Travel distance and use of salvage palliative chemotherapy in patients with metastatic colorectal cancer
Introduction
Colon cancer is one of the most common cancers diagnosed in Western countries. It is the third most common cancer and second leading cause of cancer-related death in North America (1). With the availability of several novel cytotoxic and biological agents and the prevalence of hepatic and lung metastasectomy and other liver-directed therapies over the past two decades, the survival rate of patients with metastatic colorectal cancer has improved. Nevertheless, there is a known disparity in cancer treatment and outcomes in patients living with cancer (2). A longer distance to travel for cancer care is known to be associated with less frequent use of recommended services and could be a burden to cancer patients (3-6). It has been shown that rural-dwelling patients with colorectal cancer often travel long distances for their cancer care, with potential associated burdens of time, cost and discomfort (7). Wasif and others reported that travel distance was associated with differential 90-day and 5-year mortality rates in patients who undergo surgical resection of gastrointestinal cancers (8). Likewise, Massarweh and others using the National Cancer Database demonstrated that increased travel distance was associated with more advanced colorectal cancer stage at the time of diagnosis (9). Evidence also showed a lower quality of life among colorectal cancer survivors who live far from their treating hospital (10).
Salvage cytotoxic and biological agents following progression on a first-line anti-cancer regimen improves the outcomes of patients in several advanced malignancies. Results from randomized clinical trials have demonstrated that salvage second- and third-line therapies in metastatic colorectal cancer have been associated with significant improvement in survival (1,11). Moreover, outcomes of patients with metastatic colorectal cancer are better if they are exposed to all available cytotoxic drugs during the course of their disease (12). However, not all patients receive all available therapies. Delays in starting treatment and travel burden can affect patient access and use of future therapy. Little is known about the relationship between travel distance (TD) to the cancer center and salvage second- and third-line therapies in metastatic colorectal cancer (CRC). The study aims to determine the relationship between travel distance to the cancer center with second- and subsequent lines of therapies. We hypothesize that travel distance to the cancer center affects access to second- and subsequent line therapy in patients with advanced CRC.
Methods
The University of Saskatchewan’s Research Ethics Board approved this study. The Ethics Board provided exemption for the informed consent. We studied a cohort of patients with metastatic colorectal cancer who were diagnosed from January 2006 to December 2010 in the province of Saskatchewan, Canada. Saskatchewan is a prairie province in western Canada with an area of 651,900 square kilometers and a population of approximately 1.1 million (13). Patients with World Health Organization (WHO) performance status of >1 and those who did not receive chemotherapy were excluded. Travel distance was measured by using driving distance based on Geographic Information System (GIS) software. Survival of the study cohort was estimated by using the Kaplan-Meier (KM) method. The survival distributions of different groups were compared by the log-rank test. Based on the use of second- or third-line therapy, the study cohort was divided into two groups. Patients in group A received salvage second- or third-line palliative chemotherapy, and patients in group B did not receive second-line therapy. Logistic regression analyses were performed to assess the relationships between various clinical variables and salvage second- and third-line therapy. The following variables were examined: distance travelled to cancer center, age (<70 vs. ≥70), gender, Charlson comorbid index, WHO performance status (<1 vs. 1), blood urea nitrogen (BUN) (≥8 vs. <8 mmol/L), albumin (≥35 vs. <35 g/L), bilirubin (≥26 vs. <26 mmol/L), alkaline phosphatase (≥120 vs. <120 IU/L), hemoglobin (≥120 vs. <120 g/L), white blood cell (WBC) (≥11 vs. <11×109/L), carcinoembryonic antigen (CEA) (≥5 vs. <5 mcg/L), site (colon vs. rectal), stage (IVA vs. IVB), symptomatic disease, extra-hepatic metastases, resection of primary tumor, and metastasectomy.
All variables with P value of <0.1 in univariate analyses were fitted to a multivariable model to assess their independent relationship with subsequent line chemotherapy. In order to determine if the addition of an independent variable add significantly to the association of use of salvage therapy in the model, the likelihood ratio test and t test were performed. A two-sided P value of <0.05 were considered to be statistically significant. SPSS version 23.0 was used for statistical analysis (SPSS Inc. Chicago, IL, USA).
Results
A total of 326 patients with synchronous metastatic adenocarcinoma of the colon and rectum who received first-line chemotherapy were identified. Of 326 patients, 62 patients who had a WHO performance status of >1 were excluded. The median age of the 264 eligible patients was 62 years (IQR: 53–72). Sixty-one percent were male and 38% had a WHO PS of 0. Mean Charlson score was 9.0±1.3. The preferable first-line regimen in most patients was FOLFIRI ± bevacizumab. Median TD was 64.4 km (IQR: 4.8–166). Forty-three percent of patients had to travel >100 km for their treatment (Table 1).
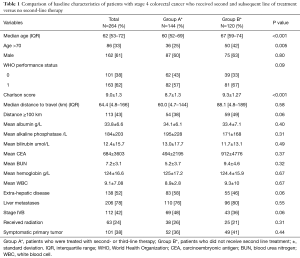
Full table
Of 264 patients, 144 (55%) in group A received salvage (second- and third-line) systemic therapies and 120 (45%) patients in group B did not receive further lines of therapy. There was a significant difference between the two groups with respect to age and comorbid illness. Patients who received salvage palliative systemic therapy were younger and had a significantly lower Charlson comorbid index (Table 1). The patients who received salvage systemic therapy had a median distance to travel of 60.0 km (IQR: 4.7–144) compared with 88.1 km (IQR: 4.8–189) if they did not receive second- or third-line therapy (P=0.58).
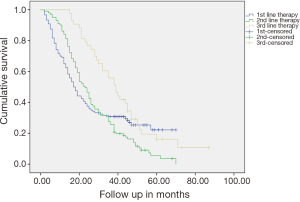
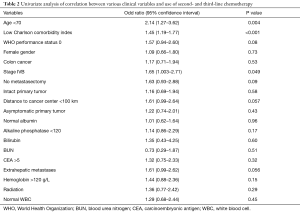
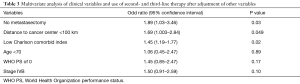
Median overall survival (OS) of the entire cohort was 23 months (95% CI: 20.1–25.8). Patients who did not receive second- and other line of therapies had median OS of 17 months (95% CI: 13.9–20.1) (Figure 1). Patients who received second-line therapy [mostly (5-Fluorouracil, leucovorin, and oxaliplatin) FOLFOX] had a median OS of 23 months (95% CI: 19.5–26.5), whereas patients who received third-line therapy (anti-epidermal growth factor receptor monoclonal antibodies ± irinotecan) had median OS of 39 months (95% CI: 32.6–45.4) (Figure 1). In univariate analysis, older age, lower Charlson comorbid index, WHO performance status of 0, distance to cancer center <100 km, no metastasectomy, intact primary tumor resection, and extrahepatic disease were significantly correlated with the use of second- or third-line therapy (Table 2). In multivariate analysis distance to the cancer center <100 km, odds ratio (OR) 1.69 (95% CI: 1.003–2.84), no metastasectomy, OR 1.89 (95% CI: 1.03–3.46), and absence of comorbid illness as per Charlson comorbid index, OR 1.45 (95% CI: 1.19–1.77) were correlated with the use of second- and subsequent line therapies (Table 3).
Full table
Full table
Discussion
Our results show that in patients with metastatic colorectal cancer and good performance status, the distance to travel correlated with differential use of second- and subsequent line of treatment. Although patients who received second- or third-line therapy were younger with a lower Charlson comorbid index, when these variables were fitted to a multivariate model, travel distance was independently correlated with the use of subsequent lines of chemotherapy. Overall, a travel distance to the cancer center lower than 100 km was associated with a 69% likelihood of receiving a second- or subsequent line of chemotherapy compared with patients who had to travel a distance greater than 100 km. In addition, unresectable metastatic disease, younger age, low burden of comorbid illnesses, WHO performance status of 0, and stage IVB disease or having more than one metastatic sites were correlated with use of second- or third-line chemotherapy. Given that a baseline low performance status can influence the duration of first-line chemotherapy and subsequent treatment, we excluded patients with a WHO performance status of 2 or greater.
There are several factors that potentially affect access to salvage therapy such as decline in performance status, previous treatment toxicity, skepticism about the benefit of further chemotherapy, or refusal to continue further treatment (14). Travel time is considered to be a direct cost of cancer care that mainly affects patients and their families (4,5). Repeated visits to the cancer center for assessment, investigations, and cancer treatment make distance an important factor for access and acceptance of treatment both in the curative and non-curative settings (14). For example, Lin and others using the National Cancer Database have shown that an increased travel burden was associated with a decreased likelihood of receiving adjuvant chemotherapy in patients with stage III colon cancer, regardless of insurance status (15). The association between travel distance and the use of salvage second- and third-line chemotherapy has not been adequately evaluated in patients with metastatic advanced colorectal cancer. To our knowledge, this is the first population-based study using individual patient data that examined the relationship between travel burden and the use of second- and third-line palliative chemotherapy in patients with metastatic colorectal cancer.
Our results confirmed that second- and third-line treatments can have a positive impact on survival and showed that real world patients who were treated with chemotherapy and received all available approved treatment have a median survival of 39 months, which signifies the importance of addressing the factors related to distance to travel, and this could influence early termination of active cancer-directed therapy.
Our study has several limitations. For example, we do not have information on physician or patient preferences that could influence decisions regarding whether or not to contemplate second-line therapy. Furthermore, we do not have information on social determinants including social support, education, and socio-economic status that could potentially influence the decision to carry on palliative chemotherapy. Hence, factors associated with less frequent use of second-line and further lines of chemotherapy in residents who were required to travel longer distances remains unknown.
In summary, our results revealed that a longer travel distance to the cancer center is associated with less frequent use of second- or subsequent line therapies in patients with metastatic CRC. Future studies are required to explore factors related to travel distance that could potentially affect under use of palliative chemotherapy in patients with metastatic colorectal cancer.
Acknowledgements
The study was supported by a research grant from Saskatchewan Cancer Agency. We would like to thanks to Drs. Haider, Zaidi, Abbas, Dueck, Asif, Mr. Riaz Alvi, MSc, Mrs. Carla Woites, Dr. Tong Zhu, and Saskatchewan Cancer Agency for their support for this project.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The University of Saskatchewan’s Research Ethics Board (NO. 06-44) approved this study. The Ethics Board provided exemption for the informed consent.
References
- Ahmed S, Johnson K, Ahmed O, et al. Advances in the management of colorectal cancer: from biology to treatment. Int J Colorectal Dis 2014;29:1031-42. [Crossref] [PubMed]
- Ahmed S, Shahid RK. Disparity in cancer care: a Canadian perspective. Current Oncology 2012;19:e376-82. [Crossref] [PubMed]
- Guidry JJ, Aday LA, Zhang D, et al. Transportation as a barrier to cancer treatment. Cancer Pract 1997;5:361-6. [PubMed]
- Schroen AT, Brenin DR, Kelly MD, et al. Impact of patient distance to radiation therapy on mastectomy use in early-stage breast cancer patients. J Clin Oncol 2005;23:7074-80. [Crossref] [PubMed]
- Celaya MO, Rees JR, Gibson JJ, et al. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States). Cancer Causes Control 2006;17:851-6. [Crossref] [PubMed]
- Scoggins JF, Fedorenko CR, Donahue SM, et al. Is distance to provider a barrier to care for Medicaid patients with breast, colorectal, or lung cancer? J Rural Health 2012;28:54-62. [Crossref] [PubMed]
- Baldwin LM, Cai Y, Larson EH, et al. Access to cancer services for rural colorectal cancer patients. J Rural Health 2008;24:390-9. [Crossref] [PubMed]
- Wasif N, Chang YH, Pockaj BA, et al. Association of distance traveled for surgery with short- and long-term cancer outcomes. Ann Surg Oncol 2016;23:3444-52. [Crossref] [PubMed]
- Massarweh NN, Chiang YJ, Xing Y, et al. Association between travel distance and metastatic disease at diagnosis among patients with colon cancer. J Clin Oncol 2014;32:942-8. [Crossref] [PubMed]
- Thomas AA, Gallagher P, O'Céilleachair A, et al. Distance from treating hospital and colorectal cancer survivors' quality of life: a gendered analysis. Support Care Cancer 2015;23:741-51. [Crossref] [PubMed]
- Guglielmi AP, Sobrero AF. Second-line therapy for advanced colorectal cancer. Gastrointest Cancer Res 2007;1:57-63. [PubMed]
- Grothey A, Sargent D. Overall survival of patients with advanced colorectal cancer correlates with availability of fluorouracil, irinotecan, and oxaliplatin regardless of whether doublet or single-agent therapy is used first line. J Clin Oncol 2005;23:9441-42. [Crossref] [PubMed]
- Statistics Canada. Available online: http://www.statcan.gc.ca/tables-tableaux/sum-som/l01/cst01/phys01-eng.htm
- Ambroggi M, Biasini C, Giovane CD, et al. Distance as a barrier to cancer diagnosis and treatment: review of the literature. Oncologist 2015;20:1378-85. [PubMed]
- Lin CC, Bruinooge SS, Kirkwood MK, et al. Association between geographic access to cancer care, insurance, and receipt of chemotherapy: geographic distribution of oncologists and travel distance. J Clin Oncol 2015;33:3177-85. [Crossref] [PubMed]


