|
Taxanes
Paclitaxel and docetaxel belong to the Taxane family
because of their chemical structures contain a common
three phenols ring. The clinical application of taxanes in the
management of GECs predates their approval by the FDA
for such an indication. It was not until 2006 that docetaxel
received FDA approval for use as a first-line treatment in
therapy-naïve patients with advanced GECs ( 11). Taxanes are di-terpenes produced by the plants of
the genus Taxus (yews). As their name suggests, taxanes
were first derived from natural sources, but now they
are all synthesized artificially. The two most commonly
used taxanes are paclitaxel and docetaxel. Although all
taxanes are currently used to treat patients with GECs,
only docetaxel has an FDA-approved indication for use
in combination with cisplatin and 5-FU to treat patients
with GECs. Paclitaxel and docetaxel both have therapeutic
indications for many solid tumor malignancies. However,
only docetaxel has an FDA-approved indication for the
treatment of advanced GECs. Paclitaxel has FDA-approved
indications as a single agent for second-line therapy for
metastatic ovarian cancer ( 12-16), for adjuvant treatment of
node-positive breast cancer ( 17), and for second-line therapy
for metastatic breast cancer ( 18), as well as for secondline
therapy for Kaposi’s sarcoma ( 19). In combination
with cisplatin, paclitaxel is also indicated as first-line
therapy for metastatic non-small cell lung ( 20) and ovarian
( 21, 22) cancers. Docetaxel was introduced at the end of
the 1990s; it was first approved in 1996 for the treatment of
refractory metastatic breast cancer ( 23-25). Additional FDA
indications for early breast cancers ( 26, 27) and for advanced
non-small cell lung cancer ( 28, 29), prostate cancer ( 30, 31),
and metastatic head and neck cancers came later ( 32).
Paclitaxel
Paclitaxel was originally isolated from the bark of the
Pacific yew tree, Taxus brevifolia. Its chemical structure
was determined in 1971, and its mechanism of action was
elucidated in 1979 ( 33). Paclitaxel is an anti-microtubule
agent that irreversibly binds specifically to the subunit
of the protein tubulin and promotes the assembly of
microtubules. The stabilization of microtubules prevents normal mitotic spindle formation and function. This
disruption of normal spindle function, which is the primary
mechanism of action of paclitaxel ( 34, 35) ultimately results
in chromosome breakage and inhibition of cell replication
and migration. Therefore, paclitaxel inhibits cell replication
by blocking cells in the late G2 and/or M phases of the
cell cycle( 35). Another important mechanism of action of
paclitaxel includes induction of apoptosis via binding to
and subsequently blocking the function of the apoptosis
inhibitor-protein, bcl-2. Pharmacokinetics studies with
paclitaxel have demonstrated that its distribution is a
biphasic process, with values for α and β half-lives of
approximately 20 minutes and 6 hours, respectively ( 33).
True nonlinear pharmacokinetics may have important
clinical implications, particularly in regards to dose
modification, because a small increase in drug exposure
and hence toxicity ( 33). More than 90% of the time,
paclitaxel binds to plasma proteins. Approximately 71% of
an administered dose of paclitaxel is excreted in the stool
via the enterohepatic circulation ( 33). Renal clearance is
minimal, accounting for 14% of the administered dose( 33).
In humans, paclitaxel is metabolized by cytochrome
P-450 (CP-450) mixed-function oxidases. Specifically,
either isoenzymes CYP2C8 and CYP3A4 of CP-450 will
metabolize paclitaxel to hydroxylated 3’ phydroxypaclitaxel
(minor) and 6α-hydroxyplacitaxel (major), as well as to
other forms of dihydroxylated metabolites. Paclitaxel is
typically administered intravenously at a dose of 135-175
mg/m 2 every 21 days ( 33, 36).
Docetaxel
While paclitaxel is a natural product, docetaxel is a semisynthetic
product. Docetaxel inhibits microtubule
disassembly and promotes microtubule stabilization,
leading to disruption of microtubule-mediated cellular
function during cell division, cell cycle arrest at G2/M
transition, and cell death ( 37). Like paclitaxel, docetaxel
induces the activation of several molecular pathways
leading to cellular apoptosis by disorganizing the
microtubule structure ( 38). However, another proposed
mechanism of action of docetaxel is related to its
effect on phospholipase-D (PLD) ( 38). PLD has been
implicated in several physiological processes, such as
membrane trafficking, cytoskeletal reorganization, cell
proliferation, differentiation, survival, and apoptosis ( 38).
Pharmacokinetics studies with docetaxel have demonstrated
a linear pharmacokinetic behavior with a 3-compartment
model. Docetaxel binds to plasma proteins more than 95%
of the time. Its metabolism also occurs via the CYP3A4
isoenzyme CP-450, and within 7 days of administration,
75% is eliminated in feces ( 38). Because most docetaxel is broken down in the liver, a reduced dose is recommended
for patients with hepatic dysfunction, particularly those
with elevated total bilirubin above the upper limit of normal
(ULN) or alkaline phosphatase greater than 2.5 times
ULN plus ALT and/or AST greater than 1.5 times ULN
( 38). Renal impairment or age greater than 75 years are an
indication for docetaxel dose adjustment ( 38). Docetaxel
is typically administered intravenously at a dose of 60-100
mg/m 2 every 21 days ( 33, 39). The most frequent dose-limiting toxicities (DLTs) of
both paclitaxel and docetaxel include myelosuppression,
hypersensitivity reactions, neuropathy, and musculoskeletal
effects. Myelosuppression is both dose- and scheduledependent,
but it is not cumulative, where neutropenia
is the principal DLT. The nadir of myelosuppression is
usually on the 8 th-10 th day and complete bone marrow
recovery is expected on the 15 th-21 th day ( 40). During
its early development and in the initial phase II studies,
docetaxel was administered at a dose of 100 mg/m 2. In
these early studies, neutropenia reached its nadir on the 8 th
day and resolved on the 15 th-21 st days of docetaxel infusion,
and febrile neutropenia requiring hospitalization was
observed in 10-14% of treated patients ( 38). Since its early
development, docetaxel is now administered at a modified
dose of 75 mg/m 2. A significant reduction in febrile
neutropenia frequency was observed with this dose ( 38). Taxane hypersensitivity reactions can be categorized
as type 1 (anaphylactoid) or type 2 (anaphylaxis).
Symptoms of an anaphylactoid reaction include dyspnea,
f lushing, chest pain and tachycardia, where the cause
is a surge of histamine release within 2-3 minutes after
the administration of the drug. Anaphylaxis is more
severe and can even be fatal; symptoms of anaphylaxis
include hypotension, angioedema, and urticaria. Both
types of reaction occur during the first two courses, and
typically begin during the first 15 minutes of the infusion
and resolve 15 minutes prior to the completion of the
infusion. Along with antihistamine premedication, the
administration of a prophylactic regimen consisting of 3-5
days of steroids beginning 1-2 days prior to treatment can
reduce the frequency and severity of a hypersensitivity
reaction ( 38, 40). Once patients have experienced either
type of severe hypersensitivity reaction, the drug is further
contraindicated. Fortunately, the incidence of anaphylaxis
is low, occurring in only 2% of patients receiving paclitaxel
and in 13% of patients receiving docetaxel. Peripheral neuropathy resulting from both axonal
degeneration and demyelination ( 40) is a DLT that is
dose-dependent and cumulative. Mild symptoms relating
to sensory loss usually improve or resolve completely
within several months after discontinuation of therapy. Pre-existing neuropathies are not a contraindication to
treatment. Central neurotoxicity may occur and may be
severe especially with paclitaxel. Myalgia and/or arthralgia
typically appear 2-3 days after drug administration, resolve
within a few days, and are unrelated to dose ( 41, 42).
Docetaxel-associated neuropathy occurs less frequently
and with less severity than paclitaxel-associated neuropathy
( 42). Reversible fluid retention syndrome ( 42, 43), which is
characterized by edema and third-space fluid retention,
is a unique side effect of docetaxel. Bowel wall edema
and pleural and peritoneal fluid retention are common
manifestations of this syndrome, which is caused by a
docetaxel-induced increase in capillary permeability.
The most serve end-organ complication of third-space
fluid collection is heart failure. This severe complication
can be ameliorated and prevented with prophylactic
administration of corticosteroids, along with aggressive and
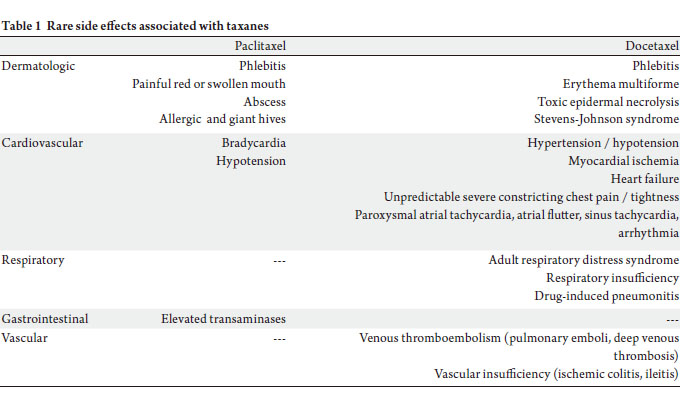
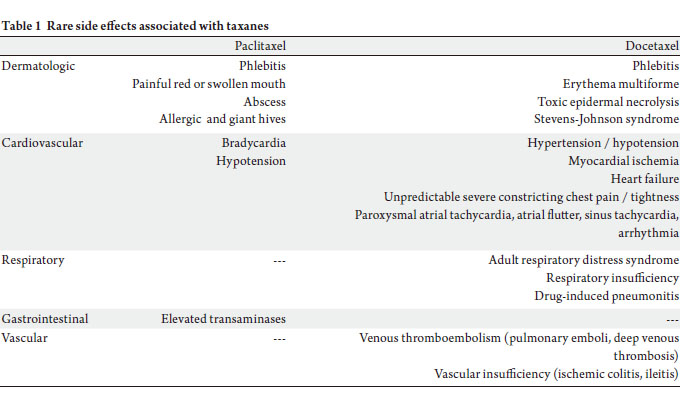
early administration of diuretics ( 43). No less important, but less frequently reported, toxicities
associated with ta xanes include fatigue, mucositis,
gastrointestinal symptoms, phlebitis, drug-induced
adult respiratory distress syndrome (for docetaxel),
and bradycardia plus swollen, red, painful mouth (for
paclitaxel). Fatigue is observed in 58-67% of the patients
treated with docetaxel, and it is occasionally severe enough
to cause a modification in dose ( 33). Mucositis typically
results from slow infusion, and it occurs more frequently
in patients treated with docetaxel than with paclitaxel.
Although less-severe gastrointestinal toxicityties, such as
nausea, vomiting, and diarrhea, also occur more frequently
with docetaxel, grade 3/4 gastrointestinal toxicities are
uncommon ( 42). Table 1 summarizes the rare adverse
effects associated taxanes.
|
|
References
- Jemal A, Center MM, DeSantis C, Ward EM. Global patterns of cancer
incidence and mortality rates and trends. Cancer Epidemiol Biomarkers
Prev 2010;19:1893-907.[LinkOut]
- Devesa SS, Blot WJ, Fraumeni JF Jr. Changing patterns in the incidence
of esophageal and gastric carcinoma in the United States. Cancer
1998;83:2049-53.[LinkOut]
- Alberts SR, Cervantes A, van de Velde CJ. Gastric cancer: epidemiology,
pathology and treatment. Ann Oncol 2003;14:Sii31-6.[LinkOut]
- Macdonald JS, Smalley SR, Benedetti J, Hundahl SA, Estes NC,
Stemmermann GN, et al . Chemoradiotherapy after surgery compared with surgery alone for adenocarcinoma of the stomach or
gastroesophageal junction. N Engl J Med 2001;345:725-30.[LinkOut]
- Cunningham D, Allum WH, Stenning SP, Thompson JN, Van de Velde
CJ, Nicolson M, et al. Perioperative chemotherapy versus surgery alone
for resectable gastroesophageal cancer. N Engl J Med 2006;355:11-20.[LinkOut]
- Boige V, Pignon JP, Saint-Aubert B, Lasser P, Conroy T, Bouché O,
et al. Final results of a randomized trial comparing preoperative
5-fluorouracil (F)/cisplatin (P) to surgery alone in adenocarcinoma of
stomach and lower esophagus (ASLE): FNLCC ACCORD07-FFCD
9703 trial [abstract]. J Clin Oncol 2007;s25:4510.
- Sakuramoto S, Sasako M, Yamaguchi T, Kinoshita T, Fujii M,
Nashimoto A, et al. Adjuvant chemotherapy for gastric cancer with S-1,
an oral fluoropyrimidine. N Engl J Med 2007;357:1810-20.[LinkOut]
- Varadhachary G, Ajani JA. Preoperative and adjuvant therapies
for upper gastrointestinal cancers. Expert Rev Anticancer Ther
2005;5:719-25.[LinkOut]
- Pyrhönen S, Kuitunen T, Nyandoto P, Kouri M. Randomised
comparison of fluorouracil, epidoxorubicin and methotrexate
(FEMTX) plus supportive care with supportive care alone in patients
with non-resectable gastric cancer. Br J Cancer 1995;71:587-91.[LinkOut]
- Varadhachary G, Ajani JA. Gastric cancer. Clin Adv Hematol Oncol
2005;3:118-24.[LinkOut]
- Van Cutsem E, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M,
Boni C, et al. Phase III study of docetaxel and cisplatin plus fluorouracil
compared with cisplatin and f luorouracil as first-line therapy for
advanced gastric cancer: a report of the V325 Study Group. J Clin Oncol
2006;24:4991-7.[LinkOut]
- Cantù MG, Buda A, Parma G, Rossi R, Floriani I, Bonazzi C, et
al. Randomized controlled trial of single-agent paclitaxel versus
cyclophosphamide, doxorubicin, and cisplatin in patients with recurrent
ovarian cancer who responded to first-line platinum-based regimens. J
Clin Oncol 2002;20:1232-7.[LinkOut]
- Paclitaxel and docetaxel in breast and ovarian cancer. Drug Ther Bull
1997;35:43-6.[LinkOut]
- Eisenhauer EA, ten Bokkel Huinink WW, Swenerton KD, Gianni L,
Myles J, van der Burg ME, et al. European-Canadian randomized trial
of paclitaxel in relapsed ovarian cancer: high-dose versus low-dose and
long versus short infusion. J Clin Oncol 1994;12:2654-66.[LinkOut]
- Gore ME, Preston N, A’Hern RP, Hill C, Mitchell P, Chang J, et al.
Platinum-Taxol non-cross resistance in epithelial ovarian cancer. Br J
Cancer 1995;71:1308-10.[LinkOut]
- Trimble EL, Adams JD, Vena D, Hawkins MJ, Friedman MA, Fisherman
JS, et al. Paclitaxel for platinum-refractory ovarian cancer: results
from the first 1,000 patients registered to National Cancer Institute
Treatment Referral Center 9103. J Clin Oncol 1993;11:2405-10.[LinkOut]
- Sparano JA, Wang M, Martino S, Jones V, Perez EA, Saphner T, et al.
Weekly paclitaxel in the adjuvant treatment of breast cancer. N Engl J
Med 2008;358:1663-71.[LinkOut]
- Bishop JF, Dewar J, Toner GC, Smith J, Tattersall MH, Olver IN, et al.
Initial paclitaxel improves outcome compared with CMFP combination
chemotherapy as front-line therapy in untreated metastatic breast
cancer. J Clin Oncol 1999;17:2355-64.[LinkOut]
- Saville MW, Lietzau J, Pluda JM, Feuerstein I, Odom J, Wilson WH,
et al. Treatment of HIV-associated Kaposi’s sarcoma with paclitaxel.
Lancet 1995;346:26-8.[LinkOut]
- Bonomi P, Kim K, Fairclough D, Cella D, Kugler J, Rowinsky E, et al.
Comparison of survival and quality of life in advanced non-small-cell
lung cancer patients treated with two dose levels of paclitaxel combined
with cisplatin versus etoposide with cisplatin: results of an Eastern
Cooperative Oncology Group trial. J Clin Oncol 2000;18:623-31.[LinkOut]
- McGuire WP, Hoskins WJ, Brady MF, Kucera PR, Partridge EE, Look
KY, et al. Cyclophosphamide and cisplatin compared with paclitaxel
and cisplatin in patients with stage III and stage IV ovarian cancer. N
Engl J Med 1996;334:1-6.[LinkOut]
- Piccart MJ, Bertelsen K, James K, Cassidy J, Mangioni C, Simonsen
E, et al. Randomized intergroup trial of cisplatin-paclitaxel versus
cisplatin-cyclophosphamide in women with advanced epithelial ovarian
cancer: three-year results. J Natl Cancer Inst 2000;92:699-708.[LinkOut]
- Nabholtz JM, Senn HJ, Bezwoda WR, Melnychuk D, Deschênes
L, Douma J, et al. Prospective randomized trial of docetaxel versus
mitomycin plus vinblastine in patients with metastatic breast cancer progressing despite previous anthracycline-containing chemotherapy.
304 Study Group. J Clin Oncol 1999;17:1413-24.[LinkOut]
- Chan S, Friedrichs K, Noel D, Pintér T, Van Belle S, Vorobiof D, et
al. Prospective randomized trial of docetaxel versus doxorubicin in
patients with metastatic breast cancer. J Clin Oncol 1999;17:2341-54.[LinkOut]
- Harvey V, Mouridsen H, Semiglazov V, Jakobsen E, Voznyi E, Robinson
BA, et al. Phase III trial comparing three doses of docetaxel for secondline
treatment of advanced breast cancer. J Clin Oncol 2006;24:4963-70.[LinkOut]
- Martin M, Pienkowski T, Mackey J, Pawlicki M, Guastalla JP, Weaver C,
et al. Adjuvant docetaxel for node-positive breast cancer. N Engl J Med
2005;352:2302-13.[LinkOut]
- Hurley J, Doliny P, Reis I, Silva O, Gomez-Fernandez C, Velez P, et al.
Docetaxel, cisplatin, and trastuzumab as primary systemic therapy for
human epidermal growth factor receptor 2-positive locally advanced
breast cancer. J Clin Oncol 2006;24:1831-8.[LinkOut]
- Shepherd FA, Dancey J, Ramlau R, Mattson K, Gralla R, O’Rourke M,
et al. Prospective randomized trial of docetaxel versus best supportive
care in patients with non-small-cell lung cancer previously treated with
platinum-based chemotherapy. J Clin Oncol 2000;18:2095-103.[LinkOut]
- Fossella FV, DeVore R, Kerr RN, Crawford J, Natale RR, Dunphy
F, et al. Randomized phase III trial of docetaxel versus vinorelbine
or ifosfamide in patients with advanced non-small-cell lung cancer
previously treated with platinum-containing chemotherapy regimens.
The TAX 320 Non-Small Cell Lung Cancer Study Group. J Clin Oncol
2000;18:2354-62.[LinkOut]
- Tannock IF, de Wit R, Berry WR, Horti J, Pluzanska A, Chi KN, et
al. Docetaxel plus prednisone or mitoxantrone plus prednisone for
advanced prostate cancer. N Engl J Med 2004;351:1502-12.[LinkOut]
- Berthold DR, Pond GR, Soban F, de Wit R, Eisenberger M, Tannock
IF. Docetaxel plus prednisone or mitoxantrone plus prednisone for
advanced prostate cancer: updated survival in the TAX 327 study. J Clin
Oncol 2008;26:242-5.[LinkOut]
- Posner MR, Hershock DM, Blajman CR, Mickiewicz E, Winquist E,
Gorbounova V, et al. Cisplatin and fluorouracil alone or with docetaxel
in head and neck cancer. N Engl J Med 2007;357:1705-15.[LinkOut]
- Eisenhauer EA, Vermorken JB. The taxoids. Comparative clinical
pharmacology and therapeutic potential. Drugs 1998;55:5-30.[LinkOut]
- Spencer CM, Faulds D. Paclitaxel. A review of its pharmacodynamic and
pharmacokinetic properties and therapeutic potential in the treatment
of cancer. Drugs 1994;48:794-847.[LinkOut]
- Rowinsky EK. Clinical pharmacology of Taxol. J Natl Cancer Inst
Monogr 1993;(15):25-37.[LinkOut]
- Ajani JA, Ilson DH, Kelsen DP. The activity of paclitaxelin
gastrointestinal tumors. Semin Oncol 1995;22:s46-50; discussion 1-3.[LinkOut]
- Tanaka M, Obata T, Sasaki T. Evaluation of antitumour effects of
docetaxel (Taxotere) on human gastric cancers in vitro and in vivo. Eur
J Cancer 1996;32A(2):226-30.[LinkOut]
- Deeks ED, Scott LJ. Docetaxel: in gastric cancer . Drugs
2007;67:1893-901.[LinkOut]
- Pazdur R, Lassere Y, Soh LT, Ajani JA, Bready B, Soo E, et al. Phase II
trial of docetaxel (Taxotere) in metastatic colorectal carcinoma. Ann Oncol 1994;5:468-70.[LinkOut]
- Rowinsky EK, Eisenhauer EA, Chaudhry V, Arbuck SG, Donehower
RC. Clinical toxicities encountered with paclitaxel (Taxol). Semin
Oncol 1993;20:s1-15.[LinkOut]
- Baker J, Ajani J, Scotté F, Winther D, Martin M, Aapro MS, et al.
Docetaxel-related side effects and their management. Eur J Oncol Nurs
2009;13:49-59.[LinkOut]
- Markman M. Management of toxicities associated with the
administration of taxanes. Expert Opin Drug Saf 2003;2:141-6.[LinkOut]
- Piccart MJ, Klijn J, Paridaens R, Nooij M, Mauriac L, Coleman R, et
al. Corticosteroids significantly delay the onset of docetaxel-induced
fluid retention: final results of a randomized study of the European
Organization for Research and Treatment of Cancer Investigational
Drug Branch for Breast Cancer. J Clin Oncol 1997;15:3149-55.[LinkOut]
- Morton RF, Jett JR, McGinnis WL, Earle JD, Therneau TM, Krook
JE, et al. Thoracic radiation therapy alone compared with combined
chemoradiotherapy for locally unresectable non-small cell lung cancer.
A randomized, phase III trial. Ann Intern Med 1991;115:681-6.[LinkOut]
- Adelstein DJ, Saxton JP, Lavertu P, Tuason L, Wood BG, Wanamaker JR,
et al. A phase III randomized trial comparing concurrent chemotherapy
and radiotherapy with radiotherapy alone in resectable stage III and IV
squamous cell head and neck cancer: preliminary results. Head Neck
1997;19:567-75.[LinkOut]
- Al-Sarraf M, LeBlanc M, Giri PG, Fu KK, Cooper J, Vuong T, et al.
Chemoradiotherapy versus radiotherapy in patients with advanced
nasopharyngeal cancer: phase III randomized Intergroup study 0099. J
Clin Oncol 1998;16:1310-7.[LinkOut]
- Kim TY, Yang SH, Lee SH, Park YS, Im YH, Kang WK, et al. A phase III
randomized trial of combined chemoradiotherapy versus radiotherapy
alone in locally advanced non-small-cell lung cancer. Am J Clin Oncol
2002;25:238-43.[LinkOut]
- Lin JC, Jan JS, Hsu CY, Liang WM, Jiang RS, Wang WY. Phase III
study of concurrent chemoradiotherapy versus radiotherapy alone for
advanced nasopharyngeal carcinoma: positive effect on overall and
progression-free survival. J Clin Oncol 2003;21:631-7.[LinkOut]
- Cooper JS, Guo MD, Herskovic A, Macdonald JS, Martenson JA Jr, Al-
Sarraf M, et al. Chemoradiotherapy of locally advanced esophageal
cancer: long-term follow-up of a prospective randomized trial (RTOG
85-01). Radiation Therapy Oncology Group. JAMA 1999;281:1623-7.[LinkOut]
- Ajani JA. Chemotherapy for advanced gastric or gastroesophageal
cancer: defining the contributions of docetaxel. Expert Opin
Pharmacother 2006;7:1627-31.[LinkOut]
- van der Gaast A, van Hagen PM, Hulshof M, Richel D, van Berge
Henegouwen MI, Nieuwenhuijzen GA, et al. Effect of preoperative
concurrent chemoradiotherapy on survival of patients with resectable
esophageal or esophagogastric junction cancer: Results from a
multicenter randomized phase III study [abstract]. J Clin Oncol
2010;s28:4004.
- Ajani J. Therapy of localized esophageal cancer: it is time to reengineer
our investigative strategies. Onkologie 2008;31:360-1.[LinkOut]
- Ajani JA, Komaki R, Putnam JB, Walsh G, Nesbitt J, Pisters PW, et al. A three-step strategy of induction chemotherapy then chemoradiation
followed by surgery in patients with potentially resectable carcinoma of
the esophagus or gastroesophageal junction. Cancer 2001;92:279-86.[LinkOut]
- Ajani JA, Mansfield PF, Crane CH, Wu TT, Lunagomez S, Lynch PM, et
al. Paclitaxel-based chemoradiotherapy in localized gastric carcinoma:
degree of pathologic response and not clinical parameters dictated
patient outcome. J Clin Oncol 2005;23:1237-44.[LinkOut]
- Ajani JA, Winter K, Okawara GS, Donohue JH, Pisters PW, Crane
CH, et al. Phase II trial of preoperative chemoradiation in patients
with localized gastric adenocarcinoma (RTOG 9904): quality of
combined modality therapy and pathologic response. J Clin Oncol
2006;24:3953-8.[LinkOut]
- Kelsey CR, Chino JP, Willett CG, Clough RW, Hurwitz HI, Morse
MA, et al. Paclitaxel-based chemoradiotherapy in the treatment of
patients with operable esophageal cancer. Int J Radiat Oncol Biol Phys
2007;69:770-6.[LinkOut]
- Schwartz GK, Winter K, Minsky BD, Crane C, Thomson PJ, Anne P, et
al. Randomized phase II trial evaluating two paclitaxel and cisplatincontaining
chemoradiation regimens as adjuvant therapy in resected
gastric cancer (RTOG-0114). J Clin Oncol 2009;27:1956-62.[LinkOut]
- Choong NW, Mauer AM, Haraf DC, Ferguson MK, Sandler AB, Kesler
KA, et al. Long-term outcome of a phase II study of docetaxel-based
multimodality chemoradiotherapy for locally advanced carcinoma of
the esophagus or gastroesophageal junction. Med Oncol 2010;Aug
21.[Epub ahead of print][LinkOut]
- Spigel DR, Greco FA, Meluch AA, Lane CM, Farley C, Gray JR, et al.
Phase I/II trial of preoperative oxaliplatin, docetaxel, and capecitabine
with concurrent radiation therapy in localized carcinoma of the
esophagus or gastroesophageal junction. J Clin Oncol 2010;28:2213-9.[LinkOut]
- Kambysellis MP, Ho KF, Craddock EM, Piano F, Parisi M, Cohen J.
Pattern of ecological shifts in the diversification of Hawaiian Drosophila
inferred from a molecular phylogeny. Curr Biol 1995;5:1129-39.[LinkOut]
- Ajani JA, Correa AM, Walsh GL, Komaki R, Lee JH, Vaporciyan AA,
et al. Trimodality therapy without a platinum compound for localized
carcinoma of the esophagus and gastroesophageal junction. Cancer
2010;116:1656-63.[LinkOut]
- Ajani JA, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni
C, et al. Quality of life with docetaxel plus cisplatin and f luorouracil
compared with cisplatin and fluorouracil from a phase III trial for
advanced gastric or gastroesophageal adenocarcinoma: the V-325 Study
Group. J Clin Oncol 2007;25:3210-6.[LinkOut]
- Ajani JA, Moiseyenko VM, Tjulandin S, Majlis A, Constenla M, Boni
C, et al. Clinical benefit with docetaxel plus fluorouracil and cisplatin
compared with cisplatin and fluorouracil in a phase III trial of advanced
gastric or gastroesophageal cancer adenocarcinoma: the V-325 Study
Group. J Clin Oncol 2007;25:3205-9.[LinkOut]
- Shah M, Shibata S, Stoller RG, Kemeny M, Ritch PS, Krishnamurthi
SS, et al. Random assignment multicenter phase II study of modified
docetaxel, cisplatin, fluorouracil (mDCF) versus DCF with growth
factor support (GCSF) in metastatic gastroesophageal adenocarcinoma
(GE) [abstract]. J Clin Oncol 2010;s28:4014.
- Ajani JA, Rodriguez W, Bodoky G, Moiseyenko V, Lichinitser M,
Gorbunova V, et al. Multicenter phase III comparison of cisplatin/
S-1 with cisplatin/infusional fluorouracil in advanced gastric or
gastroesophageal adenocarcinoma study: the FLAGS trial. J Clin Oncol
2010;28:1547-53.[LinkOut]
- Park SH, Lee WK, Chung M, Lee Y, Han SH, Bang SM, et al. Paclitaxel
versus docetaxel for advanced gastric cancer: a randomized phase II
trial in combination with infusional 5-fluorouracil. Anticancer Drugs
2006;17:225-9.[LinkOut]
- Im CK, Jung SE, Rha SY, Ahn J, Shin S, Noh S, et al. Comparison
of taxane-based (docetaxel or paclitaxel) regimens combined with
5-fluorouracil continuous infusion and low dose leucovorin for
advanced gastric carcinoma: Analysis of two phase II trials [abstract]. J
Clin Oncol 2008;s26:15679.
- Webb A, Cunningham D, Scarffe JH, Harper P, Norman A, Joffe JK, et
al. Randomized trial comparing epirubicin, cisplatin, and fluorouracil
versus f luorouracil, doxorubicin, and methotrexate in advanced
esophagogastric cancer. J Clin Oncol 1997;15:261-7.[LinkOut]
- Roth AD, Fazio N, Stupp R, Falk S, Bernhard J, Saletti P, et al.
Docetaxel, cisplatin, and f luorouracil; docetaxel and cisplatin; and
epirubicin, cisplatin, and f luorouracil as systemic treatment for
advanced gastric carcinoma: a randomized phase II trial of the Swiss
Group for Clinical Cancer Research. J Clin Oncol 2007;25:3217-23.[LinkOut]
- Tebbutt NC, Cummins MM, Sourjina T, Strickland A, Van Hazel G, Ganju V, et al. Randomised, non-comparative phase II study of
weekly docetaxel with cisplatin and 5-fluorouracil or with capecitabine
in oesophagogastric cancer: the AGITG ATTAX trial. Br J Cancer
2010;102:475-81.[LinkOut]
- Thuss-Patience PC, Kretzschmar A, Repp M, Kingreen D, Hennesser
D, Micheel S, et al. Docetaxel and continuous-infusion fluorouracil
versus epirubicin, cisplatin, and f luorouracil for advanced gastric
adenoc a rc inoma: a randomi zed pha se I I study. J Cl in Oncol
2005;23:494-501.[LinkOut]
- Sym SJ, Park S, Kwon KY, Jung I, Park J, Cho E, et al. A randomized
phase II trial of weekly docetaxel plus either cisplatin or oxaliplatin in
patients with previously untreated advanced gastric cancer: Preliminary
results [abstract]. J Clin Oncol 2009;Abstr 92.
- Lind PA, Gubanski M, Johnson AE, Fernebro E, Flygare P, Karlberg
I, et al. Final results of the randomized phase II study of sequential
docetaxel and irinotecan with infusion 5-fluorouracil/folinic acid in
patients with advanced gastric cancer - GA-TAC [abstract]. J Clin Oncol
2008;s26:4579.
- Ridwelski K, Fahlke J, Kettner E, Schmidt C, Keilholz U, Quietzsch
D, et al. Docetaxel-cisplatin (DC) versus 5-f luorouracil-leucovorincisplatin
(FLC) as first-line treatment for locally advanced or metastatic
gastric cancer: Preliminary results of a phase III study [abstract]. J Clin
Oncol 2008;s26:4512.
Cite this article as: Jimenez P, Pathak A, Phan A. The role of taxanes in the management of gastroesphageal
cancer. J Gastrointest Oncol. 2011;2(4):240-249. DOI:10.3978/j.issn.2078-6891.2011.027
|