Primary mesenteric liposarcoma: An unusual presentation of a rare condition
Introduction
Sarcomas are a heterogeneous group of malignant tumours which arise from mesenchymal tissues. Liposarcoma is one of the most common histological variants seen in adults. As per the WHO classification, the various subtypes of liposarcoma are: well-differentiated (most common), pleomorphic, round-cell, myxoid and dedifferentiated type (1). As reported by Weiss and Rao, approximately 75% of well-differentiated liposarcomas develop in the deep soft tissue of the limbs, followed by 20% in the retroperitoneum and a much smaller percentage in the inguinal region (2). Primary mesenteric liposarcoma is an extremely rare entity and so far only 17 odd cases have been reported in literature (3-19). We report here one such rare case of a large intra-abdominal liposarcoma arising from the mesentery along with a relevant review of literature regarding management.
Case report
A 50 years old man presented with history of gradually increasing lump in the left flank for the past one year. It was associated with episodes of low-grade, intermittent fever and significant weight loss in the absence of anorexia. There was no history suggestive of gastric outlet obstruction, altered bowel habits, malaena or urinary complaints. No other significant medical history was obtained. The patient had been a chronic smoker for the past 30 years. Per abdomen examination revealed a large, intra-abdominal, non-tender, approximately 20 cm × 15 cm lump occupying the whole of the left side of the abdomen and extending partly towards the right iliac fossa. It was non-mobile and not bimanually palpable. There was no free fluid in the abdomen clinically. A possibility of malignant retroperitoneal tumour was kept as the primary differential.
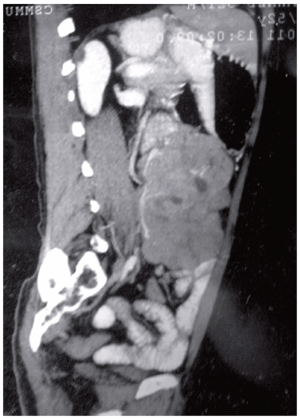
Ultrasonography revealed a complex echogenic mass without any evidence of ascites or lymphadenopathy. A 128 slice dynamic contrast enhanced CT scan of the abdomen and pelvis showed an ill-defined, multilobulated, heterogeneously enhancing, soft tissue attenuation lesion approximately 16 cm × 15 cm × 16 cm in size. The lesion was causing displacement of the bowel loops and abutting the anterior abdominal wall with well-maintained planes (Figure 1). The mesenteric vessels were posterior to the lesion. No calcification was evident. Small, rounded, non-enhancing lesions suggestive of simple cysts were seen in both kidneys. MRI showed a large lobulated mass lesion anterior to the left psoas, appearing hypointense on T1WI and heterogeneously hyperintense on T2WI. Bowel loops were displaced anteriorly. Biochemistry panel was within normal limits.
The patient was taken up for surgery after obtaining fitness for general anaesthesia. On laparotomy, a large, multilobulated tumour approximately 20 cm × 20 cm in size was seen arising from the mesentery of the jejunum. The overlying jejunal loop was densely adherent to the tumour. The tumour was not invading the superior mesenteric vessel or its main branches. The rest of the small bowel loops were pushed to the right lower quadrant and the pelvis.
The small bowel along with the growth was eviscerated and the main feeding vessel was located. The superior mesenteric vessels were identified AT AN EARLY STAGE and 2 feet of the jejunum with its involved mesentery was resected just 10 cm distal to the duodenojejunal flexure. A hand-sewn single layer anastomosis was performed to restore bowel continuity. The rest of the visualized viscera and bowel were grossly normal. No lymphadenopathy was noted.
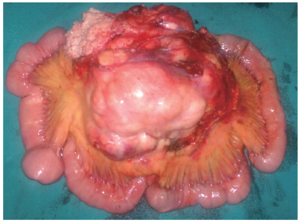
The tumour weighed approximately 1.8 kilograms (Figure 2). The cut surface had a variegated appearance with yellow/tan areas and regions of necrosis. On histopathological examination the specimen showed features suggestive of pleomorphic sarcoma. The tumour showed high mitotic activity, marked pleomorphism and intranuclear inclusions. A large number of giant cells were noted with a few showing multivacuolated cytoplasm with peripherally compressed nuclei. Tumour cells were positive for S-100 and negative for SMA/Desmin.
This patient developed an anastomotic leak on the 5th post-operative day as evidenced by bilious effluent in the intra-abdominal drain which was controlled by conservative management. The patient was advised postoperative radiotherapy and chemotherapy but he refused any further treatment and left against medical advice.
Discussion
In comparison with the retroperitoneal liposarcoma, the primary mesenteric liposarcoma is extremely rare and is treated by aggressive surgical management i.e. wide excision with adequate margins (in the absence of distant metastases). Among the malignant mesenteric tumours, lymphoma is most common followed by leiomyosarcoma. Occurring usually in the 5th to 7th decades, the incidence has been seen to be slightly higher in males (15).
Patients may present with complaints of gradual abdominal distention, pain abdomen, weight loss, early satiety and freely mobile abdominal lumps. These tumours rarely cause perforation, obstruction, intussusception, acute appendicitis or symptoms mimicking prostatism (20).
What confounded the diagnosis in this case was the finding on clinical examination of an intra-abdominal lump with very limited mobility and the subsequent core needle biopsy report of liposarcoma. The provisional diagnosis of a retroperitoneal liposarcoma was at odds with the contrast enhanced CT finding of a multilobulated heterogeneously enhancing soft tissue attenuation lesion in the left lumbar region with mesenteric vessels posterior to the lesion.
CT and MRI are indispensible for determining the tissue characteristics, size and invasion of adjacent organs (5). The reported characteristics of liposarcoma on CT images are (I) inhomogeneity, (II) infiltration or poor margination, (III) CT numbers greater than normal fat, and (IV) contrast enhancement (19). The enhancement on CT changes according to the degree of histological grade (21). Well-differentiated liposarcomas are hyperintense on T2-weighted MRI with minimal or no enhancement (22). In the present case the bowel loops were displaced anteriorly and this has been described as the 'Straddling sign' (15). The necrotic component and mass effect pointed towards the radiological diagnoses of either a GIST or sarcoma. As regards the role of gastrointestinal angiography, Hirakoba et al. have stated that it may be useful for preoperative planning (12). Liposarcomas are usually avascular to moderately vascular, and cause displacement of the major vessels. Moderately hypervascular liposarcoma may show irregular, fine tumor vessels and areas of tumor stain with early venous filling.
Among all the histological subtypes the myxoid variety is the most common, found in approximately 50% of cases. The well-differentiated type is further subdivided histologically into the inflammatory, lipoma-like, sclerosing and de-differentiated types (5) and the recently proposed 'lymphocyte-rich' type (6). Evans in 1979 reported that the median survival of patients with the well-differentiated, myxoid, dedifferentiated and pleomorphic types was 119, 113, 59 and 24 months, respectively. Thus, there was a definite correlation of the histology with the prognosis (23). Intracytoplasmic fat droplets (Oil Red O positive) are a non-specific finding and even S-100 staining may be negative in highly undifferentiated tumours. S-100 positivity has an important role in distinguishing this tumour type from malignant fibrous histiocytoma (24).
An entity known as mesenteric lipodystrophy should be kept in mind as one of the differential diagnosis of mesenteric tumour. These tumours may also present as cystic masses on imaging (14).
The treatment of choice for these tumours is surgical excision with appropriate margins followed by radiation with or without adjuvant chemotherapy in high risk patients. Pre-operative chemotherapy has been reported by one group to have been successful in shrinking a large ileocolonic mesenteric liposarcoma (17). They indicated that the key drugs to be used were doxorubicin, dacarbazine and ifosfamide. The advantages were pre-operative shrinkage of the tumour and consequently increased chances of obtaining negative margins. Also, the histological changes post- chemotherapy can guide the decision and choice of drugs for adjuvant chemotherapy. But similar results have not been replicated or reported. In the aforementioned case, the patient also received 45 Gy of post-operative irradiation. Despite a negative surgical margin and lack of nodal involvement, the patient developed a recurrence after 26 months thereby probably strengthening the case for routine adjuvant chemo/radiation. The pleomorphic lesions are considered high grade and despite clear surgical margins, a tumour size greater than 20 cm portends a poor outcome (25).
Footnote
No potential conflict of interest.
References
- DeVita VT, Lawrence TS. Rosenberg SA eds. Cancer: Principles and practice of oncology. 9th Ed. Philadelphia: Lippincott, Williams, Wilkins;2011.
- Weiss SW, Rao VK. Well-differentiated liposarcoma (atypical lipoma) of deep soft tissue of the extremities, retroperitoneum, and miscellaneous sites. A follow-up study of 92 cases with analysis of the incidence of "dedifferentiation". Am J Surg Pathol 1992;16:1051-1058. [PubMed]
- Takagi H, Kato K, Yamada E, Suchi T. Six recent liposarcomas including largest to date. J Surg Oncol 1984;26:260-267. [PubMed]
- Papadopoulos T, Kirchner T, Bergmann M, Müller-Hermelink HK. Primary liposarcoma of the jejunum. Pathol Res Pract 1990;186:803-806, discussion 807-808. [PubMed]
- Kim T, Murakami T, Oi H, et al. CT and MR imaging of abdominal liposarcoma. AJR Am J Roentgenol 1996;166:829-833. [PubMed]
- Argani P, Facchetti F, Inghirami G, Rosai J. Lymphocyte-rich well-differentiated liposarcoma: Report of nine cases. Am J Surg Pathol 1997;21:884-895. [PubMed]
- Takekawa Y, Yoshikawa T, Shibaji T, Asao Y, Nakano H. Mesenteric liposarcoma: A case report. J Nara Med Ass 1997;48:246-250.
- Amato G, Martella A, Ferraraccio F, et al. Well differentiated "lipoma-like" liposarcoma of the sigmoid mesocolon and multiple lipomatosis of the rectosigmoid colon. Report of a case. Hepatogastroenterology 1998;45:2151-2156. [PubMed]
- Calò PG, Farris S, Tatti A, Tuveri M, Catani G, Nicolosi A. Primary mesenteric liposarcoma. Report of a case. G Chir 2007;28:318-320. [PubMed]
- Khan N, Afroz N, Fatima U, Raza MH, Rab AZ. Giant primary mesenteric liposarcoma: a rare case report. Indian J Pathol Microbiol 2007;50:787-789. [PubMed]
- Cerullo G, Marrelli D, Rampone B, Perrotta E, Caruso S, Roviello F. Giant liposarcoma of the mesentery. Report of a case. Ann Ital Chir 2007;78:443-445. [PubMed]
- Hirakoba M, Kume K, Yamasaki M, Kanda K, Yoshikawa I, Otsuki M. Primary mesenteric liposarcoma successfully diagnosed by preoperative imaging studies. Intern Med 2007;46:373-375. [PubMed]
- Gupta R, Sharma A, Arora R, Kulkarni MP, Chattopadhaya TK, Singh MK. Well-differentiated mesenteric liposarcoma with osseous metaplasia: a potential diagnostic dilemma for the pathologist. J Gastrointest Cancer 2010;41:79-83. [PubMed]
- Núñez Fernández MJ, García Blanco A, López Rodríguez A, et al. Primary mesenteric liposarcoma of jejunum: presentation like a cystic mass. Minerva Med 2005;96:425-428. [PubMed]
- Burgohain J, Kathiresan N, Satheesan B. Dumbbell-shaped mesenteric liposarcoma: A case report with review of the literature. The Internet Journal of Surgery 2008;15.
- Yuri T, Miyaso T, Kitade H, et al. Well-differentiated liposarcoma, an atypical lipomatous tumor, of the mesentery: a case report and review of the literature. Case Rep Oncol 2011;4:178-185. [PubMed]
- Ishiguro S, Yamamoto S, Chuman H, Moriya Y. A case of resected huge ileocolonic mesenteric liposarcoma which responded to pre-operative chemotherapy using doxorubicin, cisplatin and ifosfamide. Jpn J Clin Oncol 2006;36:735-738. [PubMed]
- Moyana TN. Primary mesenteric liposarcoma. Am J Gastroenterol 1988;83:89-92. [PubMed]
- Ciraldo A, Thomas D, Schmidt S. Giant Abdominal liposarcoma: A Case Report. The Internet Journal of Urology 2000;1.
- Horiguchi H, Matsui M, Yamamoto T, et al. A case of liposarcoma with peritonitis due to jejunal perforation. Sarcoma 2003;7:29-33. [PubMed]
- Friedman AC, Hartman DS, Sherman J, Lautin EM, Goldman M. Computed tomography of abdominal fatty masses. Radiology 1981;139:415-429. [PubMed]
- Waligore MP, Stephens DH, Soule EH, McLeod RA. Lipomatous tumors of the abdominal cavity: CT appearance and pathologic correlation. AJR Am J Roentgenol 1981;137:539-545. [PubMed]
- Evans HL. Liposarcoma: a study of 55 cases with a reassessment of its classification. Am J Surg Pathol 1979;3:507-523. [PubMed]
- Hashimoto H, Daimaru Y, Enjoji M. S-100 protein distribution in liposarcoma. An immunoperoxidase study with special reference to the distinction of liposarcoma from myxoid malignant fibrous histiocytoma. Virchows Arch A Pathol Anat Histopathol 1984;405:1-10. [PubMed]
- Sato T, Nishimura G, Nonomura A, Miwa K. Intra-abdominal and retroperitoneal liposarcomas. Int Surg 1999;84:163-167. [PubMed]