|
Original Article
Bax expression is a candidate prognostic and predictive marker of colorectal cancer
Venkat R Katkoori1*, Catalina Suarez-Cuervo1,2*, Chandrakumar Shanmugam1, Nirag C Jhala1,3, Tom Callens4, Ludwine Messiaen4, James Posey III5,6, Harvey L Bumpers7, Sreelatha Meleth8, William E Grizzle1,6, Upender Manne1,6
1Department of Pathology, University of Alabama at Birmingham, Birmingham, AL; 2Evidence-based Practice Center, Johns Hopkins Schools of Medicine and Public Health, Baltimore, MD; 3Department of Pathology and Laboratory Medicine, University of Pennsylvania, Philadelphia, PA; 4Departments of Genetics and 5Medicine, University of Alabama at Birmingham, Birmingham, AL; 6UAB-Comprehensive Cancer Center, University of Alabama at Birmingham, Birmingham, AL; 7Department of Surgery, Morehouse School of Medicine, Atlanta, GA; 8Department of Preventive Medicine, University of Alabama at Birmingham, Birmingham, AL
*Both the authors contributed equally.
Corresponding to: Upender Manne, MS, PhD, Associate Professor, Department of Pathology, University of Alabama at Birmingham, 565-LHRB, Building 701, 19th Street South, Birmingham, AL 35294-0007. Tel: 205-934 4276; Fax: 205-975 9927. Email: manne@uab.edu.
This work was supported in part by grants from the National Institute
of Health/National Cancer Institute to Dr. U Manne (U54-CA118948, R03
CA139629, and R01-CA98932-S1).
|
|
Abstract
Objective:Since the anti-tumor activity of 5-fluorouracil (5-FU) is due to induction of apoptosis, we assessed the value of expression of key apoptotic molecules (Bax, Bcl-2 and p53) in predicting the efficacy of 5-FU therapy for colorectal adenocarcinomas (CRCs).
Methods:Archival tissues of CRCs from 56 patients who received a complete regimen of 5-FU-based chemotherapy after surgery, and 56 patients matched for age, gender, ethnicity, tumor stage, tumor location, and tumor differentiation who had undergone only surgery (without any pre- or post-surgery therapy), were evaluated for immunophenotypic expression of Bax, Bcl-2, and p53. Also, these CRCs were evaluated for Bax mutations. The predictive capacity or prognostic value of these markers was assessed by estimating overall survival.
Results:The majority of low Bax expressing CRCs have exhibited mutations at the G (8) tract. There was no significant difference in overall survival rates between the categories of surgery alone and 5-FU-treated patients. However, a better survival was observed for patients who received chemotherapy when their CRCs had low Bax/Bcl2 ratio (HR, 1.55; 95% CI: 1.46-31.00). Patients who received surgery alone and whose CRCs lacked Bax expression had 5.33 times higher mortality than those with high Bax expression (95% CI: 1.78-15.94), when controlled for tumor stage and other confounders. Bcl-2 and nuclear p53 accumulation had no predictive value in either patient group.
Conclusion:These findings are the first to demonstrate that high Bax expression is a good prognosticator for patients who underwent surgery alone, and that patient with low Bax/Bcl-2 expression ratio benefit from 5-FU-based adjuvant therapies.
Key words
colorectal adenocarcinoma; predictive marker; Bax; 5-Flurouracil
J Gastrointest Oncol 2010; 1: 76-89. DOI: 10.3978/j.issn.2078-6891.2010.019
|
|
Introduction
5-Fluorouracil (5-FU) remains the most commonly used
chemotherapeutic agent for the treatment of colorectal
cancers (CRCs). Nevertheless, more than 40 years of
5-FU usage has not yielded responses greater than 35-40%
( 1-5), neither has it decreased the rates of recurrence
( 6, 7). Therefore, novel strategies are required to predict
response to treatment. Although several molecular
markers have prognostic value for CRCs ( 8-15) their
predictive value in assessing treatment response remains
controversial( 7, 16-18). In addition to selecting the best
chemotherapeutic tools, a new challenge is to identify genetic and/or molecular markers that can be used as
predictors of response to treatment. As demonstrated for cultured cells, p53-dependent
apoptosis modulates the cytotoxic effect of chemotherapeutic
agents; cells with functional p53 or wild-type p53 (wt-p53)
are more sensitive, and cells with mutated or lack of p53 are
more resistant ( 19, 20). Lenz et al demonstrated a better rate
of response to 5-FU for patients whose tumors were wildtype
for p53 than those whose tumors had overexpressed
or mutated p53 ( 21). In contrast, Allegra et al found that
overexpressed p53 correlated with a better response to
treatment ( 22, 23), and Elsaleh et al ( 24) could not find
any relationship between p53 status and 5-FU response
or survival of patients with colon or rectal tumors. Thus,
data relating to the predictive value of p53 in CRCs is
contradictory and inconclusive. Apoptosis is a complex process that proceeds through
two pathways. The extrinsic pathway is based on cell surface
receptors and cytoplasmic proteins. The intrinsic pathway
occurs in the mitochondria, where the balance of pro- and
anti-apoptotic proteins is largely regulated by the members
of the Bcl-2 family. p53 has been described as a main
modulator of apoptosis in both pathways ( 25). The antitumor
activity of 5-FU has been related to its capacity to
induce apoptosis by damaging the DNA and/or by altering
the expression profiles of pro- and anti-apoptotic molecules
( 26-28). Chemo-resistance may depend on the function
and relationship between pro- and anti-apoptotic proteins
( 29, 30). The balance between anti-apoptotic (e.g., Bcl-2) and
pro-apoptotic proteins (e.g., Bax) in a cell determines its
susceptibility to apoptosis after 5-FU treatment( 31). Since
the checkpoint is controlled by the ratio between promoters
and inhibitors of apoptosis (i.e., the ratio of Bax to Bcl2)
and p53 ( 26-28), their concomitant expression should be
considered together in assessing their clinical significance.
In the current report, as a proof of concept, we evaluated
the predictive and prognostic usefulness of these markers
in two groups of CRC patients, one treated with surgery
alone and the second treated with surgery and 5-FU-based
adjuvant chemotherapy.
|
|
Patients and methods
Patients
The institutional review board of the University of Alabama
at Birmingham (UAB) approved these experiments, and
the Bioethics Committee reviewed the proposed effort.
From the UAB Hospital, we collected data for 650 patients
who were diagnosed and underwent surgery for primary
colorectal adenocarcinoma with curative intent between 1987 and 1993. Use of patients from this period maximized
post-surgery follow-up, because 70% of the patients (78 of
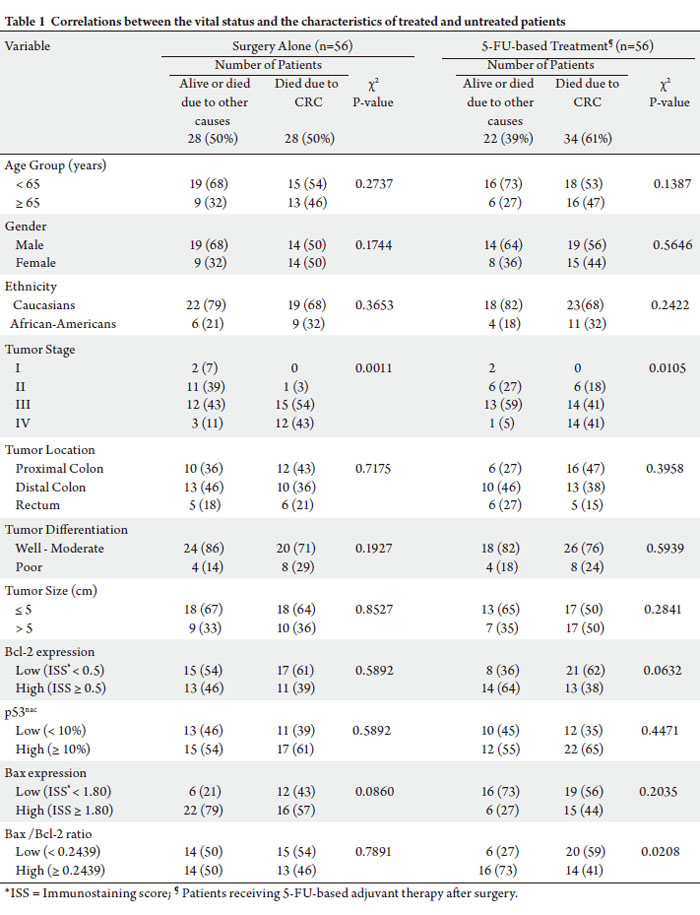
112) had either stage II or III CRCs (Table 1).
Patient eligibility criteria
During our initial selection process, patients who received
radiation and/or any chemotherapy before surgery were
excluded. We included only those patients who completed
at least 3 months of post-surgical adjuvant chemotherapy
and for whom there was complete information on dosage
and duration of treatment. With these criteria and the
availability of paraffin blocks, the final group consisted of 56
patients who had surgery plus 5-FU-based adjuvant therapy.
Treatment
Details of the chemotherapy were as follows: Twenty
eight patients received 5-FU alone, 12 patients received
5-FU plus levamisole (LV), 10 patients received 5-FU
plus leucovorin (LC), 4 patients received 5-FU plus
doxorubicin (5-FUDR), 1 patient received 5-FU/1-(2-
chloroethyl)-3-cyclohexyl-1-nitrosourea) (CCNU), and
1 patient received 5-FU/LV/LC. The control group of 56
patients, who were matched for age; gender; ethnicity;
and tumor stage, location, and histologic differentiation,
and who had undergone only curative resection without
adjuvant therapy after surgery were selected randomly
from the initial patient pool. In the surgery-alone group,
patients with stage III or IV CRCs did not receive adjuvant
therapy for various clinical and personal reasons but had
undergone surgery with a palliative intent. The final study
sample consisted of 112 patients; their characteristics are
given in Table 1.
Pathological evaluations
The surgical pathology reports were reviewed by three
investigators (CS-C, NCJ & CKS), and a pathologist
(NCJ) individually reviewed slides stained with
hematox ylin and eosin for the degree of histologic
differentiation and re-graded lesions as well, moderate,
poor or undifferentiated ( 32, 33). Well and moderately
differentiated tumors were pooled into a low-grade group,
and poor and undifferentiated tumors into a high-grade
group ( 34). Pathologic staging was performed according
to the criteria of the American Joint Commission on
Cancer ( 35). The International Classification of Diseases
for Oncology codes were used to specify the anatomic
location of the tumor ( 32). The tumor was considered
mucinous if ≥ 50% demonstrated mucinous histology ( 32).
The anatomic sub-sites were the proximal colon, the distal
colon, and the rectum. Three-dimensional tumor size was
determined; the largest dimension was used for statistical purposes.
Patient demographics and follow-up information
Patient demographics, along with clinical and follow-up
information, were retrieved retrospectively from medical
records, physician charts, and pathology reports and from
the UAB tumor registry. Patients were followed, either by
their physician or by personnel associated with the tumor
registry, until their death or the date of the last documented
contact. Through telephone and mail contacts, these
personnel ascertained outcome (mortality) information
directly from patients (or relatives) and physicians. This
information was validated by examination of the state
death registry. Demographic data, including patient age
at diagnosis, gender, race/ethnicity, date of surgery, date
of the last follow-up (if alive), date of recurrence (if any)
and date of death, were collected. Collection of followup
information, performed every six months, ended in
April 2010. Laboratory investigators (VRK & CS-C) were
blinded to the outcome information until completion of the
assays.
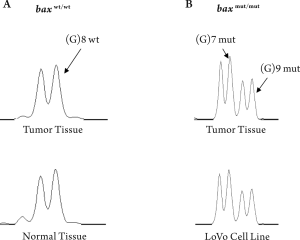
Mutational analysis
Earlier studies have reported a decreased expression of
Bax in CRCs which exhibited mutations in the poly G(8)
region of the bax gene ( 36, 37). Therefore, in this study, we
also analyzed the genomic DNA samples extracted from
CRCs and their corresponding normal tissues to assess the
expression status of Bax in relation to the bax mutational
status. Genomic DNA was extracted from tissue sections
(10-μm thick) of primary CRCs and LoVo cell line as
described ( 38). The 94-base-pair region encompassing
the (G) 8 tract in the bax coding sequence was amplified
by PCR on the CRCs, with carboxyf luorescein (6FAM)-
labeled 5’atccaggatcgagcagggcga-3’ sense primer and 5’
cactcgctcagcttcttggtggac-3’ antisense primer. PCR was
accomplished in a 25-μL reaction volume containing
approximately 100 ng of genomic DNA, a 200-μmol/L
concentration of dNTPs (Invitrogen, Carlsbad, CA), and
0.5 U of Platinum Taq DNA polymerase (Invitrogen).
Amplification consisted of a 15-min denaturation step at
95 oC, followed by 36 cycles of 30 sec at 95 oC, 30 sec at 50
oC, and 30 sec at 72 oC and a final extension step of 5 min at
72 oC. Appropriate dilutions of fluorescent PCR products
were mixed with formamide and carboxy-X-rhodaminelabeled
molecular weight standards (GeneScan-500 ROX,
Applied Biosystems, Foster City, CA), heat denatured, and
run in a 50-cm capillary array containing GS Performance
Optimized Polymer6 (Applied Biosystems), at a voltage of
15kV on the ABI PRISM 3100 Genetic Analyzer (Applied Biosystems). The profiles of PCR products were analyzed
by use of GeneScan 3.1 software (Applied Biosystems).
Numerous normal DNA samples were used to establish
the normal peak size and the profile pattern of the bax gene
fragment. All PCRs with abnormal profiles were repeated
twice, independently, to confirm the presence of mutations.
Immunohistochemistry
Formalin-fixed, paraffin-embedded archival tissues were
collected from the surgical pathology division of the
UAB Hospital. From the blocks, tissue sections (5-μm
thick), representative of normal mucosa and invasive
adenocarcinomas were cut 1 to 2 days before staining to
avoid potential problems in antigen recognition due to
storage of cut sections on glass slides( 39, 40). Sections
were de-paraffinized in xylene and rehydrated in graded
alcohols. For antigen retrieval of Bax and Bcl-2, the slides
were microwave boiled in citrate buffer (10 mmol/L, pH
6.0) for 7 min. For p53, antigen retrieval is not required
( 8, 41, 42). Endogenous peroxidase activity was quenched
with 3% hydrogen peroxide for 5 min. Non-specific binding
of the primary antibodies was blocked by incubating the
slides in 3% goat serum at room temperature for 1 hr in
humidity chambers with the primary mouse monoclonal
antibodies for Bax (Clone B9, Santa Cruz Biotechnology
Inc, CA, USA) (1:200), Bcl-2 (Clone 124, Roche Diagnostic
corporation, Indianapolis, IN, USA) (1:60) and p53
(Clone BP53, BioGenex, San Ramon, CA, USA) (1:80). A
biotin-streptavidin horseradish peroxidase detection kit
was used as the secondary detection system (BioGenex).
The biotinylated goat anti-mouse secondary and avidinhorseradish
peroxidase label were each applied for 10
min. The antigen-antibody complex was recognized by
incubating with the chromogen, diamino-benzidine, for
7 min. The slides were counterstained with hematoxylin
for 1 min. Known positive controls were included in each
staining run; negative controls were obtained by omitting
the primary antibody. Slides were then dehydrated in
graded alcohols, cleared in 3 xylene baths, and mounted
with Permount™ mounting media. As we reported earlier
( 43), these antigens are stable in paraffin blocks.
Staining evaluation
Stained slides were evaluated under a light microscope,
and the staining was scored semi-quantitatively by CS-C,
NCJ and UM, CKS together to limit the bias; if there was
a disagreement in their scores, they reached to a consensus
before proceeding. Obser vers were bl inded for the
clinicopathologic data and the treatment status. Phenotypic
expression of Ba x and Bcl-2 was present in the cell
cytoplasm and accumulation of p53 in the nucleus (p53 nac). As described earlier ( 8, 9, 12, 13), the percentage of positive
cells and staining intensity were taken into consideration
for estimation of the final immunostaining score (ISS). The
intensity of staining of individual cells was scored on a scale
of 0 (no staining) to + 4.0 (strong staining). In addition,
each reviewer estimated the proportion of cells stained
at each intensity level. The percentage of cells and the
corresponding intensity were then multiplied to obtain the
ISS. For each case, the final ISS was the average of the values
estimated by these three investigators.
Cutoff values
Molecular marker expression was dichotomized into high
expressors and low expressors, based on the cut-off values
discussed below. For Bax expression, the median ISS (1.8) of
tumor tissues was taken as the cut-off value; i.e., the tumors
expressing ≥ 1.80 were considered as “high expressors”
(equivalent to > +1 of routine immunohistochemistry,
IHC, scoring in the diagnostic pathology setting) and those
CRCs with ISS 27, 44, 45). For
Bcl-2 expression, based on prior studies by us and others
( 8), we chose 0.5 ISS as the cut-off value. We considered
only tumor cells with distinct nuclear immunostaining for
p53 as positive and considered the tumor positive only if
there was ≥10% positivity of all malignant cells in a tissue
section, as described earlier ( 9). We chose this cutoff
because, at this value, there was the highest concordance
between immunohistochemical detection of p53 nac and
point mutations of the p53 gene detected by single-strand
confirmation polymorphism and DNA sequencing analyses.
At this cutoff value, IHC detects 95% of point mutations
in the p53 gene ( 42). The cut-off value for Bax/Bcl-2 ratio
was based on their levels of expression in benign colonic
epithelium. We used the ISS values of Bax and Bcl-2 to
determine the Bax/Bcl-2 ratio of each case, then a median
value of 0.25 was obtained. This 0.25 value was used as a
cut-off for Bax/Bcl-2 ratio to dichotomize CRCs into groups
of “high” and “low” ratios.
Statistical analysis
Correlations between biomarkers and clinical response
(overall survival) were evaluated by chi-square tests. The
type-I error rate of each test was controlled at < 0.05. All
analyses were performed with SAS statistical software,
version 9.0 ( 46). Kaplan-Meier curves and log-rank tests
were used to assess the effect of the selected biomarkers in
univariate analyses ( 47). Overall survival was estimated
as the number of months from surgery to the date of death
or last contact. Patients who were alive at last contact and those who died due to a cause other than colorectal cancer
were “right censored.” Only those deaths due to CRCs
were considered as events. Multivariate Cox proportional
hazards tests ( 48) were utilized to identify the independent
prognostic value of molecules indicators of survival, after
controlling for patient age, gender, race, tumor location,
tumor size, tumor stage, tumor grade, and the three
molecular markers, Bax, Bcl-2, and p53 nac. Models were built
separately for each patient group (the group of patients who
received chemotherapy after surgery and the group who
underwent surgery without any pre- or post-surgery chemoor
radiation therapy).
|
|
Results
Demographic and clinicopathologic characteristics of the
patient population
Table 1 shows the patient distribution; their demographic,
clinicopathological and molecular characteristics; and their
correlation with survival. For both treatment groups, there
were similar distributions of patient age, gender, ethnicity,
tumor stage, tumor location, tumor size, and tumor grade,
in terms of deaths due to CRC. The median follow-up
period of the complete study population of 112 patients was
9.31 years (range < 1 – > 20 years).
Survival analysis based on treatment
Univariate Kaplan-Meier survival analysis demonstrated
no significant differences in overall survival rates between
the surgery-alone and the 5-FU-treated patient groups (log
rank, P=0.71) (data not shown).
Bax (G) 8 mutation frequency and its relation to clinicopathologic
features
We analyzed for the presence of mutations in the (G) 8
tract of the Bax gene in a human CRC cell line (LoVo) and
in 83 CRCs. The LoVo cells displayed a bi-allelic Bax (G) 8
frame-shift mutation; this status was used as a reference in
CRCs for Bax mutations (Fig 1). In our analysis, 23 of 83
(28%) CRCs demonstrated biallelic Bax (G) 8 frame-shift
mutations. The majority of CRCs with mutations at the G
(8) tract also had low Bax expressing (20 of 23, 87%). CRCs
that displayed these mutations were significantly higher
for male patients (17 of 23, 74%) and distal tumors (18 of
23, 79%). However, there was no association between the
presence of Bax (G) 8 mutations with age, race/ethnicity,
depth of wall infiltration, tumor grade, tumor stage, lymph
node invasion, or presence of distant metastasis (data not
shown). Since the number of CRCs with Bax mutations is
small, we have not further analyzed the mutational data
to assess correlation between Bax mutations and patient survival in the surgery alone and surgery and 5-FU therapy
patient groups separately.
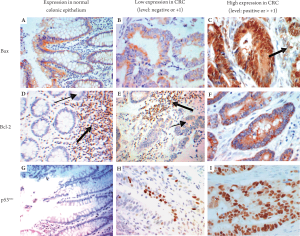
Bax immunophenotypic expression analysis
Immunoreactivity for Bax was observed in the cytoplasm.
In most CRCs, the Bax staining pattern was homogenous,
ranging from low to high levels. In 11% of CRCs (12
cases), however, there was intratumoral heterogeneity. A
low level of Bax expression was observed consistently in
benign colonic epithelium, lymphocytes, and endothelial
cells (Fig 2A-C). The presence of staining in intra-tumoral
lymphocytes was used as an internal positive control. Of the
CRCs, 54% (60 of 112) had high levels of Bax expression
(22 of the 5-FU treated group and 38 of the surgeryalone
group). Twelve of 28 surgery-alone patients (43%)
with low Bax expression died due to CRCs; 19 of 34 5-FU
treated patients (56%) with low Bax expression died due
to CRCs (Table 1). There was no association between Bax
expression and p53nac in either patient group (data not
shown). CRCs with negative or low Bax immunostaining
were significantly associated with CRCs that demonstrated
frame-shift mutations at the Bax (G) 8 tract (20 of 23, 87%)
as compared to CRCs without this mutation (25 of 60,
41%) (data not shown). In addition, most CRCs with poor
differentiation had low Bax expression in the surgery-alone
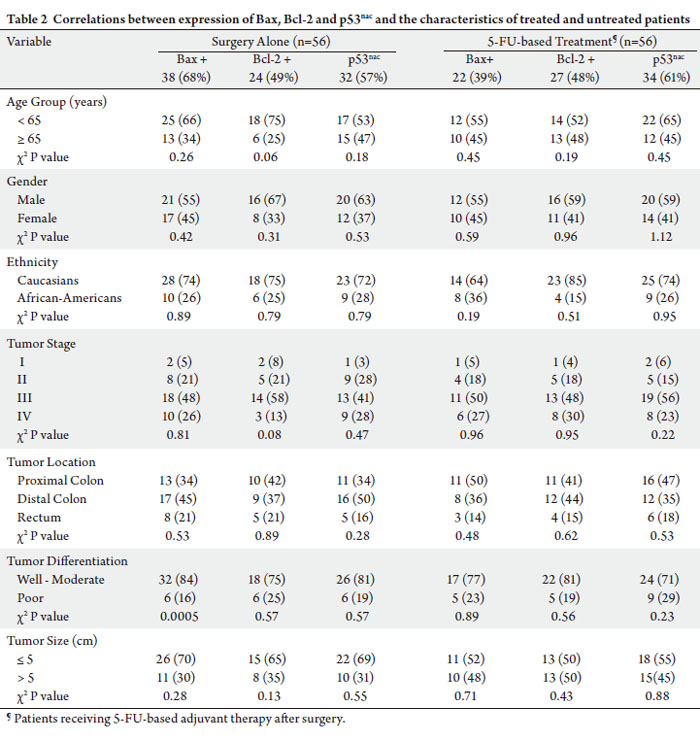
group (χ2, P= 0.0005) (Table 2).
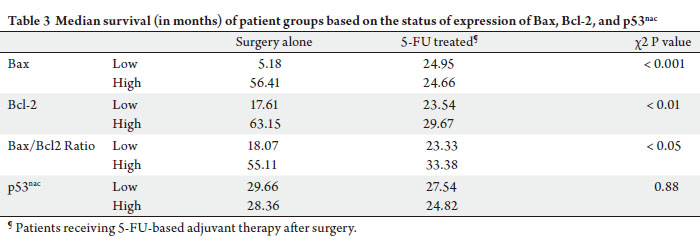
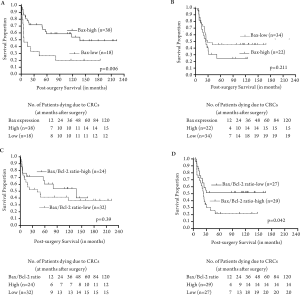
The median survival of the 5-FU treated group of
patients with low Bax expression was 25 months relative to
5 months for surgery-alone patients with low Bax expression
(Table 3). The median survival for 5-FU treated patients
with high Bax expression was 25 months relative to 56
months for surgery-alone patients with high Bax expression
(Table 3). Kaplan-Meier analyses demonstrated a significant
association between high Bax expression and better patient
survival in the surgery-alone group (log rank P=0.006) (Fig
3A). Although there was no significant association between
Bax expression status and patient survival in the 5-FU
treated group, patients with decreased Bax expression had
improved survival (overall log rank P=0.211) (Fig 3B).
Bcl-2 immunophenotypic expression analysis
Immunoreactivity for Bcl-2 was localized in the cytoplasm;
overall, the staining was homogenous. The staining in
intra-tumoral lymphocytes was used as an internal control
(Fig 2D-F). Of the patients, 46% had high levels of Bcl-2
expression (27 5-FU-treated patients and 24 surgeryalone
patients). There were no significant differences in the
incidence of deaths due to CRCs in the Bcl-2 low and high
expressors of among the 5-FU-treated or surgery-alone
patients (Table 1). However, the median survival was higher
(63.15 months) for surgery-alone patients with high levels of
Bcl-2 expression as compared to those with low expression
(17.61 months). There was no significant difference in the
median survival of 5-FU treated patients with low or high
Bcl-2 expression (Table 3).
Univariate Kaplan-Meier survival analysis demonstrated
no statistically significant differences in survival of patients
with or without Bcl-2 expression in the surgery-alone
group (overall log rank P=0.431) or the 5-FU-treated group
(overall log rank P=0.112) (data not shown).
Bax/Bcl2 expression ratio
For each patient, the ratio of Bax/Bcl2 expression was
determined and correlated with patient survival separately
for each treatment categor y. The ratio of Ba x/Bcl2
expression was not correlated with patient survival in
surgery alone category (Fig 3C). In contrast, the ratio of
Bax/Bcl2 expression significantly correlated with patient
survival, indicating that those patients with a high Bax/
Bcl2 ratio value would not benefit from 5-FU treatment;
however, those patients with low Bax/Bcl2 ratios were more
likely to have better survival when treated with 5-FU based
therapies (Fig 3D).
Analysis of nuclear accumulation of p53
Expression of p53nac was generally homogenous; however,
p53 staining was observed in the cytoplasm of malignant cells in 7% of cases (8 of 112) (Fig 2G-I). The cytoplasmic
staining was not further analyzed. High levels of p53nac were
found in tumors of 59% of patients (33 5-FU-treated and 32
surgery-alone). For both categories of patients, there were no
significant differences in the incidence of deaths due to CRCs
(Table 1), in the median survival (Table 3), or survival rates
(data not shown) in relation to p53nac (Table 1).
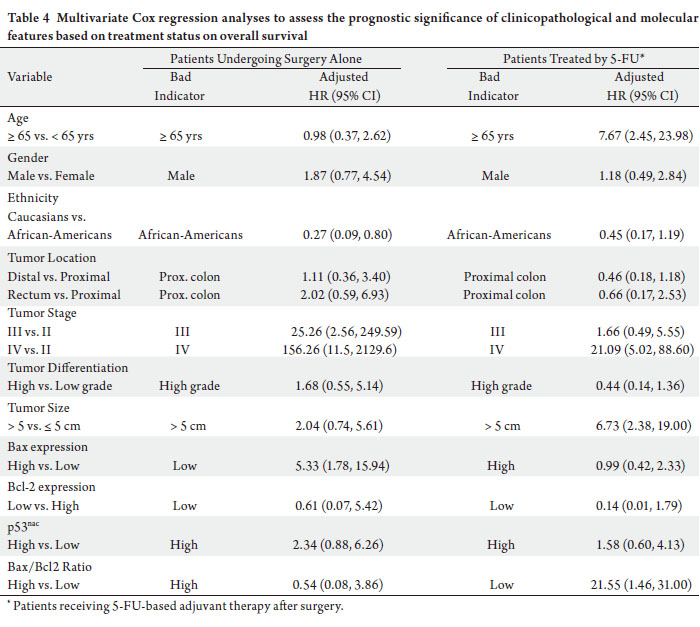
Multivariate survival analyses
As determined by multivariate analyses of Cox proportional hazards, surgery-alone patients with low Bax expression had
5.33 times higher mortality compared to those with high
Bax expression (HR: 5.33; CI: 1.78-15.94) when adjusted
for demographic and clinicopathological variables and for
expression Bcl-2, the Bax/Bcl2 ratio, and p53nac (Table 4).
5-FU treated patients with low Bax/Bcl2 ratios had 21.55
times higher mortality compared to those with high Bax/
Bcl2 ratios (HR: 21.55; CI: 1.46-31.00), when adjusted for
other variables (Table 4). Bcl-2 and p53nac, however, were
not independent prognostic indicators of survival in either group of patients (Table 4).
|
|
Discussion
The current study, we analyzed the predictive value of Bax,
Bcl-2, and p53nac and determined their association with
survival in CRC patients who received 5-FU-based adjuvant
treatment after surgery and in CRC patients matched for
age, gender, ethnicity, tumor stage, tumor location, and
tumor differentiation who underwent surgery alone with curative or palliative intent. These analyses demonstrate a
better survival of patients who received chemotherapy when
their CRCs lacked Bax expression. In contrast, patients with
CRCs that exhibited high Bax expression had worse survival
when they received 5-FU-based adjuvant chemotherapy.
Furthermore, multivariate Cox regression analysis showed
that surgically treated patients with low levels (or lack) of
Bax expression had 5.33 times higher mortality than those
with high Bax expression, after adjusting for confounding
variables, including tumor stage. Bcl-2 or p53nac had no predictive value in either group of patients. These findings
are the first to indicate that patients with CRCs that lack or
express low levels of Bax, but not those with high expression,
benefit from 5-FU-based adjuvant therapies. Analysis of a
large sample set, however, could provide more definitive
information.
Although the current evaluation was performed in
a retrospective setting, and the sample was small, the
inclusion and exclusion criteria and the sample matching
method, described in the Material and Methods section,
minimizes the risk of error and provides strength to the
findings. By including only those patients who completed
at least 3 months of treatment when on continuous infusion
regimens or 6 months when on bolus regimens, and
excluding all patients who received any kind of treatment
prior to surgery, we lowered the potential errors from
using a population from different protocols and different
physicians.
Although several studies have been performed to identify
potential predictive markers of 5-FU for CRC treatment,
the results are inconclusive ( 16-18, 49). 5-FU and other
chemotherapeutic agents may cause death of cancer cells by
inducing apoptosis. Since apoptosis can be initiated either
in the mitochondria by activation of the caspases cascade or
by the induction of p53 and apoptotic molecules such as Bax
and Bcl-2, we assessed the prognostic and predictive value
of expression of Bax and Bcl-2 and p53 nac. Relative to p53, Bax is downstream and can act
synergistically with p53, but it does not completely depend
on p53 to function in apoptosis ( 27, 28). Furthermore,
the efficacy of Bax in predicting response or resistance
to chemotherapy and apoptosis is tissue-specific ( 28).
In agreement with previous studies ( 28, 50) the current
investigation demonstrated that Bax expression in CRCs
is not associated with the status of p53 nac; however, Bax
expression has both predictive and prognostic value. The
findings that the patients with CRCs expressing high
levels of Bax had a better survival than those with low Bax
expression, particularly in patients who have undergone
surgery alone, are consistent with several other earlier
studies of CRCs ( 27, 51-53) and other human malignancies
( 44, 54). Although it was not significant, the predictive role
of Bax expression was evident in our observation that
patients with low Bax expression who received 5-FU-based
adjuvant therapy had a longer survival than those patients
with high Bax expression, showing that patients with low
Bax expression have an apparent benefit from 5-FU-based
adjuvant therapy. An earlier analysis involving patients with
advanced CRCs (recurrent or metastatic) who received
methotrexate plus 5-FU demonstrated a similar trend in an association between Bax expression and overall survival, as
the median survival for low expressors of Bax was 9 months
compared to 14 months for high expressors ( 55). For a group
of patients subjected to preoperative radiochemotherapy for
locally advanced rectal carcinoma, however, there was no
correlation between the level of Bax expression and tumor
recurrence ( 56). Contrary to our findings, results of studies performed
in vitro demonstrate that CRC cell lines with high Bax
expression responded well to long-term 5-FU exposure,
which induced apoptosis ( 57, 58). Additionally, studies
performed in vitro have indicated that antioxidants, such
as N-acetylcysteine and vitamin E, are required to augment
Bax expression to elicit 5-FU-induced apoptosis ( 59).
Nevertheless, there were no such findings in clinical studies
or in experimental studies performed in vivo. Based on
our findings, however, the low levels of Bax may exert less
intrinsic resistance to the complex cascade of intracellular
signals of apoptotic pathways triggered by chemotherapeutic
agents. Thus, there are apparently distinct mechanisms of
Bax involvement in the manifestation of apoptosis. Molecular markers have different functional roles, similar
to the Bax expression observed here. A recent investigation
by Tsuji et al ( 60) demonstrated that high expression of
dihydropyrimidine dehydrogenase (DPD) in Stage II and
III CRCs was an effective indicator of oral 5-FU-based
adjuvant therapy; however, low expression of tumor DPD
predicted poor survival for patients undergoing surgery
alone. The prognostic value of high Bax expression observed
for the surgery-alone group might be useful for a sub-set
of Stage I and Stage II patients; in contrast, the predictive
value of Bax expression might be useful in predicting the
efficacy of 5-FU-based therapy, particularly for patients
with advanced stage disease (Stage III or IV), who routinely
receive 5-FU-based adjuvant therapy. Larger studies
determining the clinical usefulness of Bax expression in
CRCs according to pathologic stage may confirm these
findings. In the current investigation, increased Bcl-2 expression
in CRCs was not predictive of 5-FU-based adjuvant
therapy; however, increased Bcl-2 expression was an
indicator of prolonged survival for patients who had surgery
alone. The prognostic value of Bcl-2 expression in CRCs
has been demonstrated ( 8, 61). The association between
increased Bcl-2 expression and patient overall survival was
stronger in early-stage CRCs ( 62-64) and for CRCs located
in the distal colorectum ( 11). Similar to our findings, other
studies demonstrated that, for patients receiving 5-FUbased
chemotherapy, Bcl-2 expression did not inf luence
response to chemotherapy and did not affect overall
survival( 55, 65, 66). Our multivariate survival analysis, however, demonstrated a better survival of patients whose
tumors had low a Bax/Bcl-2 ratio (i.e., Bax was low) and who
received 5-FU-based adjuvant chemotherapy. Furthermore,
the expression of these two apoptotic markers was not
associated with p53 nac. Similar to our findings, Mirjolet et
al ( 67) and Violette et al ( 58) demonstrated, by experiments
performed in vitro, that 5-FU sensitivity is independent of
p53. The current findings support the premise that patients
with CRCs expressing high levels of Bax should not be
considered for 5-FU-based adjuvant chemotherapy. These
results indicate that the balance between pro-apoptotic
and anti-apoptotic markers has a function in the response
to therapy. Nevertheless, large prospective studies are
required to provide further information useful for making
therapeutic decisions. p53 has been considered to be a prognost ic and
predictive marker, and it has been established as an
important prognostic indicator, specifically for non-
Hispanic Caucasian patients with tumors located in the
proximal colon ( 9). As anticipated, p53 nac was not useful
in predicting the overall survival of patients receiving
surger y alone, because these two cohorts consist of
tumors from all anatomic locations of the colorectum,
and from African Americans and non-Hispanic Caucasians. The current report demonstrates that p53 nac is not useful
in predicting the response to 5-FU-based adjuvant therapy.
Several studies have shown that p53 has a function in
chemotherapy-induced apoptosis and is a predictor of 5-FUbased
adjuvant therapy response in CRCs ( 68); others did
not find such an association ( 58, 67, 69). These conflicting
findings may be due to the admixture of patient populations
for ethnicity, tumor stage, or tumor location, as has been
observed in the evaluation of p53 nac for its prognostic value
( 9). Other reasons for these conf licting results could be
the technical variations in detecting p53 nac, including the
antigen enhancement methods and antibodies used or the
choice of cut-off values considered for tumor positivity for
abnormal p53 expression ( 8). The predictive capacity of p53
in CRCs remains controversial. Findings of the current investigation show that, for the
surgery-alone group, high Bax expression is associated with
better survival. Although statistically not significant, low
Bax expression in the 5-FU-based adjuvant chemotherapy
group was associated with improved survival. Further, these
data reveal that patients with low Bax/Bcl2 expression ratios
would benefit from 5-FU-based adjuvant therapy. Findings
from the present proof-of-principle studies provide evidence
that phenotypic expression of Bax and Bcl-2 predict the
response to 5-FU-based adjuvant therapy in CRCs. Future
prospective studies will assess the clinical utility of these markers.
|
|
Acknowledgements
We thank Dr. Donald Hill, Division of Preventive Medicine,
University of Alabama at Birmingham, for his critical
comments.
|
|
References
- Boyle P, Leon ME. Epidemiology of colorectal cancer. Br Med Bull
2002;64:1-25.[LinkOut]
- Sun W, Haller DG. Chemotherapy for colorectal cancer. Hematol Oncol
Clin North Am 2002;16:969-94.[LinkOut]
- Van Cutsem E, Dicato M, Wils J, Cunningham D, Diaz-Rubio E,
Glimelius B, et al. Adjuvant treatment of colorectal cancer (current
expert opinion derived from the Third International Conference:
Perspectives in Colorectal Cancer, Dublin, 2001). Eur J Cancer
2002;38:1429-36.[LinkOut]
- Conley BA, Kaplan RS, Arbuck SG. National cancer institute clinical
trials program in colorectal cancer. Cancer Chemother Pharmacol
1998;42:S75-9.[LinkOut]
- Simmonds PC. Palliative chemotherapy for advanced colorectal cancer:
systematic review and meta-analysis. Colorectal Cancer Collaborative
Group. BMJ 2000;321:531-5.[LinkOut]
- Ragnhammar P, Hafstrom L, Nygren P, Glimelius B. A systematic
overview of chemotherapy effects in colorectal cancer. Acta Oncol
2001;40:282-308.[LinkOut]
- Wang Y, Jatkoe T, Zhang Y, Mutch MG, Talantov D, Jiang J, et al. Gene
expression profiles and molecular markers to predict recurrence of
Dukes' B colon cancer. J Clin Oncol 2004;22:1564-71.[LinkOut]
- Manne U, Myers RB, Moron C, Poczatek RB, Di l lard S, Weiss
H, et a l . Prognostic significance of Bcl-2 expression and p53
nuclear accumulation in colorectal adenocarcinoma. Int J Cancer
1997;74:346-58.[LinkOut]
- Manne U, Weiss HL, Myers RB, Danner OK, Moron C, Srivastava
S, et al. Nuclear accumulation of p53 in colorectal adenocarcinoma:
prognostic importance differs with race and location of the tumor.
Cancer 1998;83:2456-67.[LinkOut]
- Manne U, Weiss HL, Grizzle WE. Racial differences in the prognostic
usefulness of MUC1 and MUC2 in colorectal adenocarcinomas. Clin
Cancer Res 2000;6:4017-25.[LinkOut]
- Manne U, Weiss HL, Grizzle WE. Bcl-2 expression is associated with
improved prognosis in patients with distal colorectal adenocarcinomas.
Int J Cancer 2000;89:423-30.[LinkOut]
- Manne U, Jhala NC, Jones J, Weiss HL, Chatla C, Meleth S, et
al. Prognostic significance of p27(kip-1) expression in colorectal
adenocarcinomas is associated with tumor stage. Clin Cancer Res
2004;10:1743-52.[LinkOut]
- Manne U, Gary BD, Oelschlager DK, Weiss HL, Frost AR, Grizzle
WE. Altered subcellular localization of suppressin, a novel inhibitor of cell-cycle entry, is an independent prognostic factor in colorectal
adenocarcinomas. Clin Cancer Res 2001;7:3495-503.[LinkOut]
- Grizzle WE, Manne U, Jhala N, Weiss H. The molecular characterization
of colorectal neoplasia in translational research. Arch Path & Lab Med
2001;125:91-8.[LinkOut]
- Nehls O, Okech T, Hsieh CJ, Enzinger T, Sarbia M, Borchard F, et al.
Studies on p53, BAX and Bcl-2 protein expression and microsatellite
instability in stage III (UICC) colon cancer treated by adjuvant
chemotherapy: major prognostic impact of proapoptotic BAX. Br J
Cancer 2007;96:1409-18.[LinkOut]
- Maughan NJ, Quirke P. Pathology--a molecular prognostic approach.
Br Med Bull 2002;64:59-74.[LinkOut]
- Duffy MJ, van Dalen A, Haglund C, Hansson L, Klapdor R, Lamerz
R, et al. Clinical utility of biochemical markers in colorectal cancer:
European Group on Tumour Markers (EGTM) guidelines. Eur J Cancer
2003;39:718-27.[LinkOut]
- Bast RC Jr, Ravdin P, Hayes DF, Bates S, Fritsche H Jr, Jessup JM, et al.
2000 update of recommendations for the use of tumor markers in breast
and colorectal cancer: clinical practice guidelines of the American
Society of Clinical Oncology. J Clin Oncol 2001;19:1865-78.[LinkOut]
- Lane DP. Cancer. p53, guardian of the genome. Nature 1992;358:15-6.[LinkOut]
- Yang B, Eshleman JR, Berger NA, Markowitz SD. Wild-type p53 protein
potentiates cytotoxicity of therapeutic agents in human colon cancer
cells. Clin Cancer Res 1996;2:1649-57.[LinkOut]
- Lenz HJ, Hayashi K, Salonga D, Danenberg KD, Danenberg PV,
Metzger R, et al. p53 point mutations and thymidylate synthase
messenger RNA levels in disseminated colorectal cancer: an analysis of
response and survival. Clin Cancer Res 1998;4:1243-50.[LinkOut]
- Allegra CJ, Parr AL, Wold LE, Mahoney MR, Sargent DJ, Johnston P, et
al. Investigation of the prognostic and predictive value of thymidylate
synthase, p53, and Ki-67 in patients with locally advanced colon cancer.
J Clin Oncol 2002;20:1735-43.[LinkOut]
- Allegra CJ, Paik S, Colangelo LH, Parr AL, Kirsch I, Kim G, et al.
Prognostic value of thymidylate synthase, Ki-67, and p53 in patients
with Dukes’ B and C colon cancer: a National Cancer Institute-National
Surgical Adjuvant Breast and Bowel Project collaborative study. J Clin
Oncol 2003;21:241-50.[LinkOut]
- Elsaleh H, Powell B, Soontrapornchai P, Joseph D, Goria F, Spry
N, et al. p53 gene mutation, microsatellite instability and adjuvant
chemotherapy: impact on survival of 388 patients with Dukes’ C colon
carcinoma. Oncology 2000;58:52-9.[LinkOut]
- Fridman JS, Lowe SW. Control of apoptosis by p53. Oncogene
2003;22:9030-40.[LinkOut]
- Lowe SW, Ruley HE, Jacks T, Housman DE. p53-dependent apoptosis
modulates the cytotoxicity of anticancer agents. Cell 1993;74:957-67.[LinkOut]
- Sturm I, Köhne CH, Wolff G, Petrowsky H, Hillebrand T, Hauptmann
S, et al. Analysis of the p53/BAX pathway in colorectal cancer: low BAX
is a negative prognostic factor in patients with resected liver metastases.
J Clin Oncol 1999;17:1364-74.[LinkOut]
- McCurrach ME, Connor TM, Knudson CM, Korsmeyer SJ, Lowe SW.
bax-deficiency promotes drug resistance and oncogenic transformation by attenuating p53-dependent apoptosis. Proc Natl Acad Sci U S A
1997;94:2345-9.[LinkOut]
- Chresta CM, Masters JR, Hickman JA. Hypersensitivity of human
testicular tumors to etoposide-induced apoptosis is associated with
functional p53 and a high Bax:Bcl-2 ratio. Cancer Res 1996;56:1834-41.[LinkOut]
- Eliopoulos AG, Kerr DJ, Herod J, Hodgkins L, Krajewski S, Reed JC,
et al. The control of apoptosis and drug resistance in ovarian cancer:
influence of p53 and Bcl-2. Oncogene 1995;11:1217-28.[LinkOut]
- Koshiji M, Adachi Y, Taketani S, Takeuchi K, Hioki K, Ikehara
S. Mechanisms underlying apoptosis induced by combination of
5-fluorouracil and interferon-gamma. Biochem Biophys Res Commun
1997;240:376-81.[LinkOut]
- WHO. International classification of diseases for oncology. In: 1990;
Geneva: World Health Organization; 1990.
- Purdie CA, Piris J. Histopathological grade, mucinous differentiation
and DNA ploidy in relation to prognosis in colorectal carcinoma.
Histopathology 2000;36:121-6.[LinkOut]
- Compton CC, Fielding LP, Burgart LJ, Conley B, Cooper HS, Hamilton
SR, et al. Prognostic factors in colorectal cancer. College of American
Pathologists Consensus Statement 1999. Arch Pathol Lab Med
2000;124:979-94.[LinkOut]
- Green FL, Page DL, Fleming ID, Fritz A, Balch CM, Haller DG, et al.
AJCC cancer staging handbook: From the AJCC cancer staging manual.
6th ed. New York: Springer-Verlag; 2006.
- Jansson A, Sun XF. Bax expression decreases significantly from primary
tumor to metastasis in colorectal cancer. J Clin Oncol 2002;20:811-6.[LinkOut]
- Sturm I, Köhne CH, Wolff G, Petrowsky H, Hillebrand T, Hauptmann
S, et al. Analysis of the p53/BAX pathway in colorectal cancer: low BAX
is a negative prognostic factor in patients with resected liver metastases.
J Clin Oncol 1999;17:1364-74.[LinkOut]
- Fredricks DN, Relman DA. Paraffin removal from tissue sections for
digestion and PCR analysis. Biotechniques 1999;26:198-200.[LinkOut]
- Jacobs TW, Prioleau JE, Stillman IE, Schnitt SJ. Loss of tumor markerimmunostaining
intensity on stored paraffin slides of breast cancer. J
Natl Cancer Inst 1996;88:1054-9.[LinkOut]
- Prioleau J, Schnitt SJ. p53 antigen loss in stored paraffin slides. N Engl J
Med 1995;332:1521-2.[LinkOut]
- Baas IO, van den Berg FM, Mulder JW, Clement MJ, Slebos RJ,
Hamilton SR, et al. Potential false-positive results with antigen
enhancement for immunohistochemistry of the p53 gene product in
colorectal neoplasms. J Pathol 1996;178:264-7.[LinkOut]
- Grizzle WE, Myers RB, Manne U, Srivastava S. Immunohistochemical
evaluation of biomarkers in prostatic and colorectal neoplasia. In:
Hanausek M, Walaszek Z, editors. John Walker's methods in molecular
medicine-tumor marker protocols. Totowa: Humana Press; 1998. p.
143-60.
- Manne U, Myers RB, Srivastava S, Grizzle WE. Re: loss of tumor
marker-immunostaining intensity on stored paraffin slides of breast
cancer. J Natl Cancer Inst 1997;89:585-6.[LinkOut]
- Krajewski S, Blomqvist C, Franssila K, Krajewska M, Wasenius VM,
Niskanen E, et al. Reduced expression of proapoptotic gene BAX is associated with poor response rates to combination chemotherapy and
shorter survival in women with metastatic breast adenocarcinoma.
Cancer Res 1995;55:4471-8.[LinkOut]
- Miquel C, Borrini F, Grandjouan S, Aupérin A, Viguier J, Velasco V,
et al. Role of bax Mutations in Apoptosis in Colorectal Cancers With
Microsatellite Instability. Am J Clin Pathol 2005;123:1-9.[LinkOut]
- Allison P. Survival analysis using the SAS system: A practical guide.
Cary, NC: SAS Institute Inc;1995.
- Kaplan E, Meier P. Non-parametric estimation from incomplete
observations. J Am Stat Assoc 1958;53:457-48.[LinkOut]
- Cox DR . Regression models and life tables . J Roy Stat Soc
1972;34:187-220.
- Allen WL, Johnston PG. Role of genomic markers in colorectal cancer
treatment. J Clin Oncol 2005;23:4545-52.[LinkOut]
- De Angelis PM, Stokke T, Thorstensen L, Lothe RA, Clausen OP.
Apoptosis and expression of Bax, Bcl-x, and Bcl-2 apoptotic regulatory
proteins in colorectal carcinomas, and association with p53 genotype/
phenotype. Mol Pathol 1998;51:254-61.[LinkOut]
- Ogura E, Senzaki H, Yamamoto D, Yoshida R, Takada H, Hioki K, et al.
Prognostic significance of Bcl-2, Bcl-xL/S, Bax and Bak expressions in
colorectal carcinomas. Oncol Rep 1999;6:365-9.[LinkOut]
- Schelwies K, Sturm I, Grabowski P, Scherübl H, Schindler I, Hermann
S, et al. Analysis of p53/BAX in primary colorectal carcinoma: low BAX
protein expression is a negative prognostic factor in UICC stage III
tumors. Int J Cancer 2002;99:589-96.[LinkOut]
- Nehls O, Hass HG, Okech T, Zenner S, Hsieh CJ, Sarbia M, et al.
Prognostic implications of BAX protein expression and microsatellite
instability in all non-metastatic stages of primary colon cancer treated
by surgery alone. Int J Colorectal Dis 2009;24:655-63.[LinkOut]
- Sturm I, Petrowsky H, Volz R, Lorenz M, Radetzki S, Hillebrand T, et
al. Analysis of p53/BAX/p16(ink4a/CDKN2) in esophageal squamous
cell carcinoma: high BAX and p16(ink4a/CDKN2) identifies patients
with good prognosis. J Clin Oncol 2001;19:2272-81.[LinkOut]
- Paradiso A, Simone G, Lena MD, Leone B, Vallejo C, Lacava J, et
al. Expression of apoptosis-related markers and clinical outcome in
patients with advanced colorectal cancer. Br J Cancer 2001;84:651-8.[LinkOut]
- Tannapfel A, Nusslein S, Fietkau R, Katalinic A, Kockerling F,
Wittekind C. Apoptosis, proliferation, bax, bcl-2 and p53 status prior to
and after preoperative radiochemotherapy for locally advanced rectal
cancer. Int J Radiat Oncol Biol Phys 1998;41:585-91.[LinkOut]
- Kobayashi T, Sawa H, Morikawa J, Zhang W, Shiku H. Bax induction
activates apoptotic cascade via mitochondrial cytochrome c release and
Bax overexpression enhances apoptosis induced by chemotherapeutic
agents in DLD-1 colon cancer cells. Jpn J Cancer Res 2000;91:1264-8.[LinkOut]
- Violette S, Poulain L, Dussaulx E, Pepin D, Faussat AM, Chambaz J, et
al. Resistance of colon cancer cells to long-term 5-fluorouracil exposure is correlated to the relative level of Bcl-2 and Bcl-X(L) in addition to Bax
and p53 status. Int J Cancer 2002;98:498-504.[LinkOut]
- Adeyemo D, Imtiaz F, Toffa S, Lowdell M, Wickremasinghe RG,
Winslet M. Antioxidants enhance the susceptibility of colon carcinoma
cells to 5-fluorouracil by augmenting the induction of the bax protein.
Cancer Lett 2001;164:77-84.[LinkOut]
- Tsuji T, Sawa i T, Takeshita H, Nakagoe T, Hidaka S, Atsushi
Nanashima, et al. Tumor dihydropyrimidine dehydrogenase in
stage II and III colorectal cancer: low level expression is a beneficial
marker in oral-adjuvant chemotherapy, but is also a predictor for poor
prognosis in patients treated with curative surgery alone. Cancer Lett
2004;204:97-104.[LinkOut]
- Sinicrope FA, Hart J, Michelassi F, Lee JJ. Prognostic value of bcl-2
oncoprotein expression in stage II colon carcinoma. Clin Cancer Res
1995;1:1103-10.[LinkOut]
- Krajewska M, Kim H, Kim C, Kang H, Welsh K, Matsuzawa S, et al.
Analysis of apoptosis protein expression in early-stage colorectal cancer
suggests opportunities for new prognostic biomarkers. Clin Cancer Res
2005;11:5451-61.[LinkOut]
- Meterissian SH, Kontogiannea M, Al-Sowaidi M, Linjawi A, Halwani
F, Jamison B, et al. Bcl-2 is a useful prognostic marker in Dukes' B colon
cancer. Ann Surg Oncol 2001;8:533-7.[LinkOut]
- Chatla C, Jhala NC, Katkoori VR, Alexander D, Meleth S, Grizzle WE,
et al. Recurrence and survival predictive value of phenotypic expression
of Bcl-2 varies with tumor stage of colorectal adenocarcinoma. Dis
Markers 2005;21:1-10.[LinkOut]
- Rosati G, Chiacchio R, Reggiardo G, De Sanctis D, Manzione L.
Thymidylate synthase expression, p53, bcl-2, Ki-67 and p27 in
colorectal cancer: relationships with tumor recurrence and survival.
Tumour Biol 2004;25:258-63.[LinkOut]
- Schneider HJ, Sampson SA, Cunningham D, Norman AR, Andreyev
HJ, Tilsed JV, et al. Bcl-2 expression and response to chemotherapy in
colorectal adenocarcinomas. Br J Cancer 1997;75:427-31.[LinkOut]
- Mirjolet JF, Barberi-Heyob M, Didelot C, Peyrat JP, Abecassis J, Millon
R, et al. Bcl-2/Bax protein ratio predicts 5-f luorouracil sensitivity
independently of p53 status. Br J Cancer 2000;83:1380-6.[LinkOut]
- Tang R, Wang JY, Fan CW, Tsao KC, Chen HH, Wu CM, et al. p53
is an independent pre-treatment markers for long-term survival in
stage II and III colorectal cancers: an analysis of interaction between
genetic markers and fluorouracil-based adjuvant therapy. Cancer Lett
2004;210:101-9.[LinkOut]
- Ahnen DJ, Feigl P, Quan G, Fenoglio-Preiser C, Lovato LC, Bunn PA
Jr, et al. Ki-ras mutation and p53 overexpression predict the clinical
behavior of colorectal cancer: a Southwest Oncology Group study.
Cancer Res 1998;58:1149-58.[LinkOut]
Cite this article as:
Katkoori V, Suarez-Cuervo C, Shanmugam C, Jhala N, Callens T, Messiaen L, Posey J III, Bumpers H, Meleth S, Grizzle W, Manne U. Bax expression is a candidate prognostic and predictive marker of colorectal cancer. J Gastrointest Oncol. 2010;1(2):76-89. DOI:10.3978/j.issn.2078-6891.2010.019
|