMed]
- Kennelly RP, Heeney A, White A, et al. A prospective analysis of patient outcome following treatment of T3 rectal cancer with neo-adjuvant chemoradiotherapy and transanal excision. Int J Colorectal Dis 2012;27:759-64. [Crossref] [PubMed]
- Smith FM, Waldron D, Winter DC. Rectum-conserving surgery in the era of chemoradiotherapy. Br J Surg 2010;97:1752-64. [Crossref] [PubMed]
- Hanly AM, Ryan EM, Rogers AC, et al. Multicenter evaluation of rectal cancer reImaging post neoadjuvant (MERRION) therapy. Ann Surg 2014;259:723-7. [Crossref] [PubMed]
- van Gijn W, Marijnen CA, Nagtegaal ID, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 2011;12:575-82. [Crossref] [PubMed]
- Zhou ZR, Liu SX, Zhang TS, et al. Short-course preoperative radiotherapy with immediate surgery versus long-course chemoradiation with delayed surgery in the treatment of rectal cancer: a systematic review and meta-analysis. Surg Oncol 2014;23:211-21. [Crossref] [PubMed]
- Sajid MS, Siddiqui MR, Kianifard B, et al. Short-course versus long-course neoadjuvant radiotherapy for lower rectal cancer: a systematic review. Ir J Med Sci 2010;179:165-71. [Crossref] [PubMed]
- van Eeghen EE, den Boer F, Bakker SD, et al. Outcome of rectal cancer after radiotherapy with a long or short waiting period before surgery, a descriptive clinical study. J Gastrointest Oncol 2016;7:321-5. [Crossref] [PubMed]
- van Eeghen EE, Bakker SD, van Bochove A, et al. Impact of age and comorbidity on survival in colorectal cancer. J Gastrointest Oncol 2015;6:605-12. [PubMed]
- Dewhurst CE, Mortele KJ. Magnetic resonance imaging of rectal cancer. Radiol Clin North Am 2013;51:121-31. [Crossref] [PubMed]
- Moriones AB, Unzué JZ, Oroz LI, et al. Preoperative staging MRI for rectal cancer and pathologic correlation. An Sist Sanit Navar 2011;34:167-74. [PubMed]
- Halefoglu AM, Atasoy ST, Sakiz D, et al. Accuracy of thin-section magnetic resonance imaging with a pelvic phased-array coil in the local staging of rectal cancer. J Comput Assist Tomogr 2013;37:58-64. [Crossref] [PubMed]
- Nilsson S, Norlén BJ, Widmark A. A systematic overview of radiation therapy effects in prostate cancer. Acta Oncol 2004;43:316-81. [Crossref] [PubMed]
- Glimelius B, Holm T, Blomqvist L. Chemotherapy in addition to preoperative radiotherapy in locally advanced rectal cancer—a systematic overview. Rev Recent Clin Trials 2008;3:204-11. [Crossref] [PubMed]
- Pettersson D, Lörinc E, Holm T, et al. Tumour regression in the randomized Stockholm III Trial of radiotherapy regimens for rectal cancer. Br J Surg 2015;102:972-8; discussion 978. [Crossref] [PubMed]
- Yang SH, Lee RC, Chen CC, et al. Is decrease of tumor volume correlated with stage change after preoperative concurrent chemoradiotherapy? Hepatogastroenterology 2005;52:765-9. [PubMed]


