Complete response and prolonged disease-free survival in a patient with recurrent duodenal adenocarcinoma treated with bevacizumab plus FOLFOX6
Background
Adenocarcinoma of the small bowel is relatively rare malignancy which carries a poor prognosis. The American Cancer Society estimated 6,960 new cases of small intestinal cancer diagnosed in the year 2010 (1). According to the National Cancer Data Base, adenocarcinoma represented 36.9% of all patients with small bowel malignancies (2). Despite recent technical advances in imaging and endoscopy (3), delays in diagnosis is common and the majority (58%) of patients present with advanced Stage III or IV disease (2). Small bowel adenocarcinoma (SBA) also has the poorest prognosis among small bowel cancer histologies, with relative five-year observed survival rate of 32.5%, compared to 39.9% for stromal tumors, 49.6% for lymphomas and 64.6% for carcinoids. The median survival and 5-year disease specific survival (DSS) rates of patients with stage IV or recurrent disease are 9 months and 4.2%, respectively. For patients with stage III disease, median survival is 29.8 months and 5-year survival rate is only 35.4% (4). In addition, 5-year DSS is worse for patients with duodenal adenocarcinoma (28.2%) compared to those with jejunal (37.6%) or ileal (37.8%) primaries. Poorly differentiated tumors also carry a worse prognosis with median survival times of 11.1 months compared to 28.6 months for those with well-differentiated tumors. Literature regarding treatment options in the adjuvant and metastatic setting for small bowel adenocarcinoma is limited. There is an urgent need to evaluate novel strategies to treat these rare malignancies. We hereby report the case of our patient with recurrent duodenal adenocarcinoma with a disease-free survival of more than five years after treatment with chemotherapy and an antiangiogenic agent, bevacizumab.
Case report
An otherwise healthy 45-year-old man presented with significant abdominal bloating and tarry stools and was found to have a mass in the third portion of the duodenum. Computed tomography (CT) scan revealed concentric wall thickening of the distal duodenum and a mildly enlarged aortocaval lymph node. A Whipple procedure was performed and identified a tumor in the third portion of the duodenum. Pathologic examination of the 2.5 cm duodenal mass revealed a moderately to poorly differentiated duodenal adenocarcinoma with focal signet ring features. Metastatic carcinoma was found in three of five periduodenal lymph nodes and one omental implant.
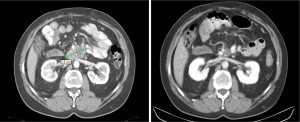
Six weeks following surgery, the patient was started on adjuvant chemotherapy with modified FOLFOX6 for eight doses followed by consolidative chemoradiation. Thirty months following surgery, he developed a local recurrence. CT imaging revealed a soft tissue mass, measuring 4.2 cm × 2.4 cm anterior to the left renal vein and immediately posterior to the superior mesenteric artery. His CEA level was elevated at 16.3 and treatment was started with FOLFOX6 and Bevacizumab with subsequent reduction of the tumor size to 2.4 cm × 1.8 cm after three months (Figure 1). After 12 doses of FOLFOX6, positron emission tomography (PET) showed a residual area without increased FDG uptake, corresponding to the tumor seen on imaging. The patient’s chemotherapy was switched to capecitabine and bevacizumab due to oxaliplatin-related neuropathy. Maintenance chemotherapy was given over a duration of two years after he achieved a complete radiologic and PET response to therapy. The patient continues to be disease-free 8 years since his recurrence.
Discussion
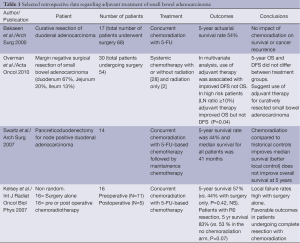
Currently, there is no consensus as to the benefit of, and the optimal regimen for, adjuvant therapy for patients with small bowel adenocarcinoma. The rarity of the disease has limited the ability to carry out prospective clinical trials and the optimal regimen remains undefined. Retrospective studies reported no significant survival advantage for patients who received adjuvant chemotherapy after resection of their primary tumors (5-7). In fact, patients who received adjuvant radiotherapy had shorter median survival times at 21.6 months compared to 49.9 months for those who did not (6). However, a multivariate analysis of one of these retrospective studies demonstrated that the use of adjuvant chemotherapy improved disease-free survival, and in patients considered “high risk” (lymph node ratio ≥10%), adjuvant therapy appear to improve survival (7). Despite a lack of clear evidence supporting its use, the National Cancer Data Base [1985-2005] reported an increase in the use of adjuvant chemotherapy from 8.1% in 1985 to 22.5% in 2005 (2). Chemotherapeutic regimens have included 5-FU or capecitabine with or without a platinum compound, such as oxaliplatin (7). Some of these retrospective data are summarized in Table 1.
Full table
Two years after his last adjuvant chemotherapy, our patient had a radiographic recurrence of duodenal adenocarcinoma with a concurrent rise in his CEA. He then displayed a complete radiographic response to systemic chemotherapy using FOLFOX6 and bevacizumab, followed by maintenance capecitabine and bevacizumab for a period of two years. Remarkably, he continues to be disease-free eight years after his recurrence.
For patients with unresected or metastatic SBA, there was a significant improvement in overall survival with systemic therapy compared to those who received no therapy (12 vs. 2 months; P=0.02) based on the MD Anderson retrospective study (5). Older fluoropyrimidine-based regimens, such as 5FU, doxorubicin with mitomycin yielded a disappointing 18% response rate and an 8-month median survival (8). Two of the 38 evaluable patients had complete radiologic responses. More recently, oxaliplatin plus capecitabine produced a 50% response rate (3 complete responses) with a 20.4-month median survival among 31 patients with small bowel and ampullary adenocarcinomas (9). Excluding the patients with ampullary tumors, response rate was 61% for the 18 patients with SBA. Further support for the use of oxaliplatin-based regimen in SBA arose from a retrospective French multicenter study (10). FOLFOX was associated with a 34% response rate, median progression-free survival of 6.9 months and median OS of 17.8 months. Thus, oxaliplatin-based chemotherapy has been suggested as a new standard for the treatment of metastatic or recurrent SBA (Table 2).

Full table
This is the first case report of bevacizumab used both with first-line FOLFOX, and with maintenance capecitabine, in a patient with SBA resulting in a complete radiologic response and prolonged progression-free survival 8 years after his recurrence. Vascular endothelial growth factor A (VEGF-A) overexpression was observed in 91% of SBA (11). Bevacizumab is an anti-VEGF monoclonal antibody with proven efficacy in the treatment of metastatic colorectal cancer (12). Although the mechanism of its efficacy has not been elucidated, results indicate that it renders cancer cells more sensitive to cytotoxic chemotherapy (13). Malignant epithelial cells of the gastrointestinal tract including small bowel adenocarcinoma express VEGF mRNA strongly, in contrast to normal epithelium, hyperplastic polyps, and adenomas (14). A recent study of 54 patients with small bowel adenocarcinoma confirmed this finding. 50 (91%) of these patients’ tissue displayed expression of VEGF-A, with high levels of its expression observed in 44 (81%) patients (11). Thus, there is basic science evidence to suggest that bevacizumab may be effective in SBA. Clinical success with bevacizumab in SBA was reported in 2008 by Tsang et al. (15). A 68-year-old with advanced adenocarcinoma of the jejunum received 8 cycles of gemcitabine and bevacizumab with regression of disease as measured by PET one year after presentation.
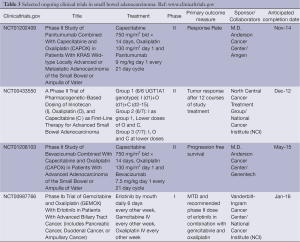
In treating this patient’s recurrence, we hypothesized that bevacizumab would give added efficacy to the standard cytotoxic chemotherapy regimen. As noted above, MDACC’s prospective study’s success with capecitabine and oxaliplatin for advanced adenocarcinoma of the small bowel included 10% of patients who achieved a complete radiographic response. Because the chemotherapeutic regimens used for this patient’s recurrence also included FOLFOX (which includes oxaliplatin) and, later, capecitabine, it is difficult to ascertain the contribution of bevacizumab to his excellent response. Nonetheless, we present these findings to propose that bevacizumab does warrant further study for treatment of SBA. Table 3 lists current studies for patients with SBA, including one study from MD Anderson utilizing bevacizumab with chemotherapy.
Full table
Conclusions
This is an unusual case of a patient with prolonged disease-free survival of a recurrent small bowel signet ring adenocarcinoma who experienced a complete radiologic response to bevacizumab with oxaliplatin-based chemotherapy. Further investigation of this regimen is warranted.
Acknowledgements
Disclosure: The authors have no conflict of interest to disclose.
References
- Jemal A, Siegel R, Xu J, et al. Cancer statistics, 2010. CA Cancer J Clin 2010;60:277-300. [PubMed]
- Bilimoria KY, Bentrem DJ, Wayne JD, et al. Small bowel cancer in the United States: changes in epidemiology, treatment, and survival over the last 20 years. Ann Surg 2009;249:63-71. [PubMed]
- Rondonotti E, Pennazio M, Toth E, et al. Small-bowel neoplasms in patients undergoing video capsule endoscopy: a multicenter European study. Endoscopy 2008;40:488-95. [PubMed]
- Howe JR, Karnell LH, Menck HR, et al. The American College of Surgeons Commission on Cancer and the American Cancer Society. Adenocarcinoma of the small bowel: review of the National Cancer Data Base, 1985-1995. Cancer 1999;86:2693-706. [PubMed]
- Dabaja BS, Suki D, Pro B, et al. Adenocarcinoma of the small bowel: presentation, prognostic factors, and outcome of 217 patients. Cancer 2004;101:518-26. [PubMed]
- Chang HK, Yu E, Kim J, et al. Adenocarcinoma of the small intestine: a multi-institutional study of 197 surgically resected cases. Hum Pathol 2010;41:1087-96. [PubMed]
- Overman MJ, Kopetz S, Lin E, et al. Is there a role for adjuvant therapy in resected adenocarcinoma of the small intestine. Acta Oncol 2010;49:474-9. [PubMed]
- Gibson MK, Holcroft CA, Kvols LK, et al. Phase II study of 5-fluorouracil, doxorubicin, and mitomycin C for metastatic small bowel adenocarcinoma. Oncologist 2005;10:132-7. [PubMed]
- Overman MJ, Varadhachary GR, Kopetz S, et al. Phase II study of capecitabine and oxaliplatin for advanced adenocarcinoma of the small bowel and ampulla of Vater. J Clin Oncol 2009;27:2598-603. [PubMed]
- Zaanan A, Costes L, Gauthier M, et al. Chemotherapy of advanced small-bowel adenocarcinoma: a multicenter AGEO study. Ann Oncol 2010;21:1786-93. [PubMed]
- Overman MJ, Pozadzides J, Kopetz S, et al. Immunophenotype and molecular characterisation of adenocarcinoma of the small intestine. Br J Cancer 2012:144-50. [PubMed]
- Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med 2004;350:2335-42. [PubMed]
- Kerbel RS. Antiangiogenic therapy: a universal chemosensitization strategy for cancer? Science 2006;312:1171-5. [PubMed]
- Brown LF, Berse B, Jackman RW, et al. Expression of vascular permeability factor (vascular endothelial growth factor) and its receptors in adenocarcinomas of the gastrointestinal tract. Cancer Res 1993;53:4727-35. [PubMed]
- Tsang H, Yau T, Khong PL, et al. Bevacizumab-based therapy for advanced small bowel adenocarcinoma. Gut 2008;57:1631-2. [PubMed]


