
Population-based assessment of the performance of sigmoidoscopy in the detection of colorectal cancer: implications for future screening recommendations
Introduction
Colorectal cancer (CRC) is one of the most common incident cancers as well as one of the most common causes of cancer deaths worldwide (1). Current North American guidelines advocate for the use of flexible sigmoidoscopy every 10 years as an alternative screening strategy for the detection of CRC among average-risk individuals (2). However, other international guidelines (e.g., Australian) recommend against its routine use in CRC screening (3). The current study aims at evaluating its performance in a hypothetical population-based model based on the Surveillance, Epidemiology and End Results (SEER)-18 registry database (4).
Methods
We explored SEER database through SEER*stat software. Cases diagnosed as colorectal carcinoma within the age group of 50–74 years during the year 2010 were included. Cases were classified as either accessible or non-accessible to detection by screening sigmoidoscopy by virtue of their anatomic location (tumors within the rectum, sigmoid or descending colon were considered accessible, while cases within other colorectal sub-sites were considered non-accessible). Overall, US citizens within the age group of 50–74 years covered by the SEER-18 registry were determined from SEER rate session. Assuming that all eligible US citizens underwent screening sigmoidoscopy and assuming that all CRC cases within accessible sites were correctly identified by sigmoidoscopy, true positive, true negative, and false negative rates were calculated. False positive cases could not be derived due to data limitations. Sensitivity and negative predictive value (NPV) of screening sigmoidoscopy were also computed.
Results
A total of 18,794 patients aged between 50–74 years old were diagnosed during 2010 (total US population covered by the SEER-18 registry in the same year and within the same age group included 21,613,411 US citizens). A total of 10,786 CRC patients (57.4%) were diagnosed within sigmoidoscopy-accessible sites, 7,532 CRC patients (40.1%) were diagnosed within sigmoidoscopy-non-accessible sites and an additional 476 patients (2.5%) were diagnosed with unknown sub-sites. This translated into 2,853 CRC-related deaths at 5 years for sigmoidoscopy-accessible deaths versus 2,126 CRC-related deaths for sigmoidoscopy-non-accessible deaths. Additional baseline characteristics of the CRC cohort are available in Table 1. Based on the assumptions detailed above, sensitivity of screening sigmoidoscopy would be 58.8% and NPV would be 99.9%.
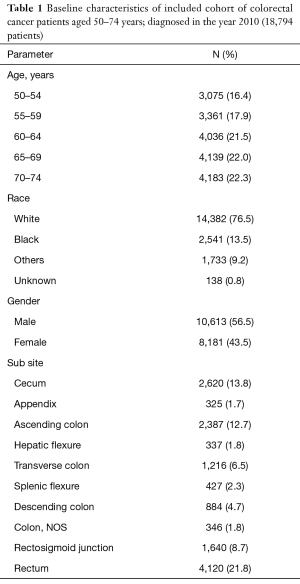
Full table
Discussion and conclusions
The current population-based study suggests that flexible sigmoidoscopy alone has a relatively low sensitivity for the detection of CRC, in particular tumors on the right-side, and thus it may be insufficient as a single screening modality. It should also be noted that the estimates in the current study were based on the assumption that all left-sided cases are successfully detected by flexible sigmoidoscopy which is likely optimistic. If additional left-sided cases were missed by flexible sigmoidoscopy, sensitivity would be poorer.
Unfortunately, previous studies have shown that colonoscopy has a limited sensitivity in the detection of right-sided CRC lesions. This has been attributed in part to poor pre-colonoscopy preparation and/or lack of experience of the endoscopists (5). Fecal testing appears to be an appropriate starting point for the screening pathway for average-risk patients. Additional studies should strive to improve the detection rates of right-sided CRC, possibly through better colonoscopy techniques or use of CT colonography.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Globocan cancer registry. Available online: globocan.iarc.fr.
- NCCN guidelines. Available online: https://www.nccn.org/professionals/physician_gls/pdf/colorectal_screening.pdf.
- Cancer guidelines Australia. Available online: https://wiki.cancer.org.au/australia/Guidelines:Colorectal_cancer
- Surveillance, Epidemiology, and End Results (SEER) Program. SEER*Stat Database: Incidence - SEER 18 Regs Custom Data (with additional treatment fields), Nov 2017 Sub (1973-2015 varying) - Linked To County Attributes - Total U.S., 1969-2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released April 2018, based on the November 2017 submission. Available online: https://seer.cancer.gov/
- Neugut AI, Lebwohl B. Colonoscopy vs sigmoidoscopy screening: Getting it right. JAMA 2010;304:461-2. [Crossref] [PubMed]


