
Intensive care for patients with gastric cancers: outcome and survival prognostic factors
Introduction
Therapeutic management of patients with hematological and solid malignancies in intensive care unit (ICU) is a controversial topic both in terms of potential futility for individual patients and in terms of use of resources. Recent therapeutic breakthroughs have drastically improved the life expectancy and the quality of life of patients with a number of different solid tumors. On the other hand, remission remains a marginal phenomenon for patients suffering from metastatic tumors, especially gastro-intestinal cancers. A number of studies have examined the effect of hematological and solid malignancies on patients who are hospitalized in ICU (1,2) and some have focused on the particular issue of patients who have undergone bone marrow transplant (3,4) However, there is only a handful of studies that have analyzed the management and prognosis of patients hospitalized in ICU depending on the specific nature of their solid tumor. They have generally examined lung cancer (5,6), but other cancer types have seldom been investigated.
The different forms of gastric cancers have similar natural histories and therapeutic management strategies and they all share low survival rates. Close to one million new cases were diagnosed in the world in 2012 and 723,100 related deaths were recorded that year (7). The therapeutic management of these cancers has changed since 2016, with the introduction of the FLOT neoadjuvant chemotherapy protocol (docetaxel, oxaliplatin, fluorouracil, and leucovorin) for patients with resectable cancers (8). Under this protocol, median overall survival reached 22.9 months for patients who underwent both surgery and chemotherapy (9). In addition, the use of targeted therapies, such as trastuzumab, in HER2-positive advanced gastric cancers has proved to be beneficial in terms of survival (10).
In some cases, patients with gastric cancers require life support in ICUs in the course of their illness. We have tried to determine the mortality prognostic factors and the outcome of these patients in a single center retrospective study that includes the patients hospitalized in our medical ICU over the last 10 years.
Methods
Patients
We performed a retrospective analysis of a single center cohort in a university hospital medical ICU. We screened the digital medical charts of all the patients who were admitted in the ICU between January 2007 and July 2017 by searching for the following keywords “gastric cancer”, “gastroesophageal junction cancer”.
We excluded patients younger than 18 years old, patients who did not have any organ failure and patients who were hospitalized in ICU for immediate postoperative care after gastrectomy. The patients, who did not have a histological confirmation of their cancer and for whom some of the key data were missing, were excluded.
Only the first stay was analyzed for patients who were admitted more than once in ICU.
Data collection
Data was extracted from digital medical records.
Statistical analysis
Continuous variables are presented as mean ± standard deviation (SD) and were compared using Mann & Whitney test. Qualitative variables are presented as numbers and percentages and were compared using χ2 test or Fisher’s exact test depending on theoretical effectives. To assess prognostic factors of death all potential factors presenting P value <0.1 in univariate analysis were included in a multivariate regression model. A logistic regression model using Firth’s bias reduction method was fitted to handle separation in our data. Stepwise selection procedure based on AIC (Akaike Information Criterion) was then performed. Results are presented as odds ratio (OR) with their 95% confidence intervals (CIs). Survival curves were performed using Kaplan-Meier method and compared with log-rank test. A P value <0.05 was considered as statistically significant. All the analyses were conducted using R software version 3.2.2. R Core Team (2015). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/.
The study design was approved by the Institutional Review Board of the Strasbourg Medical School (ref. AMK/BG/ 2015/2015-34).
Results
Patients’ characteristics and management
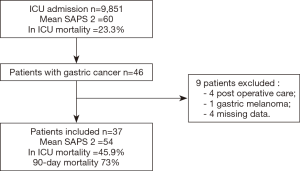
Forty-six patients with gastric cancer were admitted between January 2007 and July 2017 (incidence of 4.6‰). Nine patients were excluded: 4 were admitted for immediate postoperative care, 1 patient had a gastro-oesophageal junction melanoma and 4 patients were excluded because of missing data. Final analysis was done on a total of 37 patients (Figure 1).
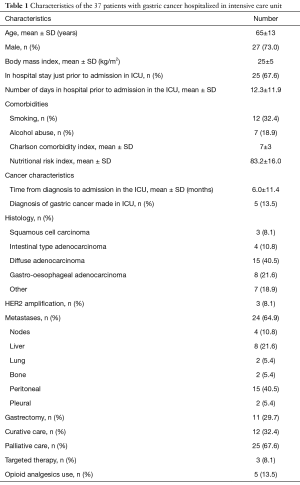
The majority of patients were males (73%) and the mean age was 65 years old (Table 1). Twenty-five patients (67.6%) were hospitalized before their admission in the ICU and 12 patients were directly admitted in ICU from their home. Twenty-four patients (64.9%) had metastatic cancer and 13 patients (35.1%) had a localized cancer with all but one of them in curative care. The mean time between the diagnosis of gastric cancer and admission in the ICU was 6.0±11.4 months. The most frequent histological type was diffuse adenocarcinoma (15 patients, 40.5%), followed by gastro-oesophageal junction adenocarcinoma (8 patients, 21.6%), intestinal type adenocarcinoma (4 patients, 10.8%) and squamous cell carcinoma (3 patients, 8.1%).
Full table
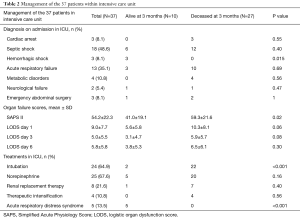
Table 2 shows the characteristics of the patients and the treatment they underwent on admission. The most frequent diagnosis on admission was septic shock (18 patients, 48.6%), followed by acute respiratory failure (13 patients, 35.1%). The mean simplified acute physiology score (SAPS II) was 54.2±22.3 and the mean logistic organ dysfunction score (LODS) on admission was 9.0±7.7.
Full table
A majority of the patients were intubated at some point during their ICU stay (24 patients, 64.9%) and were treated with norepinephrine (25 patients, 67.6%). Therapeutic intensification was defined as the necessity of adding at least one organ support 3 days or more after admission. Four patients (10.8%) required such intensification.
Outcome and mortality prognostic factors
Twenty-four patients (64.9%) died in our hospital without being discharged, among which 17 (45.9%) died within the ICU. Only 10 patients (27.0%) survived longer than 3 months after ICU admission, among which 2 were still hospitalized at that time point.
In total, 34 patients (92%) died over the study period with a median survival of 16.5 (4.8–121) days. Among the 3 patients who were still alive at the end of the study period, one is considered in remission (with a survival >5 years) and the two others were still alive after 2 years and 6 months respectively. Thirteen patients (35.1%) were discharged from the hospital. Their 3-month outcome after discharge was as follows: 3 were dead, 2 had a World Health Organization (WHO) performance status <2 grade, 4 had a WHO performance status ≥2 and 4 patients could not be evaluated.
Risk factors of ICU mortality
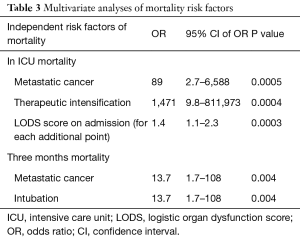
Three independent risk factors of ICU mortality were identified in multivariate analysis (Table 3): metastatic cancer (OR =89; 95% CI, 2.7–6,588), therapeutic intensification (OR =1,471; 95% CI, 9.8–811,973) and LODS score on admission (OR =1.4; 95% CI, 1.1–2.3).
Full table
In addition, several risk factors were identified in univariate analysis: SAPS II score on admission (P=0.01), intubation (P<0.01), use of norepinephrine (P=0.01), LODS score on day 3 (P<0.01) and day 6 (P<0.01) and worsening of LODS score between admission and day 6 (P<0.01).
Risk factors of 3-month mortality
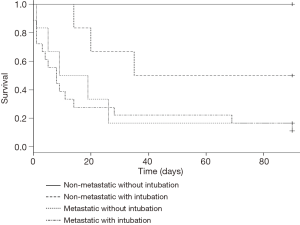
Two independent risk factors of 3-month mortality were identified in multivariate analysis: metastatic cancer (OR =13.70; 95% CI, 1.7–108) and intubation (OR =13.70; 95% CI, 1.7–108).
Subgroup analysis
Cancers diagnosed within the ICU
Five patients (13.5%) were diagnosed with gastric cancer while hospitalized in the ICU. Four of them had metastatic cancer. Three of them died in the ICU and the two others without being discharged from the hospital.
Localized versus metastatic cancer
Among the 13 patients with localized cancer, 12 were undergoing curative care (2 had undergone neoadjuvant chemotherapy, 3 had undergone surgery, 3 had undergone both treatments and 4 patients had been diagnosed recently and had therefore not undergone any specific treatment yet) and one was undergoing palliative care because of his general status. Nine patients were discharged from the hospital with a median survival of 8 months. Two patients were readmitted to the ICU and one patient survived more than 5 years.
Among the 25 patients who were under palliative care, 11 had already undergone chemotherapy, 3 were already treated with a combination of chemotherapy and trastuzumab, and the others had been too recently diagnosed. Fifteen patients died in the ICU and 6 patients died in the hospital without being discharged. Four patients were discharged from the hospital with a median survival of 4.5 months. Finally, only 2 patients with metastatic cancers were alive 3 months after their admission in the ICU (Figure 2).
Intubation
Twenty-four patients (64.9%) were intubated in the ICU and only 2 of them were alive 3 months after admission. One of the patients who survived had a HER-2 positive metastatic cancer but was intubated for less than a day in a context of iatrogenic opioid overdose. He survived for 7 months after ICU admission (Figure 2). The other patient who was intubated in the ICU and who survived more than 3 months had a non-metastatic cancer that was surgically removed. He was hospitalized in the ICU with acute respiratory distress syndrome and was ventilated mechanically for 24 days. He survived for 5 months after his ICU admission.
Therapeutic intensification
Four of the 37 patients (10.1%) in our study underwent therapeutic intensification as defined above: all died within the ICU.
Discussion
This is the first study to focus on the outcome of patients with gastric cancers who are admitted to an ICU for acute life-threatening organ failure in the course of their illness. The only study that discusses the management of patients with gastric cancers who are hospitalized in ICU is a retrospective Chinese cohort that reports on the predictive factors of ICU lengths of stay for patients 60 years and older (11). Nutritional support and shock were identified as prognostic factors correlating with length of stay. Most of their patients were admitted in ICU for postoperative care and were selected on the basis of their age. By contrast, our study excluded the patients who were hospitalized for immediate postoperative care in order to examine more closely the patients who were proposed to the ICU for acute life-threatening medical reasons. In addition, our study is the only report investigating the outcome of these patients in a European context.
We calculated the LODS for all the patients on admission, on day 3 and 6. This score was initially published in 1996 to evaluate the severity of patients hospitalized in ICU (12). In a study focusing on the controversial issue of patients with hematological and solid malignancies who require mechanical ventilation, Lecuyer et al. subsequently showed that the LODS score on day 3 and 6, as well as therapeutic intensification (initiation of mechanical ventilation, vasopressors, or dialysis) after day 3 were significantly associated with mortality (13). Our data confirm the predictive power of the LODS score in the context of gastric cancers: the LODS scores on admission, day 3 and 6 are all significantly associated with ICU mortality in univariate analysis. In addition, the LODS score on admission and therapeutic intensification are independently associated with ICU mortality in multivariate analysis (all of the patients for whom mechanical ventilation, vasopressors, or dialysis were initiated after day 3 died in the ICU).
The in-hospital mortality of our cohort was 65.8% compared to the mortality of 78.2% reported by Lecuyer et al. (13). This difference can be a statistical artifact or reflect a difference in the cohorts studied. Indeed, Lecuyer included patients with a wide variety of solid tumors and 60% of patients with hematological malignancies in his study. In addition, all of the patients in his study underwent mechanical ventilation. Our study population focused exclusively on one type of cancer. Finally, the proportion of metastatic cancers, which is not reported in Lecuyer’s work, probably plays a determining role in overall survival rates in our results.
Mechanical ventilation for acute respiratory failure has been identified as a mortality prognostic factor for patients with hematological or solid malignancies (14). In our cohort, intubation is not associated with mortality in ICU but it is associated with 3-month mortality in multivariate analysis. This crucial finding points to the potential futility of such invasive management in terms of medium or long-term survival, especially for patients with metastatic cancers.
The median survival rate of patients receiving curative care with neoadjuvant FLOT chemotherapy is reported to be 22.9 months (15). Given these results, it seems reasonable to admit patients in ICU if they require life support therapy in the course of their illness. In our cohort, 12 patients were under curative care when they were admitted in the ICU. Two patients died in ICU and one additional patient died in the hospital. Nine patients were discharged from the hospital with a median survival of 8 months. None of these patients were treated with the FLOT chemotherapy protocol but these results should not discourage clinicians from admitting these patients into ICU on the sole basis of their gastric cancer.
By contrast, the median survival of patients with metastatic gastric cancers who receive palliative FLOT chemotherapy is between 11 and 14.6 months (16) and even shorter when less effective protocols are used (17,18). Quality of life is an important issue for these patients who cannot be offered curative care. This element should be central when deciding to admit this subgroup of patients in ICU or not. The majority of the patients in our cohort had metastatic cancers (24 patients, 64.9%). The median time between the diagnosis of cancer and the admission in ICU was 2.9 months for this subgroup of patients. The oncological treatment had therefore barely begun for a large proportion of these patients and decisions regarding potential admission in ICU as well as the use of life-sustaining therapies had probably not been taken yet, which certainly explains why a number of these patients were admitted in ICU.
Among the subgroup of patients with metastatic cancer, 14 patients (41.7%) died in the ICU and 20 patients (83.3%) died in our hospital without having been discharged. The 4 patients who were discharged had a median survival of 4.5 months. These data highlight the fact that admitting patients with metastatic gastric cancers does not increase their survival substantially while potentially altering their quality of life through the use of ICU invasive treatments. These results should be kept in mind when discussing the appropriateness of life-sustaining therapies with patients and their families.
The main limitation of this study resides in its retrospective nature and the fact that it is a single center study.
Conclusions
The admission of gastric cancer patients to the ICU for life-threatening organ failure remains a matter of debate in a context of lack of evidence-based recommendations. Our study identifies a number of factors that are most associated with 3-month and ICU mortality: mechanical ventilation support, presence of metastasis, a high LODS score on admission and therapeutic intensification during the ICU stay. These elements could help guide clinicians in their use of ICU resources and their discussions of prognosis with patients and families.
Acknowledgements
Maleka Schenck, Marie Line Harlay, Jean Etienne Herbrecht, Max Guillot and Vincent Castelain who take care of these patients every day with great dedication and professionalism.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study design was approved by the Institutional Review Board of the Strasbourg Medical School (ref AMK/BG/ 2015/2015-34). Consent to publish from all patients treated in the department were obtained for all observational studies.
References
- Ha FJ, Weickhardt AJ, Parakh S, et al. Survival and functional outcomes of patients with metastatic solid organ cancer admitted to the intensive care unit of a tertiary centre. Crit Care Resusc 2017;19:159-66. [PubMed]
- Schellongowski P, Sperr WR, Wohlfarth P, et al. Critically ill patients with cancer: chances and limitations of intensive care medicine-a narrative review. ESMO Open 2016;1:e000018. [Crossref] [PubMed]
- Afessa B, Tefferi A, Hoagland HC, et al. Outcome of recipients of bone marrow transplants who require intensive-care unit support. Mayo Clin Proc 1992;67:117-22. [Crossref] [PubMed]
- Price KJ, Thall PF, Kish SK, et al. Prognostic indicators for blood and marrow transplant patients admitted to an intensive care unit. Am J Respir Crit Care Med 1998;158:876-84. [Crossref] [PubMed]
- Reichner CA, Thompson JA, O’Brien S, et al. Outcome and code status of lung cancer patients admitted to the medical ICU. Chest 2006;130:719-23. [Crossref] [PubMed]
- Soares M, Darmon M, Salluh JIF, et al. Prognosis of lung cancer patients with life-threatening complications. Chest 2007;131:840-6. [Crossref] [PubMed]
- Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87-108. [Crossref] [PubMed]
- Al-Batran SE, Hofheinz RD, Pauligk C, et al. Histopathological regression after neoadjuvant docetaxel, oxaliplatin, fluorouracil, and leucovorin versus epirubicin, cisplatin, and fluorouracil or capecitabine in patients with resectable gastric or gastro-oesophageal junction adenocarcinoma (FLOT4-AIO): results from the phase 2 part of a multicentre, open-label, randomised phase 2/3 trial. Lancet Oncol 2016;17:1697-708. [Crossref] [PubMed]
- Das M. Neoadjuvant chemotherapy: survival benefit in gastric cancer. Lancet Oncol 2017;18:e307. [Crossref] [PubMed]
- Bang YJ, Van Cutsem E, Feyereislova A, et al. Trastuzumab in combination with chemotherapy versus chemotherapy alone for treatment of HER2-positive advanced gastric or gastro-oesophageal junction cancer (ToGA): a phase 3, open-label, randomised controlled trial. Lancet 2010;376:687-97. [Crossref] [PubMed]
- Zhang XC, Zhang ZD, Huang DS. Prediction of length of ICU stay using data-mining techniques: an example of old critically Ill postoperative gastric cancer patients. Asian Pac J Cancer Prev 2012;13:97-101. [Crossref] [PubMed]
- Le Gall JR, Klar J, Lemeshow S, et al. The Logistic Organ Dysfunction system. A new way to assess organ dysfunction in the intensive care unit. ICU Scoring Group. JAMA 1996;276:802-10. [Crossref] [PubMed]
- Lecuyer L, Chevret S, Thiery G, et al. The ICU trial: a new admission policy for cancer patients requiring mechanical ventilation. Crit Care Med 2007;35:808-14. [Crossref] [PubMed]
- Taccone FS, Artigas AA, Sprung CL, et al. Characteristics and outcomes of cancer patients in European ICUs. Crit Care 2009;13:R15. [Crossref] [PubMed]
- Al-Batran SE, Hartmann JT, Hofheinz R, et al. Biweekly fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) for patients with metastatic adenocarcinoma of the stomach or esophagogastric junction: a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie. Ann Oncol 2008;19:1882-7. [Crossref] [PubMed]
- Van Cutsem E, Boni C, Tabernero J, et al. Docetaxel plus oxaliplatin with or without fluorouracil or capecitabine in metastatic or locally recurrent gastric cancer: a randomized phase II study. Ann Oncol 2015;26:149-56. [Crossref] [PubMed]
- Okines AF, Norman AR, McCloud P, et al. Meta-analysis of the REAL-2 and ML17032 trials: evaluating capecitabine-based combination chemotherapy and infused 5-fluorouracil-based combination chemotherapy for the treatment of advanced oesophago-gastric cancer. Ann Oncol 2009;20:1529-34. [Crossref] [PubMed]
- Starling N, Rao S, Cunningham D, et al. Thromboembolism in patients with advanced gastroesophageal cancer treated with anthracycline, platinum, and fluoropyrimidine combination chemotherapy: a report from the UK National Cancer Research Institute Upper Gastrointestinal Clinical Studies Group. J Clin Oncol 2009;27:3786-93. [Crossref] [PubMed]


