Survivorship after treatment of pancreatic cancer: insights via an Internet-based survivorship care plan tool
Introduction
Pancreatic cancer is an aggressive disease that presents a daunting set of challenges in survivorship. Prognosis remains poor with current 5-year relative survival estimated at 8% (1). Even those patients who undergo potentially curative resection with multimodal adjuvant therapy will ultimately die of disease due to local recurrence and/or distant metastasis (2). Further, there is a scarcity of effective interventions that physicians can offer at the time of recurrence.
Poor prognosis of disease should not exclude attention to survivorship care as every person is considered a survivor from the moment of diagnosis (3). Little dialogue or investigation has been committed to this topic in pancreatic cancer, perhaps to the detriment of the patient. A lack of supporting evidence devoted to surveillance practices in pancreatic cancer has led to heterogeneity in follow-up and disagreement on its necessity and efficacy (4-6).
Survivorship care plans (SCPs) offer an opportunity for both patients and providers to establish a plan beyond active treatment, in addition to enhancing communication across all parties. These documents often contain a treatment summary, counseling on late effects and their treatment, recommendations for cancer screening and health maintenance, referrals for follow-up care, and a list of support resources. The use of SCPs in patients with a diagnosis of pancreatic cancer has never been explored previously. This study examines a convenience sample from pancreatic cancer survivors and their proxies voluntarily utilizing a publically available Internet-based tool for creation of SCPs. We present patient-reported data to describe treatment patterns and related side effects, surveillance care patterns, and perceptions of the tool itself.
Methods
SCP
A team of oncology nurses and physicians at the Abramson Cancer Center of the University of Pennsylvania designed and published an Internet-based tool for the creation of individualized SCPs in 2007. This tool is publicly accessible via Oncolink (www.oncolink.org/oncolife), a cancer information website based at the University of Pennsylvania that averages more than 385,000 unique visits per month. In the past, this tool has also been available via livestrongcareplan.org from which a portion of the data were gathered for this study. The resource allows patients, family members, or healthcare providers to input data regarding demographics, diagnosis, and treatment course to provide individualized, comprehensive healthcare recommendations for future care (7). The recommendations included in its care plans are evidence- or consensus-based wherever possible, and are in accordance with guidelines provided by the National Cancer Institute and American Society of Clinical Oncology. In areas where guidelines are not established, the care plan’s recommendations are based on our institution’s own practice and with guidance from leaders in survivorship medicine.
The tool has undergone several revisions since its creation to include questions regarding late and long-term effects customized to the survivor’s specific treatments and/or primary cancer diagnosis. These responses, too, are used to prioritize content in the care plan.
The care plan tool is publicly accessible via OncoLink, allowing users to find it independently or be made aware by their healthcare provider. Upon completion of the tool’s queries, the care plan is generated and received in PDF format. Addition of a five-question, one-page user satisfaction survey was added through an optional link accessible upon receipt of the care plan.
Data collection and analysis
All users first provided demographic and treatment information. They were then queried about late- and long-term effects customized to their treatment course, with the intent of targeting outcomes for which the individual survivor was at highest risk. Not all users were offered every question regarding late effects given this adaptive line of questioning. Answer choices were typically formatted as “yes”, “no”, or “I don’t know” unless otherwise specified.
Only fully completed care plans were included in analysis. Demographic, treatment, management, and side effect profiles data were reviewed, in addition to follow-up survey responses.
Institutional Review Board approval was obtained prior to any study proceedings. For this analysis, data were obtained from the survivor user database for all pancreatic cancer patients since publication of the seventh version, which was expanded to include questions pertaining to late- and long-term effects. Survey respondents from May 2010 to October 2014 were included in this study.
Results
Demographics
This analysis included 117 care plans created for survivors of pancreatic cancer. Sex distribution was nearly equitable as 53% (n=62) were female and a majority of survivors were Caucasian (75%, n=88). Median age at diagnosis was 60 years (mean 58.9 years, range 19-91). Thirty-one percent (n=36) of survivors were 2 years or greater from diagnosis. Starting with the eighth version of this tool, users were asked about their disease status. Of 89 responders, 27% (n=24) reported living with metastatic disease, while 2% (n=2) were experiencing recurrence after completing treatment. Demographic details are further detailed in Table 1.
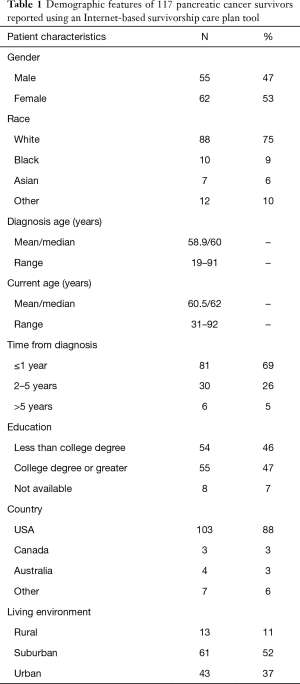
Full table
Treatments received and related long-term effects
A majority of survivors reported having had multimodality therapy (67%); the most common combinations being trimodality therapy with surgery, chemotherapy, and radiation (32%) and surgery/chemotherapy (21%). Of the 101 (86%) survivors who received chemotherapy, gemcitabine (n=75), fluorouracil (n=34), a platinum-based agent (n=21), and nab-paclitaxel (n=12) were frequently reported. Most survivors who received surgery (n=78, 67%) either underwent pancreaticoduodenectomy (n=68) or distal pancreatectomy (n=4). Forty-three percent (n=54) of survivors reported receipt of radiotherapy, with 74% (n=40) reporting radiation to the primary site and 22% (n=12) to metastatic disease.
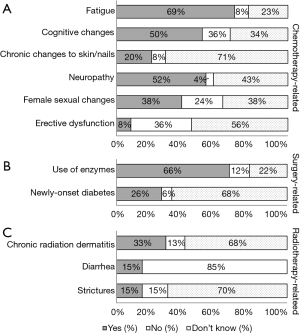
Late and long-term effects are reported by treatment modality in Figure 1. Fatigue, cognitive changes, and neuropathy were reported by 69%, 50%, and 52%, respectively, of survivors who received chemotherapy. While 38% of females reported sexual dysfunction, only 8% of males reported erectile dysfunction. For those survivors who had undergone surgery, many reported use of pancreatic enzymes for digestion (66%) and a diagnosis of diabetes since surgery (26%). Those having received radiation most frequently reported chronic radiation dermatitis (33%); gastrointestinal toxicities including chronic diarrhea or strictures/obstruction were both experienced by 15% of survivors.
Survivorship care patterns
SCPs were completed by the survivor themselves in 50% of cases and by a family member or friend in 31% of cases. Of the 19 healthcare providers (16% of all users) who completed SCPs, 13 were nurses and 6 were nurse practitioners (Table 2).
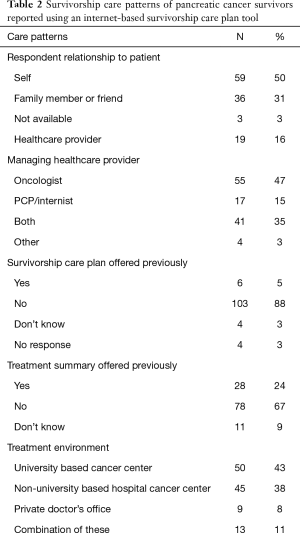
Full table
Most users reported continued care from an oncologist (47%) or both an oncologist and primary care provider (35%). The percentage of patients seeing an oncologist decreased over time, as 86% of survivors were managed or co-managed by an oncologist if less than 2 years from diagnosis (70 of 81 survivors) versus 72% if 2 or more years from diagnosis (26 of 36 survivors). A consequent increase in management by primary care providers alone was also observed, increasing from 11% (9 of 81 survivors) to 22% (8 of 36 survivors) once 2 or more years from diagnosis.
Twenty-four percent (n=28) of users had received a treatment summary yet only 5% (n=6) had received survivorship information following treatment for pancreatic cancer. Most patients received care at a cancer center, whether university based (43%, n=50), non-university based (38%, n=45), or in combination with another treatment setting (11%, n=13) (Table 2).
Survey results
A total of 24 users (21%) completed a brief five-question survey at the time of SCP receipt. Demographic details of survey responders were no different than non-responders. 4% (n=1), 38% (n=9), and 50% (n=12) of respondents felt that the plan contained too much, just enough, or not enough information, respectively; 8% (n=2) responded that they “did not know”. A total of 83% (n=20) reported they would share the healthcare provider summary with their healthcare team.
Discussion
Using a convenience sample of 117 pancreatic cancer survivors and their proxies, we examine survivorship care patterns and late effects of this population. Not only do we demonstrate that a small population of these survivors exists but that they seek guidance regarding survivorship issues through engagement with an Internet-based SCP tool. Fatigue, cognitive changes, neuropathy, pancreatic insufficiency, and chronic radiation dermatitis are frequently reported by this population who received mostly multimodality therapy. Although a large majority are managed or co-managed by an oncology specialist, only a minority of survivors have previously received survivorship information. Upon receipt of the Internet-based SCP, many respondents expressed that they would share the plan with their healthcare team yet desired more information than the plan provided.
We describe a population of pancreatic cancer survivors, most of whom received multimodality treatment and present self-reported late- and long-term effects by treatment modality. Chemotherapy was most commonly associated with fatigue, cognitive changes, and neuropathy. The high degree of neuropathy is not surprising, considering that many survivors received a platinum-based agent and/or nab-paclitaxel with which the association of peripheral neuropathy is well-established (8,9). Our tool, however, cannot determine the chronicity of this effect and many of these reports may reflect acute treatment-related effects if the survivor is undergoing salvage therapy. Surgery was associated with use of pancreatic enzymes and, to a lesser extent, a new diagnosis of diabetes; likely due to most post-surgical survivors having undergone some degree of pancreatic resection. Finally, radiotherapy was associated with chronic radiation dermatitis, chronic diarrhea, and strictures/obstruction. These findings are consistent with previous studies with patient-reported outcomes, many of which utilize the QLQ-PAN26, an EORTC-affiliated disease-specific quality of life questionnaire (10-13). The use of patient-reported outcomes is especially important in cancers with poor prognoses to ensure that any intervention to extend survival is undertaken in a meaningful manner, as judged by the patients themselves. A customizable SCP—much like the one we present—has potential to improve communication between patient and physician regarding treatment-related effects, as well as to facilitate shared-decision making in survivorship.
Nearly one-third of these survivors were alive 2 or more years from diagnosis and of these, nearly 75% were living without disease. Foremost, this suggests that there remains a significant period following active treatment that patients can benefit from survivorship support. Additionally, even though many survivors may be without present disease, sustained disease-free survival does not equate with definitive cure (14,15). Probable relapse should not deter nor delay provision of survivorship care, but instead, offer an opportunity to improve survivorship support. Many pancreatic cancer patients convey a limited understanding of their prognosis while clinicians believe patients are aware of their recurrence risk (4). SCPs, if appropriately articulated, could stand to improve communication between physicians and patients regarding prognosis while still providing hope.
Although a majority of survivors were being managed in some part by an oncology specialist, nearly half of these patients were co-managed with primary care providers. Furthermore, the percentage of survivors managed by a cancer specialist decreased over time with a resultant increase in management by primary care providers alone. This is consistent with previous reports on physician oversight in pancreatic cancer patients following surgical resection, and suggests a transition in care from a cancer specialist to a primary care provider over time (5). These observations indicate that pancreatic cancer patients often rely on co-managed care and can also expect transitions between care teams in survivorship, signaling a necessity for effective cross-team communication for which application of SCPs could prove valuable.
That so few survivors report previous receipt of survivorship information suggests that these communication tools are still underutilized in this population. Furthermore, this number is lower than previous studies utilizing responses from the OncoLink SCP tool for other cancer sites (16-19). As many pancreatic cancer patients are anticipated to live with incurable disease from time of diagnosis or to relapse soon after treatment, providers may defer provision of an SCP. Additionally, although the American College of Surgeons’ Commission on Cancer has issued requirements that SCPs be integrated into clinical practice starting in 2015, these guidelines exclude patients with metastatic disease and, further, suggest prioritization of common disease sites such breast, colorectal, prostate, lung, and lymphoma (20). Without pressure from this outside mandate, SCP use in pancreatic patients is unlikely to increase in the coming years relative to their disease counterparts unless a unique benefit is recognized by both survivors and their providers.
An overwhelming number of survey respondents indicated that they would share the healthcare provider summary portion of their SCP with their healthcare team. This is despite half of respondents answering that their plan could use more, or did not have enough, information. Although one may expect that the latter opinion would preclude the former, the coexistence of these views may be explained by a more nuanced interpretation. Focus groups utilizing patients with advanced or metastatic cancer have identified that SCPs are useful for this population but that their needs in survivorship are somewhat different from those survivors who face better prognosis. These patients endorse a more focused plan that centers on current management, rather than future care or scenarios (6). Thus, our survey respondents’ dissatisfaction may have been prompted by the content of information, rather than the volume of information included in the document.
Finally, we observed a more equitable representation of male and female survivors than in previous studies utilizing the OncoLink SCP tool, in which a female preponderance is typically reported (7,19,21,22). We hypothesized that this was likely due to inclusion of responses from both patients and proxies, with the latter party responding in place for a majority of male survivors. This was confirmed upon review of our data as only 39% of self-reporting survivors were male while 58% of family and friends responded for a male survivor. This suggests a weaker engagement of male survivors with the SCP tool and is consistent with previous reports on health information seeking behavior (23). Further investigation of this observation is warranted especially as it may reveal barriers in utilization of survivorship care.
There are limitations to the data we present. The tool itself does not allow users to provide staging information, which could not only affect treatment-related effects but also the survivor’s perspective on survivorship. We did observe, however, that our cohort did contain an over-representative sample of patients receiving surgical intervention, as less than 20% of patients in the general population present with resectable disease (2). This may first indicate that our cohort is disproportionately representative of early stage disease, since surgery is often pursed with curative intent for these patients. It may also suggest that patients with early stage disease are more likely to use this tool because they envision some duration of extended survival. With that, our findings may not be generalizable to the pancreatic cancer population as a whole. This tool was also unable to distinguish between definitive versus salvage therapies, which could impact interpretation of patient-reported outcomes. For example, for patients receiving salvage chemotherapy for recurrent or metastatic disease may be attributing symptoms related to disease-progression as treatment-related effects.
Further, our study relied on self-initiated participation, which could introduce selection bias as patients or proxies experiencing extremes of treatment may be prompted to pursue creation of an SCP. Self-reporting, however, may also mitigate reporter bias since patients or proxies are not vulnerable to the judgments imposed by healthcare providers during routine questioning at follow-up appointments.
Pancreatic cancer patients face a unique set of challenges in survivorship given that this malignancy has overall poor survival, a high propensity for recurrence, and non-curative treatment when relapse occurs. We have shown that there is small population of pancreatic cancer survivors who exist and seek support, but for whom structured survivorship care planning is lacking in practice. SCPs have a potentially valuable role for these survivors via communication of treatment-related effects and coordination across multidisciplinary healthcare teams. Such plans may better accommodate this challenging population by accurately conveying the risk of relapse, integrating issues related to relapse, and prioritizing issues pertaining current management. Further development and evaluation of SCPs for pancreatic cancer patients is needed.
Acknowledgements
This work was supported in part by the LIVESTRONG Foundation in the form of an unrestricted educational grant.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This research protocol was approved by our institutional review board (811528) and conforms to the provisions of in accordance with the Helsinki Declaration as revised in 2013. A waiver of informed consent was obtained from the institutional review board prior to initiation of any study proceedings.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2017. CA Cancer J Clin 2017;67:7-30. [Crossref] [PubMed]
- Gillen S, Schuster T, Meyer Zum Büschenfelde C, et al. Preoperative/neoadjuvant therapy in pancreatic cancer: a systematic review and meta-analysis of response and resection percentages. PLoS Med 2010;7:e1000267. [Crossref] [PubMed]
- President’s Cancer Panel. Living Beyond Cancer: Finding a New Balance. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; 2004.
- Deobald RG, Cheng ES, Ko YJ, et al. A qualitative study of patient and clinician attitudes regarding surveillance after a resection of pancreatic and peri-ampullary cancer. HPB (Oxford) 2015;17:409-15. [Crossref] [PubMed]
- Sheffield KM, Crowell KT, Lin YL, et al. Surveillance of pancreatic cancer patients after surgical resection. Ann Surg Oncol 2012;19:1670-7. [Crossref] [PubMed]
- Mayer DK, Green M, Check DK, et al. Is there a role for survivorship care plans in advanced cancer? Support Care Cancer 2015;23:2225-30. [Crossref] [PubMed]
- Hill-Kayser CE, Vachani C, Hampshire MK, et al. An internet tool for creation of cancer survivorship care plans for survivors and health care providers: design, implementation, use and user satisfaction. J Med Internet Res 2009;11:e39. [Crossref] [PubMed]
- Ewertz M, Qvortrup C, Eckhoff L. Chemotherapy-induced peripheral neuropathy in patients treated with taxanes and platinum derivatives. Acta Oncol 2015;54:587-91. [Crossref] [PubMed]
- Hoy SM. Albumin-bound paclitaxel: a review of its use for the first-line combination treatment of metastatic pancreatic cancer. Drugs 2014;74:1757-68. [Crossref] [PubMed]
- Barbier L, Jamal W, Dokmak S, et al. Impact of total pancreatectomy: short- and long-term assessment. HPB (Oxford) 2013;15:882-92. [Crossref] [PubMed]
- Fitzsimmons D, Johnson CD. Quality of life after treatment of pancreatic cancer. Langenbecks Arch Surg 1998;383:145-51. [Crossref] [PubMed]
- Herman JM, Chang DT, Goodman KA, et al. Phase 2 multi-institutional trial evaluating gemcitabine and stereotactic body radiotherapy for patients with locally advanced unresectable pancreatic adenocarcinoma. Cancer 2015;121:1128-37. [Crossref] [PubMed]
- Hurt CN, Mukherjee S, Bridgewater J, et al. Health-Related Quality of Life in SCALOP, a Randomized Phase 2 Trial Comparing Chemoradiation Therapy Regimens in Locally Advanced Pancreatic Cancer. Int J Radiat Oncol Biol Phys 2015;93:810-8. [Crossref] [PubMed]
- Dusch N, Weiss C, Ströbel P, et al. Factors predicting long-term survival following pancreatic resection for ductal adenocarcinoma of the pancreas: 40 years of experience. J Gastrointest Surg 2014;18:674-81. [Crossref] [PubMed]
- Ferrone CR, Brennan MF, Gonen M, et al. Pancreatic adenocarcinoma: the actual 5-year survivors. J Gastrointest Surg 2008;12:701-6. [Crossref] [PubMed]
- Berman AT, DeCesaris CM, Simone CB 2nd, et al. Use of Survivorship Care Plans and Analysis of Patient-Reported Outcomes in Multinational Patients With Lung Cancer. J Oncol Pract 2016;12:e527-35. [Crossref] [PubMed]
- Grover S, Hill-Kayser CE, Vachani C, et al. Patient reported late effects of gynecological cancer treatment. Gynecol Oncol 2012;124:399-403. [Crossref] [PubMed]
- Sloane K, Vachani C, Hampshire MK, et al. Late effects in survivors of central nervous system tumors: reports by patients and proxies. J Cancer Surviv 2016;10:234-40. [Crossref] [PubMed]
- Frick MA, Vachani CC, Hampshire MK, et al. Survivorship after lower gastrointestinal cancer: Patient-reported outcomes and planning for care. Cancer 2017;123:1860-8. [Crossref] [PubMed]
- Commission on Cancer of the American College of Surgeons. Cancer Program Standards: Ensuring Patient-Centered Care (2016 Edition). Available online: www.facs.org/cancer/coc/programstandards.html
- Hill-Kayser CE, Vachani C, Hampshire MK, et al. Patient-reported toxicity after colorectal cancer (CRC) treatment. J Clin Oncol 2011;29:484. [Crossref]
- Metz JM, Hampshire MK, Vachani C, et al. Patient-reported toxicities and comorbidities after treatment for cancers of the upper gastrointestinal tract. J Clin Oncol 2012;30:148. [Crossref]
- Kontos E, Blake KD, Chou WY, et al. Predictors of eHealth usage: insights on the digital divide from the Health Information National Trends Survey 2012. J Med Internet Res 2014;16:e172. [Crossref] [PubMed]


