Total gastrectomy with isoperistaltic jejunal interposition flap for symptomatic management of gastric polyposis from familial adenomatous polyposis
Introduction
Familial adenomatous polyposis (FAP) is characterized by the development of copious adenomatous polyps throughout the gastrointestinal (GI) tract, namely the colon and rectum. The first of these polyps usually present in adolescence but the disease is progressive, with both increased number of polyps and malignant transformation with advancing age. Up to 80% of patients have extra colonic polyps, usually involving the upper GI tract including the stomach and duodenum. The inherent concern of course is the guaranteed development of malignancy arising from the APC germline mutation located on chromosome 5q. Cancer usually develops at a mean age of 35 years, as such, prophylactic colectomy with or without a proctectomy is considered standard of care.
Extra-colonic polyps are usually benign in nature, although frequent surveys via endoscopy and pathologic confirmation via biopsy are required. Unless malignancy is detected, surgical intervention for these upper GI polyps is unnecessary.
In this case report we describe a patient with known FAP who presented with gastric outlet obstruction as well as global gastric dysmotility as a result of polyp carpeting of the gastric mucosa albeit no evidence of malignancy. The symptomatology of the patient necessitated a total gastrectomy with reconstruction for definitive management.
Case report
A 40-year-old male well known to the GI service was admitted to the hospital with recurrent complaints of hematemesis, early satiety, poor appetite, and persistent nausea. The patient had undergone multiple upper and lower endoscopies since his diagnosis of FAP in 2005. He originally underwent a total colectomy with an ileorectal anastomosis to follow in 2007. He had some known rectal polyps that were being serially monitored with flexible sigmoidoscopy. Due to his GI complaints, the patient underwent esophagogastroduodenoscopy (EGD) at an outside hospital which he reported to note diffuse gastric polyposis. Given his recent history of hematemesis he then underwent repeat EGD at our hospital.
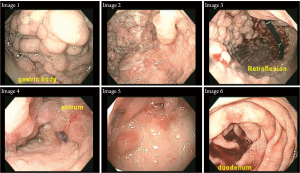
The patient’s original EGD at the outside hospital could not visualize the duodenum because the polyposis at the gastric pylorus did not allow for the scope to be advanced. However, the repeat EGD done at our institution was able to visualize the duodenum. It was noted the patient had diffuse carpeting of pedunculated polyps throughout the fundus, body, cardia, and antrum of the stomach. There was also superficial ulceration at the gastroesophageal junction and scattered polyps within the bulb of the duodenum. Otherwise the second portion of the duodenum appeared normal. Multiple biopsies were taken and final pathology showed gastritis and adenomatous polyps with no evidence of Helicobacter pylori. There was no evidence of malignancy. Of note, flexible sigmoidoscopy at the time showed a normal appearing anastomosis and one polyp from which a biopsy was taken. Figure 1 shows the extent of gastric polyposis found throughout the stomach.
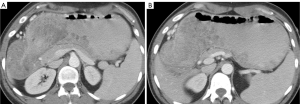
The patient was then referred to surgery clinic for further management of his symptoms. A CT scan was obtained which showed diffuse gastric polyposis as well as diffuse gastric distention (Figure 2A,B). The patient was subsequently admitted for clinically significant anemia secondary to hematemesis. Patient was again noted to have diffuse gastritis with focal ulcerations secondary to the extensive polyposis. The patient was managed non-operatively but it was decided that the patient’s persistent symptoms would require definitive surgical treatment. The patient was started on total parenteral nutrition (TPN) given poor nutrition and in preparation for surgery.
The patient was pre admitted for pre operative optimization and then went to surgery for a planned exploratory laparotomy, total gastrectomy, isoperistaltic jejunal interposition graft, distal jejunojejunostomy, duodenojejunostomy, and placement of a distal feeding tube.
Discussion
FAP is a hereditary condition characterized by the development of polyps both in the colon as well as in extra-colonic locations. Polyps in the stomach and small intestine develop in about 90% of patients. The gastric polyps primarily consist of fundic gland hyperplasia, however occasionally gastric adenomas are found. Notably, gastric cancer is only rarely reported as a complication of FAP in the United States.
Small intestinal neoplasia is however not rare in FAP and principally occurs in the periampullary region of the duodenum. Duodenal adenomatous polyps, which typically appear later than the colonic lesions may be multiple but tend not to carpet the small intestine. The ampulla of Vater is a particular target for neoplastic development. With time, carcinoma develops in up to 5% to 10% of these patients, therefore duodenal surveillance is required. This was a key point in deciding to proceed with a jejunal flap in our patient because it allowed for close surveillance of the duodenum. The standard Roux-en-Y reconstruction performed after a gastrectomy makes visualizing the duodenum very difficult.
Total gastrectomy with isoperistaltic jejunal interposition in the setting of gastric polyposis in FAP has not previously been reported in the literature. Jejunal interposition is frequently used to treat dumping syndrome following gastrectomy or gastric bypass (1,2). The Henley jejunal interposition is preferred to Roux-en-Y gastric bypass due to the lower risk for the development of Roux stasis/post gastrectomy syndrome, characterized by poor emptying (3). The jejunal interposition is also superior in that it allows for easier endoscopic surveillance of the duodenum, a key necessity in FAP patients. Nuclear medicine Tc99m sulfur colloid intestinal emptying studies following jejunal interposition demonstrate a double exponential curve, consisting of both slow and fast components compatible with more physiologic emptying (4).
Notably, gastrectomy in the setting of gastric polyposis in patients with FAP is not routinely performed due to the low risk of malignant transformation of the gastric polyps in this setting. Our patient however had significant symptomatology including nausea, hematemesis and early satiety with no other explanation. Fortunately post-operatively the patient had near complete clinical improvement. Gastric polyps in the setting of FAP usually consist of fundic gland polyposis which has virtually no malignant potential. Adenomatous gastric polyps can also be seen in FAP and have a 40% chance of malignant transformation. Although gastric polyps are typically asymptomatic and often incidentally discovered, symptomatic presentations include occult bleeding, ulcerated polyps leading to anemia, and prolapsing polyps leading to gastric outlet obstruction, potentially requiring operative intervention.
In the setting of FAP, colonic interposition is not an option given the 100% risk for colonic adenomatous polyps and malignant transformation, necessitating total colectomy (5). Roux-en-Y gastrojejunostomy could be considered, however our patient had pre-operative symptoms of early satiety; secondarily due to the significant polyp burden in his stomach, a total gastrectomy was felt to be the best therapeutic option. The jejunal interposition flap has several advantages including low perioperative risk, good motor activity of the flap and lower incidence of intrinsic disease compared with other forms of reconstruction (6).
Conclusions
FAP is associated with gastric polyposis, which is typically asymptomatic. In the setting of symptomatic gastric polyposis, total gastrectomy with isoperistaltic jejunal interposition is a viable therapeutic option.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Fenger HJ, Kallehauge HE, Gudmand-Höyer E. Pathophysiological studies of the effect of isoperistaltic jejunal interposition in the treatment of the incapacitating dumping syndrome. Scand J Gastroenterol 1972;7:283-7. [PubMed]
- Morii Y, Arita T, Shimoda K, et al. Jejunal interposition to prevent postgastrectomy syndromes. Br J Surg 2000;87:1576-9. [PubMed]
- Aranow JS, Matthews JB, Garcia-Aguilar J, et al. Isoperistaltic jejunal interposition for intractable postgastrectomy alkaline reflux gastritis. J Am Coll Surg 1995;180:648-53. [PubMed]
- Mackie CR, Hall AW, Clark J, et al. The effect of isoperistaltic jejunal interposition upon gastric emptying. Surg Gynecol Obstet 1981;153:813-9. [PubMed]
- Maier A, Pinter H, Tomaselli F, et al. Retrosternal pedicled jejunum interposition: an alternative for Reconstruction after total esophago-gastrectomy. Eur J Cardiothorac Surg 2002;22:661-5. [PubMed]
- Yasuda T, Shiozaki H. Esophageal reconstruction using a pedicled jejunum with microvascular augmentation. Ann Thorac Cardiovasc Surg 2011;17:103-9. [PubMed]