Palliative care and end-of-life health care utilization in elderly patients with pancreatic cancer
Introduction
Pancreatic cancer is the fourth leading cause of cancer related mortality in the Unites States and has a 5-year overall survival (OS) of less than 10% (1,2). Patients with pancreatic cancer also experience high symptom burden, especially towards the end of life, and symptom palliation is the cornerstone of management (3).
Palliative care programs offer comprehensive supportive care services for cancer patients beyond conventional, disease-directed therapies, and provide holistic care which can lead to better cancer outcomes. There has been a sharp increase in availability of palliative care services in US hospitals (4). This can be in the form of dedicated palliative care, nutrition, physical therapy, nursing, mental health and social services. This is particularly relevant to pancreatic cancer, which has exceptionally high mortality and morbidity. Palliative care, when provided in parallel with antineoplastic therapies, can lead to improved cancer outcomes including improved OS and quality of life (5-9). Especially if offered early in the disease course, palliative care can lead to less aggressive interventions near the end of life (6). These interventions are frequently futile, can be detrimental to patient quality of life and significantly add to overall health costs. This is particularly relevant to pancreatic cancer, which has exceptionally high mortality and morbidity. In this study, we look to understand utilization of palliative care services among geriatric pancreatic cancer patients across the United States (US). We used a national database of Medicare beneficiaries diagnosed with pancreatic cancer to study the patterns of palliative care consultations. Additionally, we assessed the effect of palliative care on end-of-life health care utilization.
Methods
Data
Patients were identified using the National Cancer Institute Surveillance, Epidemiology, and End Results (SEER)-Medicare linked database which is a linkage of patient records from the SEER cancer registries with their Medicare enrollment and claims files (10). SEER is a national program that includes 18 cancer registries from 14 states across the United States, representing about 30% of the US population. The Medicare claim files include sociodemographic, clinical, tumor specific and treatment related information along with diagnostic and procedure details for linked patients aged 65 or more. Medicare files consists of health claims from both inpatient and outpatient care. We obtained inpatient hospitalizations from the Medical Provider Analysis and Review (MEDPAR) file which is a 100% utilization file with a unique record for each inpatient hospitalization covered under Medicare part A. Outpatient and National Claims History (NCH) files were used as indicated for institutional and non-institutional outpatient claims.
Patients
The inclusion criteria were:
- Medicare beneficiaries with a new diagnosis of pancreatic cancer between 2000 and 2009;
- Age at least 66 years at the time of analysis to include only those beneficiaries who received at least 1 year of Medicare benefits before death.
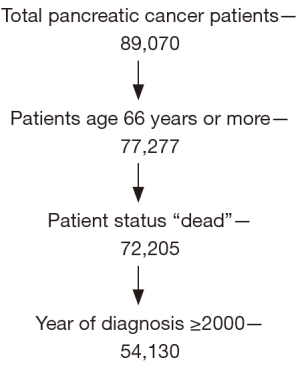
We excluded those patients with status as ‘alive’ since our aim was to assess health utilization before death only which resulted in a final study sample size of 54,130 (Figure 1).
We used the International Classification of Diseases, ninth revision codes (ICD-9) to identify the nature of care received during the hospital stay. Palliative care consultation was identified from appropriate Medicare files using ICD-9 codeV66.7 (11). For patients with more than one palliative care consult, only the first episode was included. Age, year of diagnosis, sex, race, marital status and stage were assessed from SEER-Medicare file.
We assessed the trends of palliative care consults and healthcare utilization patterns for patients diagnosed between 2000 and 2009. The following measures of health care utilization were assessed for the last 30 days of life: number of intensive care unit (ICU) admissions, mean length of stay in the ICU, cost associated with ICU stay, number of emergency room visits, and cost associated with ER visits. Cost of care was calculated by taking a sum of all charges in the last 30 days for each patient in the group (palliative care vs. no palliative care) and then dividing it by the number of patients in that group.
Chi-square tests and univariate logistic regression analyses were conducted to investigate if there were significant differences in patient demographics between palliative care and non-palliative care groups. Student’s t-tests were used to examine if there were significant differences in health services utilization between palliative care and non-palliative care groups. We used multivariate logistic regression to identify demographic characteristics and health service utilization that were significantly associated with palliative care consults.
We used propensity score matching to balance for observed differences between palliative and non-palliative care (12). Patients with palliative care were propensity matched with patients without palliative care in a 1:2 ratio. The following five variables were selected for propensity score matching based on multivariate analysis: sex, race, marital status and stage of disease. Health services utilization of patients who did and did not receive a palliative care consult were compared between the two groups.
Statistical analyses were performed with SAS version 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
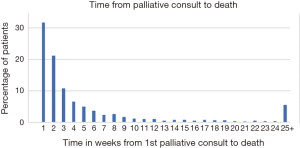
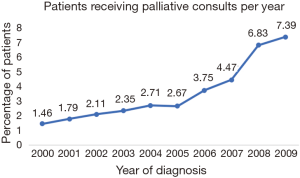
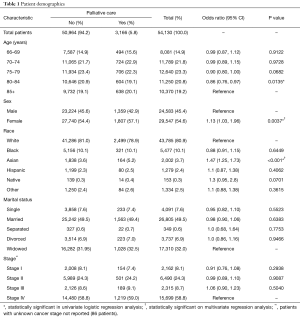
Of 54,130 cases, 54% were female, 81% were white and 5.8% (3,166) received a palliative care consult. Of all palliative care consults, 31.6% were in the last 7 days of life, 70% were within 30 days from death and 14% were between 30–60 days of death (Figure 2). Only 11% of patients received a palliative care consult more than 12 weeks before death. The proportion of patients receiving palliative care increased consistently from 1.46% for patients diagnosed in 2000, to 7.4% in 2009 (Figure 3, P<0.001) with a sharp rise in later years. Table 1 describes the sociodemographic and clinical characteristics of patients with and without palliative care. On univariate analysis, patients receiving palliative care were more likely to be female and Asian compared to patients without palliative care. Patients older than 85 years of age were more likely to receive palliative care consults. No statistically significant associations were seen between marital status and disease stage. On multivariate analysis, only Asian patients and female patients were more likely to receive palliative care consults.
Full table
Trends of health care utilization
The mean number of visits to the ER in the last 30 days of life were significantly higher for patients who received palliative care consults versus those who did not (0.9±0.6 vs. 0.8±0.6, P<0.001) and had a significantly higher cost of care ($1,436.8 vs. $1,060.7, P<0.001) (Table 2). The length of ICU stay for patients with palliative care was lower than those without (1.0 vs. 1.3 days, P=0.0017) (Table 2). There was no difference in the cost of care for ICU ($5,470.6 vs. $4,909.8, P=0.182) or number of ICU admissions between the two groups (P=0.140).
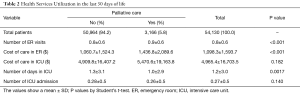
Full table
Propensity score matching
We compared health care utilization of patients with palliative care with propensity score-matched (PSM) patients without palliative care (Table 3). Univariate analysis revealed that in the last thirty days of life, the number of ED visits and cost of ED care were significantly higher for patients with palliative care. The cost of ICU care and number of admissions to ICU were not different between the two groups.
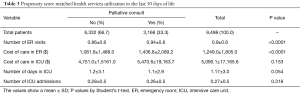
Full table
Discussion
In this study of Medicare patients with pancreatic cancer, the rate of palliative care consults increased a near 4-fold from 1.8% in 2000 to 7.8% in 2009. This increase in referral rates reflects recognition of palliative care as a distinct service for terminally ill patients and is a response to calls for increased integration of palliative services for cancer patients (13-15). In this analysis, palliative care is being offered to sicker patients near the end of life and is not associated with reduced health care utilization or cost. These findings are in contrast with controlled prospective studies that suggest that palliative care can reduce cost of care and resource utilization (16,17).
One-third of all palliative care consults in this cohort took place in the last week of life. Another population based study in patients with breast and colon cancer also reported that 40% of palliative care consults were ordered in the last 7 days of life (18). In contrast, Osta et al. (19) reported that time between palliative consult and death in a large comprehensive cancer center was 42 days—significantly longer than our analysis. This difference between the single institution experiences and population based analysis suggests that although palliative care referrals are increasing nationally, there are significant differences in patterns of utilization. Systematic implementation of palliative services is needed to extend findings from controlled studies to the broader population.
Previous studies have evaluated the rate of palliative care referrals in other solid tumors and also observed an increase in recent years (18). Age was significantly associated with palliative care consults while marital status was not. Other studies have also suggested that older patients are more likely to receive palliative care and this may provide insight on why population based studies have failed to demonstrate an impact of palliative care on markers of end of life health care utilization (20,21). Treatment decisions for elderly and terminally ill cancer patients can be complex and recommendations are to aim for early palliative care discussions for all patients, regardless of age. The potential benefit of palliative care in large database analysis can be diluted as older, and possibly sicker, patients are more likely to be referred.
In addition to trends and predictors of palliative care referrals in a cohort of elderly pancreatic cancer patients, we evaluated the impact of real world palliative care referrals on measures of end-of-life health care utilization. As most data on end of life health care utilization are based on studies in controlled prospective trials it is important to assess the impact in the real world setting. The unique features of the SEER-Medicare dataset made this analysis possible. Patients who received palliative care consults had more ER visits and higher cost of ER care compared to those with no palliative care. These findings are in contrast to a prospective single institution experience from a large US academic medical center (22) which demonstrated that palliative care results in lower re-admission rates in the last 30 days of life. The most common reason cancer patients seek care in the ER are uncontrolled symptoms which suggests ER visits may be a surrogate measure for poor symptom control (23). Patients with palliative care had more ER visits towards the end of life suggests palliative care referrals are preferentially offered to sicker patients with higher symptom burden. Guidelines which advocate for integration of palliative care services for cancers with poor prognosis such as pancreatic cancer, recommend universal palliative referrals early in the disease course (9). Our analysis suggest that palliative care referrals are being offered to sicker patients, and very late in the disease course which likely limits the impact of palliative care on end of life health care utilization as demonstrated in this paper.
There was no difference in ICU admissions and cost of care in ICU between the palliative and non-palliative groups. The length of ICU stay was lower in the palliative care group in univariate analysis which was not seen on multivariate analysis. This is likely explained by palliative care referrals being placed so close to death. Prior studies have shown that patients with palliative care consults are dying in the ICU which supports this observation (24-27). Propensity score matching was performed to reduce the effect of known confounding variables on outcome. The effect of palliative care on end of life health care utilization in the form of ER visits and ICU admissions in the last 30 days life utilization did not change. There is little difference in ICU costs or higher ER costs for palliative patients since sicker patients are likely to have higher treatment costs (28-30).
This observation is in contrast to the reported effect of palliative care referrals for cancer patients in controlled studies (6). Palliative care referrals are placed very late in the course of the disease. Patients are likely to have developed complications and encumbered significant costs by the time of referral which prevents palliative care from significantly impacting patient care. Lack of effective control of symptoms earlier in the disease course leads to higher symptom burden, poor quality of life and higher ER use (31,32). It is for these reasons that palliative care guidelines by professional oncology societies advocate for early incorporation of palliative care, as early as within 8 weeks of cancer diagnosis (9). This provides clinicians with more lead time to identify and address cancer symptoms before the onset of downstream complications.
Limitations of this study are those expected from a claims database of elderly patients. We only included patients older than 66 years of age, and the results may not be generalizable to the entire population. But as the average age of diagnosis of pancreatic cancer is in the 70s this study population is likely representative. For the purpose of this analysis we are unable to identify palliative care offered without an associated claim. This raises the potential for under-reporting of palliative care in our cohort. Reduced re-admission after palliative care in other studies was likely due to more goal oriented discussions about end of life care, rather than symptom management alone (22). The nature, and quality, of palliative care and quality of the program cannot be determined from a claims database. We performed propensity score matching to adjust for confounding factors associated with palliative care referrals but it is not possible to adjust for factors not measured by a claims database such as patient performance status. Cancer registries capture anticancer systemic therapies, radiation therapies and surgery but palliative care is not generally identified as a discrete treatment. The specific strengths of the SEER-Medicare linked database allowed this analysis to be completed and evaluate predictors of palliative care and time from death.
In conclusion, the rate of palliative care for elderly patients with pancreatic cancer has increased between 2000 and 2009. Referral to palliative care was not associated with a reduction in end of life ICU care and ED visits. Referrals are placed very late in the disease course and increasingly used for sicker patients. Early referral to palliative care may allow patients a greater opportunity to benefit from services targeting symptom control which may reduce potentially futile end of life health care utilization. Pancreatic cancer is associated with high mortality and morbidity and future studies should assess the effect of universal palliative care referral for all pancreatic cancer patients at the time of diagnosis.
Acknowledgements
Funding: Research reported in this publication was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award Number UL1TR001105.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was conducted in accordance with a SEER-Medicare data use agreement, and was approved by the University of Texas Southwestern Medical Center Institutional Review Board (No. STU 032013-045). This was a secondary analysis of an existing database the need for informed consent was waived.
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin 2016;66:7-30. [Crossref] [PubMed]
- Institute NC. Cancer Stat Facts: Pancreas Cancer. 2014. Avilable online: https://seer.cancer.gov/statfacts/html/pancreas.html. Accessed 09/29/2017 2017.
- Fitzsimmons D, Johnson CD. Quality of life after treatment of pancreatic cancer. Langenbecks Arch Surg 1998;383:145-51. [Crossref] [PubMed]
- Dumanovsky T, Augustin R, Rogers M, et al. The Growth of Palliative Care in U.S. Hospitals: A Status Report. J Palliat Med 2016;19:8-15. [Crossref] [PubMed]
- Perone JA, Riall TS, Olino K. Palliative Care for Pancreatic and Periampullary Cancer. Surg Clin North Am 2016;96:1415-30. [Crossref] [PubMed]
- Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010;363:733-42. [Crossref] [PubMed]
- Howie L, Peppercorn J. Early palliative care in cancer treatment: rationale, evidence and clinical implications. Ther Adv Med Oncol 2013;5:318-23. [Crossref] [PubMed]
- Schenker Y, Arnold R. Toward Palliative Care for All Patients With Advanced Cancer. JAMA Oncol 2017;3:1459-60. [Crossref] [PubMed]
- Ferrell BR, Temel JS, Temin S, et al. Integration of Palliative Care Into Standard Oncology Care: American Society of Clinical Oncology Clinical Practice Guideline Update. J Clin Oncol 2017;35:96-112. [Crossref] [PubMed]
- Institute NC. SEER-Medicare: How the SEER & Medicare Data are Linked. 2017. Available online: https://healthcaredelivery.cancer.gov/seermedicare/overview/linked.html. Accessed 09/29/2017 2017.
- Capello CF, Meier DE, Cassel CK. Payment code for hospital-based palliative care: help or hindrance? J Palliat Med 1998;1:155-63. [Crossref] [PubMed]
- Rosenbaum PR, Rubin DB. The Central Role of the Propensity Score in Observational Studies for Causal Effects. Biometrika 1983;70:41-55. [Crossref]
- von Gunten CF. Fellowship training in palliative medicine. J Palliat Med 2006;9:234-5. [Crossref] [PubMed]
- Portenoy RK, Lupu DE, Arnold RM, et al. Formal ABMS and ACGME recognition of hospice and palliative medicine expected in 2006. J Palliat Med 2006;9:21-3. [Crossref] [PubMed]
- Scott JO, Hughes L. A needs assessment: Fellowship Directors Forum of the American Academy of Hospice and Palliative Medicine. J Palliat Med 2006;9:273-8. [Crossref] [PubMed]
- Brumley R, Enguidanos S, Jamison P, et al. Increased satisfaction with care and lower costs: results of a randomized trial of in-home palliative care. J Am Geriatr Soc 2007;55:993-1000. [Crossref] [PubMed]
- Siderow S, Silvers A, Meier DE. Palliative Care Improves Quality of Care, Lowers Costs. Manag Care 2016;25:40-1. [PubMed]
- Roeland EJ, Triplett DP, Matsuno RK, et al. Patterns of Palliative Care Consultation Among Elderly Patients With Cancer. J Natl Compr Canc Netw 2016;14:439-45. [Crossref] [PubMed]
- Osta BE, Palmer JL, Paraskevopoulos T, et al. Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. J Palliat Med 2008;11:51-7. [Crossref] [PubMed]
- Warren JL, Barbera L, Bremner KE, et al. End-of-life care for lung cancer patients in the United States and Ontario. J Natl Cancer Inst 2011;103:853-62. [Crossref] [PubMed]
- Murphy JD, Nelson LM, Chang DT, et al. Patterns of care in palliative radiotherapy: a population-based study. J Oncol Pract 2013;9:e220-7. [Crossref] [PubMed]
- O'Connor NR, Moyer ME, Behta M, et al. The Impact of Inpatient Palliative Care Consultations on 30-Day Hospital Readmissions. J Palliat Med 2015;18:956-61. [Crossref] [PubMed]
- Mayer DK, Travers D, Wyss A, et al. Why do patients with cancer visit emergency departments? Results of a 2008 population study in North Carolina. J Clin Oncol 2011;29:2683-8. [Crossref] [PubMed]
- Rivet EB, Ferrada P, Albrecht T, et al. Characteristics of palliative care consultation at an academic level one trauma center. Am J Surg 2017;214:657-60. [Crossref] [PubMed]
- Khandelwal N, Brumback LC, Halpern SD, et al. Evaluating the Economic Impact of Palliative and End-of-Life Care Interventions on Intensive Care Unit Utilization and Costs from the Hospital and Healthcare System Perspective. J Palliat Med 2017;20:1314-20. [Crossref] [PubMed]
- Teno JM, Gozalo PL, Bynum JP, et al. Change in end-of-life care for Medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA 2013;309:470-7. [Crossref] [PubMed]
- Kathleen Sebelius TRF, Edward J. Sondik. Health, United States, 2010. Available online: https://www.cdc.gov/nchs/data/hus/hus10.pdf. Accessed 10/27/2017 2017.
- Chastek B, Harley C, Kallich J, et al. Health care costs for patients with cancer at the end of life. J Oncol Pract 2012;8:75s-80s. [Crossref] [PubMed]
- Bramley T, Antao V, Lunacsek O, et al. The economic burden of end-of-life care in metastatic breast cancer. J Med Econ 2016;19:1075-80. [Crossref] [PubMed]
- Chang HT, Lin MH, Chen CK, et al. Medical care utilization and costs on end-of-life cancer patients: The role of hospice care. Medicine (Baltimore) 2016;95:e5216. [Crossref] [PubMed]
- El-Jawahri A, Greer JA, Temel JS. Does palliative care improve outcomes for patients with incurable illness? A review of the evidence. J Support Oncol 2011;9:87-94. [Crossref] [PubMed]
- Basch E, Deal AM, Kris MG, et al. Symptom Monitoring With Patient-Reported Outcomes During Routine Cancer Treatment: A Randomized Controlled Trial. J Clin Oncol 2016;34:557-65. [Crossref] [PubMed]