Prolonged survival of metastatic hepatocellular carcinoma: a case report
Introduction
Hepatocellular carcinoma (HCC) is the second leading cause of cancer-related death in the world (1). The prognosis of HCC in our patient population, similar to other centres, is very poor largely due to the advanced stage at presentation with large and multinodular lesion as well as limited access to hepatobiliary service in our country. Overall median survival of HCC has been reported to be around 11 months from the date of diagnosis (2). Multimodality approaches provide better outcome for advanced HCC, giving better quality of life (3). We report a case of metastatic HCC who had gone radical surgeries despite his advanced stage of disease.
Case presentation
A 50-year-old gentleman, with no known comorbid, presented with 1-month history of non-specific abdominal pain with palpable abdominal mass over right hypochondrium. Investigation revealed raised alpha fetoprotein (AFP), 146 ng/mL. Hepatitis screening was negative. Ultrasound abdomen showed large heterogenous solid mass in right lobe of liver. Computed tomography (CT) liver 3 phase showed large heterogenous enhancing mass measured 12 cm × 10 cm right lobe of liver with area of central hypodensity likely of central necrosis and enhanced in late arterial phase (Figure 1). MRI liver showed T1 hypointense and T2 hyperintense mass measuring 10.5 cm × 10 cm × 9 cm in segment 6/7 of liver and a smaller T1 hypointense and T2 hyperintense with peripheral enhancement lesion measuring 2 cm × 2 cm × 1.5 cm at the edge of segment 3.
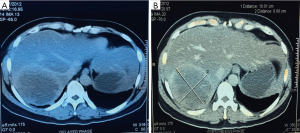
He underwent right hemihepatectomy and local excision of tumor at segment 3 in July 2012. Histopathology of both lesions confirmed hepatocellular carcinoma, grade 2. Post operatively, AFP reduced to 3.2 ng/mL. Subsequent 3-monthly surveillance AFP showed increasing level to 24.8 ng/mL 1 year later. CT staging in August 2013 showed no recurrence in the liver but there were two lung lesions at left lower lobe; posterobasal segment 1.6 cm × 1.5 cm and lateral basal segment 1 cm in size. Radiofrequency ablation (RFA) of both lung lesions done in August 2013. AFP post RFA reduced to 2.9 ng/mL. Unfortunately, AFP increased over 1 year and CT scan (Figure 2) showed left posterior basal segment lung lesions and hilar lymphadenopathy in December 2014, not possible for RFA. Clinically he only had minimal cough and as such requested delay in starting Sorafenib which was finally started in April 2015 at the dose of 400 mg BD.
Unfortunately, AFP kept increasing to 85 ng/mL and CT staging in January 2016 showed larger lung metastases with no other distant metastases.
In April 2016, he underwent left thoracotomy and pneumonectomy of lung metastases and removal of mediastinal nodes. Histopathology report of the tumour was consistent with that of metastatic hepatocellular carcinoma. Sorafenib was restarted a month after surgery.
He is now 5 years from the initial diagnosis of stage III hepatocellular carcinoma and 4 years from the diagnosis of stage IV metastatic hepatocellular carcinoma. He is clinically well and maintain an active and productive life with minimal effect only on effort tolerance. Latest CT surveillance in August 2017 showed no evidence of disease recurrence. Recent AFP in September 2017 remains 2.25 ng/mL.
Discussion
Our patient initially was diagnosed with locally advanced multinodular hepatocellular carcinoma, Barcelona clinic liver cancer (BCLC) intermediate stage (stage B). Although EASL/EORTC guidelines (3) recommend transarterial chemoembolization (TACE), our patient had surgery instead because it was felt that this is the best chance of cure for him.
Many groups have shown that not only liver resection in large or multinodular HCC with good liver function can be done safely (4), they have also showed that that liver resection can potentially give better overall survival than TACE for selected BCLC-B patients (5-7). In a study by Zhong et al., 39% of BCLC-B HCC patients who had liver resection still surviving at 3 years post procedure compared to only 16% in those who had TACE instead. The study also found that both techniques have acceptable morbidity and similar in-hospital mortality (8).
Our patient’s liver remains clear of disease post liver resection but when the disease recurs 1 year later, it unfortunately recurred in the lung. Although lung metastases are more uncommon than intrahepatic recurrence post resection, it is the commonest site of extrahepatic spread in HCC (9,10). Radical treatment of lung metastases is usually contraindicated as most of the patients would have multiple lung metastases rather than single lesion.
Therefore, patients with metastatic hepatocellular carcinoma usually are treated with systemic treatment with a multikinase inhibitor, sorafenib. Although sorafenib can potentially improves survival of these patients to 10.7 vs. 7.9 months of best supportive care, this is hardly a curative treatment (11). Our patient had sorafenib for 10 months but this fails to control his rising AFP and enlarging lung lesions.
We found a few studies that discussed surgical approach for lung metastases in hepatocellular carcinoma. In a case series reported by Tomimaru et al., he looked at 14 of his patients who had one or two potentially resectable lung metastases following liver resection of the primary disease. Of these, eight underwent resection of the metastases and six did not. They found that the 1-, 3- and 5-year survival rates following lung metastatectomy was 83.3%, 33.3% and 33.3% vs. 33.3%, 0% and 0% in HCC patients who did not have their lung metastases removed (P=0.03) (12). In a more recent report by Zhou et al. reported a median overall survival of 33 months (range, 10.7–77 months) for HCC patients who underwent lung metastatectomy (13).
Because of this, as our patient was a fit man still leading an active and productive life, we feel that we ought to approach the case more radically. Fortunately, we do not have that restricted access to cardiothoracic services compared to hepatobiliary and patient had successfully undergone the surgery last year.
Conclusions
Our patient has now survived 5 years following the initial diagnosis of HCC stage III and 4 years since diagnosis of lung metastases. He demonstrated that best outcome comes from personalised treatment, close surveillance, early detection of relapse and multimodality approach.
Acknowledgements
We would thank Dr. Foo Kin Keong (hepatobiliary surgeon, Sime Darby Medical Centre) and Dr. George John A/L K Thomas George (previous cardiothoracic surgeon in General Hospital Kuala Lumpur).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- El-Serag HB, Kanwal F. Epidemiology of hepatocellular carcinoma in the United States: where are we? Where do we go? Hepatology 2014;60:1767-75. [Crossref] [PubMed]
- Greten TF, Papendorf F, Bleck JS, et al. Survival rate in patients with hepatocellular carcinoma: a retrospective analysis of 389 patients. Br J Cancer 2005;92:1862-8. [Crossref] [PubMed]
- European Association For The Study Of The Liver, European Organisation For Research And Treatment Of Cancer. EASL–EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 2012;56:908-43. [Crossref] [PubMed]
- Ho MC, Huang GT, Tsang YM, et al. Liver resection improves the survival of patients with multiple hepatocellular carcinomas. Ann Surg Oncol 2009;16:848-55. [Crossref] [PubMed]
- Ettorre GM, Levi Sandri GB, Colasanti M, et al. Liver resection for hepatocellular carcinoma ≥5 cm. Transl Gastroenterol Hepatol 2017;2:22. [Crossref] [PubMed]
- Allemann P, Demartines N, Bouzourene H, et al. Long-term outcome after liver resection for hepatocellular carcinoma larger than 10 cm. World J Surg 2013;37:452-8. [Crossref] [PubMed]
- Torzilli G, Belghiti J, Kokudo N, et al. A snapshot of the effective indications and results of surgery for hepatocellular carcinoma in tertiary referral centers: is it adherent to the EASL/AASLD recommendations?: an observational study of the HCC East-West study group. Ann Surg 2013;257:929-37. [Crossref] [PubMed]
- Zhong JH, Ke Y, Gong WF, et al. Hepatic resection associated with good survival for selected patients with intermediate and advanced-stage hepatocellular carcinoma. Ann Surg 2014;260:329-40. [Crossref] [PubMed]
- Shah SA, Cleary SP, Wei AC, et al. Recurrence after liver resection for hepatocellular carcinoma: risk factors, treatment, and outcomes. Surgery 2007;141:330-9. [Crossref] [PubMed]
- Natsuizaka M, Omura T, Akaike T, et al. Clinical features of hepatocellular carcinoma with extrahepatic metastases. J Gastroenterol Hepatol 2005;20:1781-7. [Crossref] [PubMed]
- Llovet JM, Ricci S, Mazzaferro V, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med 2008;359:378-90. [Crossref] [PubMed]
- Tomimaru Y, Sasaki Y, Yamada T, et al. The significance of surgical resection for pulmonary metastasis from hepatocellular carcinoma. Am J Surg 2006;192:46-51. [Crossref] [PubMed]
- Zhou YM, Zhang XF, Yu F, et al. Efficacy of surgical resection for pulmonary metastases from hepatocellular carcinoma. Med Sci Monit 2014;20:1544-9. [Crossref] [PubMed]



