
Correlation between endoscopic features of the anastomosis after low anterior resection and postsurgical anorectal function
Introduction
Rectal cancer of the mid- and even lower rectum is treated by low anterior resection (LAR), which involves removal of the entire tumor and reconstruction of the bowel. This procedure is not without risk of such complications as anastomotic leakage and impaired anorectal function. While the oncologic outcomes of LAR have improved over the last two decades, anastomotic leakage, the most feared complication, remains common, with an incidence of 2.5–23% (1). A total of 60–80% of patients experience anorectal dysfunction associated with LAR. Such dysfunction takes on various manifestations, including fecal incontinence, increased defecation frequency, and urgency (2). Outcome in terms of anorectal function after LAR is difficult to predict because the postoperative anorectal function is dependent on the height of the anastomosis (3), neorectal capacity and compliance, and whether damage to a pelvic muscle or to an autonomic nerve in the pelvis occurs (4), which means that the surgical quality is important to the maintenance of anorectal function after LAR.
Diverting ileostomy has been shown to effectively reduce the post-LAR incidences of symptomatic anastomotic leakage and procedure-related death (4), and almost all patients who have undergone LAR at either of our institutions have received a diverting stoma. However, the optimal timing for ileostomy closure is undetermined; there are no definitive guidelines, and there are also no standard recommendations for examination before ileostomy closure. Some surgeons perform double-contrast barium enema and others perform endoscopy to confirm patency of the anastomosis before ileostomy closure. However, neither endoscopic data concerning the findings nor implications of the findings have been reported.
Further, evaluating the quality of LAR is difficult. Because the anastomosis is one of the fundamental components of the procedure, we hypothesized that the endoscopic features of the anastomosis reflect the surgical quality and are thus predictive of post-LAR anorectal function.
In this retrospective study, we aimed to document characteristics of the anastomoses created at the time of LAR and then viewed endoscopically before ileostomy closure. In addition, we established systems by which we scored the endoscopic findings, and we then evaluated the relation between the scores and anorectal function after ileostomy closure.
Methods
Study patients
Included in the study were 80 patients [56 men, 24 women; median age: 63.5 (range, 26–82) years] who underwent LAR with a diverting stoma as primary surgery for rectal cancer. All surgeries were performed at Kanagawa Cancer Center between September 2014 and August 2017, and endoscopic examination of the anastomosis had been performed in all 80 patients before ileostomy closure. In addition, all patients were interviewed about their anorectal function after the closure. All patients provided written, informed consent for the use of their clinical information for study purposes. Our study was cleared with the institution review board of Kanagawa Cancer Center (IRB number: EKI-124).
Post-LAR endoscopic examination
Endoscopic examination was performed in all patients about 6 months after the primary operation, just before closure of the ileostomy. Because patients had a covering ileostomy, intestinal tract cleansing was not performed. A standard video endoscope (CF-260 series or CF-290 series; Olympus Medical Systems Co., Tokyo, Japan) was used to obtain images of the anastomosis. The mucosal surface was rinsed with saline under endoscopic vision, and the examination was then performed, consisting mainly of the identification of any of seven features near the anastomosis: erythema, erosion, ulceration, granulomatous change, fine granular protrusions, or white-coated or hemorrhagic mucosa (Figure 1). We applied two simple endoscopic scoring systems that we developed for evaluation. The first was a system by which we scored the presence or absence of the seven features at the anastomosis as viewed with a colonoscope, with absence scored as 0 and presence scored as 1 for a possible total “Endoscopic Score” of 0 to 7. This system was based on the Simple Endoscopic Score for Crohn’s Disease and similar to that reported in a case of ileal pouchitis that developed after surgical treatment of ulcerative colitis (5). The score was determined in each case by two well-trained endoscopists who had reviewed a series of representative endoscopic images before evaluation. The second was a system by which we scored the width of the anastomosis. The width was determined on the basis of the diameter of the colonoscope, and in cases in which the colonoscope could not be passed through the anastomosis, the width was recorded as ≤12 mm. Width of the anastomosis ≥16, 13–15, 10–12, 7–9, 4–6, or ≤3 mm. was scored as 0, 1, 2, 3, 4, or 5, respectively.

Assessment of anorectal function after ileostomy closure
Two months after the ileostomy closure, patients anorectal function was assessed. For this, patients were interviewed about daily defecation frequency, incontinence, and any need for oral medication to induce defecation.
Incontinence was assessed of the basis of the Kirwan classification system (6). We assigned what we refer to as a Kirwan Score as follows: 1 for perfect continence, 2 for flatus incontinence, 3 for occasional minor soiling, 4 for frequent major soiling, and 5 if colostomy is required.
Statistical analysis
The Endoscopic Score and Anastomosis Size Score were recorded for each patient individually, as was the Kirwan Score. We summed these scores and then took the mean or median (range) values, which were calculated for the total patient group. Measured values were subjected to the Kruskal-Wallis test, and a P value of <0.05 was considered statistically significant. Correlation between endoscopic features of the anastomoses and anorectal function, i.e., between Endoscopic Scores, Anastomosis Size Scores, or Endoscopic plus Anastomosis Size Scores and Kirwan Scores was analyzed by Spearman’s rank correlation test for nonparametric data, and statistical significance of the correlation coefficient (r) was accepted at P<0.05.
Results
Patient characteristics
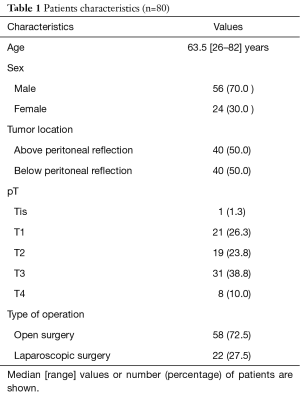
Clinical characteristics of the 80 patients who made up the study group are shown in Table 1. The tumor was above the peritoneal reflection in half of the patients, and T3 or T4 depth of invasion was found in nearly 50%. LAR was performed by means of open surgery in 58 patients (72.5%). Median time from LAR to ileostomy closure was 8 months (range, 2–13 months).
Full table
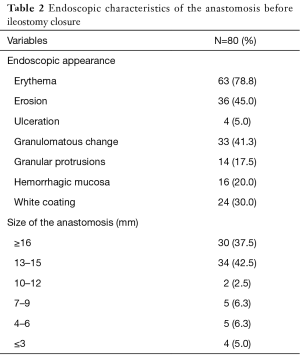
Endoscopic appearance and data collection
Features of the anastomoses visualized before ileostomy closure are summarized in Table 2. Erythema was seen in more than three fourths of the patients (78.8%); erosion was seen in 45.0%, but ulceration was seen in only four patients. The mean Endoscopic Score before ileostomy closure was 2.38 (range, 0–6). The anastomosis was sufficiently large to admit the endoscope in 80% of patients (Table 2). The mean Anastomosis Size Score was 1.16 (range, 0–5). The mean sum of the Endoscopic Score and Anastomosis Size Score before ileostomy closure was 3.43 (range, 0–8).
Full table
Anorectal function after ileostomy closure
Mean daily defecation frequency after ileostomy closure was 4.5 (range, 1–20) per day, but about 50% of patients required either a laxative (25.0%), some occasionally and some regularly, or an antidiarrheal agent (26.0%). The mean Kirwan Score was 1.54 (range, 1–4).
Relationship between endoscopic findings and post-LAR function
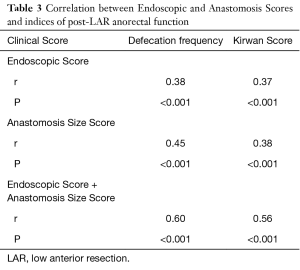
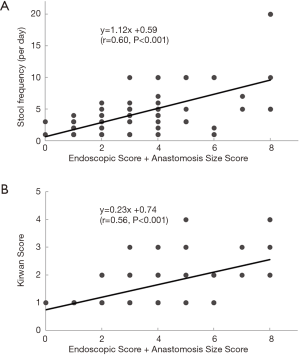
Correlation between endoscopic appearances of the anastomosis before ileostomy closure (i.e., Endoscopic Scores and Anastomosis Size Scores) and indices of anorectal function after ileostomy closure (i.e., defecation frequency and Kirwan Scores) is shown in Table 3. Positive, moderate correlation was found between the Endoscopic findings before ileostomy closure and postoperative anorectal function. The sum of the pre-closure scores (Endoscopic Score + Anastomosis Size Score) correlated more closely with defecation frequency (r=0.60, P<0.001) than did either of these two scores alone (Figure 2A). The sum of the pre-closure scores (Endoscopic Score + Anastomosis Size Score) also correlated more closely with the Kirwan Score (r=0.56, P<0.001) than did either of these two scores alone (Figure 2A,B).
Full table
Discussion
Endoscopy remains the gold standard for assessing gastroenteric lesions. To date, clinically important endoscopic features of ulcerative colitis, Crohn’s Disease, and ileal pouchitis have been reported, and the incidence of these features has also been reported (5,7,8). Although the anastomosis is checked endoscopically before covering ileostomy closure at some institutions, results of such examination have not been reported. Because our study involved a fairly large group of patients, we were able to record in detail the various features that can characterize the anastomosis after LAR but before ileostomy closure, and we were able also to document the frequency at which these features occur. Further, we were able to analyze whether a relation exists between endoscopic features of the anastomosis before closure of the ileostomy and anorectal function after the closure.
We found that the endoscopic appearance of the anastomosis was generally related to post-closure anorectal function. A commonly accepted notion is that anorectal function after LAR depends strongly on the height of the anastomosis (3). We examined our study data in light of the heights of the anastomoses and found a trend toward better function when the anastomosis was above the peritoneal reflection. Association between the location of the anastomosis and defecation frequency and that between the location of the anastomosis and the Kirwan score were not significant (P=0.18 and P=0.08 respectively).
The surgical quality of the newly constructed anastomosis is also thought to influence post-LAR anorectal function, such that even if the rectal cancer is located above the peritoneal reflection, a poor-quality anastomosis, resulting in leakage, example, can result in inadequate anorectal function (1). However, it is quite difficult to score surgical quality, and there are no reports describing such scoring. We asked ourselves whether the endoscopic features of the anastomosis reflect the quality of the LAR and whether these features can be used to predict a patient’s anorectal function after ileostomy closure. We found that both our Endoscopic Score, based on the endoscopic appearance of the anastomosis, and our Anastomosis Size Score correlated positively with defecation frequency after ileostomy closure (r=0.38 and r=0.45, respectively), and we found that the sum of the two scores correlated moderately with defecation frequency (r=0.60) and with the Kirwan Scores, indicating that our scoring systems, used together, are useful for prediction of postoperative function.
Endoscopy is extremely valuable for evaluating the anastomosis in patients who have undergone LAR. However, valid endoscopic scoring systems that are easily applied in clinical settings are needed to standardize and facilitate meaningful comparisons. Our scoring system is quite simple; scores are calculated on the basis of the presence or absence of seven specific endoscopically determined features and the diameter of anastomosis, and the information provided by the scores is easily communicated to patients.
When we assess the endoscopic appearance of the anastomosis, we must consider the possible influence of saline irrigation and mucus accumulation in the bowel. These factors can result in redness and even bleeding, but they would not be related to ulceration, granulation, or the size of the anastomosis.
Our study was limited by its retrospective approach, it did not include a comparison between patients’ pre-LAR and post-LAR anorectal function, and long-term outcomes were not investigated. Although the correlation coefficients were significant, the correlations we found were moderate at best. This means that the systems we used to score the endoscopic features of the anastomoses prior to ileostomy closure need further refinement.
Our study results suggest that endoscopic examination of the anastomosis should be performed routinely before ileostomy closure. The findings may facilitate prediction of post-LAR anorectal function and provide physicians the opportunity to explain to patients in detail what to expect after ileostomy closure. Furthermore, endoscopic findings might also reflect surgical quality, an important clinical variable that has not been easily evaluated thus far. Results of our study are encouraging, and we anticipate further studies to confirm our findings.
Acknowledgements
The study was supported by departmental resources.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Our study was cleared with the institution review board of Kanagawa Cancer Center (IRB number: EKI-124). All patients provided written informed consent for the use of their clinical information for study purposes.
References
- Hain E, Manceau G, Maggiori L, et al. Bowel dysfunction after anastomotic leakage in laparoscopic sphincter-saving operative intervention for rectal cancer: A case-matched study in 46 patients using the Low Anterior Resection Score. Surgery 2017;161:1028-39. [Crossref] [PubMed]
- Bryant CL, Lunniss PJ, Knowles CH, et al. Anterior resection syndrome. Lancet Oncol 2012;13:e403-8. [Crossref] [PubMed]
- Rasmussen OO, Petersen IK, Christiansen J. Anorectal function following low anterior resection. Colorectal Dis 2003;5:258-61. [Crossref] [PubMed]
- Lindgren R, Hallböök O, Rutegård J, et al. Does a defunctioning stoma affect anorectal function after low rectal resection? Results of a randomized multicenter trial. Dis Colon Rectum 2011;54:747-52. [Crossref] [PubMed]
- Shinozaki M, Koganei K, Fukushima T. Relationship between endoscopic findings of the pouch and bowel frequency after restorative proctocolectomy in ulcerative colitis. Dig Endosc 2005;17:224-9. [Crossref]
- Kirwan WO, Turnbull RB Jr, Fazio VW, et al. Pullthrough operation with delayed anastomosis for rectal cancer. Br J Surg 1978;65:695-8. [Crossref] [PubMed]
- Paine ER. Colonoscopic evaluation in ulcerative colitis. Gastroenterol Rep (Oxf) 2014;2:161-8. [Crossref] [PubMed]
- Rosa B, Pinho R, de Ferro SM, et al. Endoscopic scores for evaluation of Crohn's disease activity at small bowel capsule endoscopy: general principles and current applications. GE Port J Gastroenterol 2015;23:36-41. [Crossref] [PubMed]


