
Survival benefits and predictors of use of chemoradiation compared with radiation alone for early stage (T1-T2N0) anal squamous cell carcinoma
Introduction
The incidence of anal cancer, a relatively rare tumor comprising less than 2.5% of all gastrointestinal tumors, is increasing due to the growing number of people infected with HIV and HPV, which are known risk factors in tumor development (1,2). Historically, anal carcinoma was treated with abdominoperineal resection (APR), a radical procedure that rendered patients colostomy-dependent (1). Despite the aggressive nature of this intervention, 5-year survival remained around 40–80% (1,2). It was not until 1974 that the utility of CRT therapy became known, when Nigro and colleagues achieved complete pathologic response in their patients utilizing a combination of radiation therapy and chemotherapy (3). Based on these preliminary results, several randomized control trials have attempted to delineate the proper radiation dose, technique, and combination chemotherapy drugs necessary to maintain remission, with the fewest side effects (1). Early stage patients have been underrepresented or excluded in randomized trials comparing CRT to radiation alone (4,5), providing limited application of overall data to patients with T1-T2N0M0 Anal SCC. As such, there is a lack of recommendations based on gold-standard randomized data or large-scale studies regarding RT versus CRT for this group of patients (6).
The purpose of the present study was to assess patterns of care and survival of CRT versus radiation alone in patients diagnosed with T1-2N0 SCC of the anus utilizing the NCDB.
Methods
The NCDB is a hospital-based cancer registry that is estimated to capture 70% of all cancer diagnosed in the United States. It is a joint collaboration between the American College of Surgeons and the Commission on Cancer. Information collected by the participating hospitals and NCDB is fully de-identified by patient and treatment center. Coded variables include demographics, staging, pathology, site-specific factors, initial treatment modalities, recurrence and survival. The data analysis in the current study has not been verified by the NCDB and they are not responsible for its validity. Exemption was obtained from the institutional review board of the NY Harbor Healthcare System Department of Veterans Affairs before the initiation of the study.
The NCDB was queried for all patients diagnosed with anal SCC (code 210–218, histology 8,070–8,078) between 2004 and 2014. Cohorts selected included those who received radiotherapy alone and chemoradiotherapy, defining patients as receiving chemoradiotherapy if initiating chemotherapy and radiation within 14 days of each other. Patients receiving CRT were compared to the cohort of patients receiving exclusively radiotherapy, without any chemotherapy at any time during their initial treatment. Patients excluded included those surviving <3 months to account for immortal time bias. The study was limited to patients receiving a radiation dose range of 4,500–5,940 cGy, consistent with definitive treatment recommendations.
The cohort was limited to patients less than 70 years old with Charlson-Deyo Comorbidity Index of 0. We stratified patients according to age (<60 vs. ≥60), gender (male vs. female), race (White, Black, other), facility type (academic vs. nonacademic). These patient characteristics were then compared between groups utilizing Pearson Chi-square and Fisher’s exact test. Univariable and multivariable logistic regression were performed to assess for predictors of CRT usage. Five-year survival was analyzed using the Kaplan-Meier method and compared using the log-rank test both for the full cohort and then on the subsets of T1 and T2 patients. Univariable and multivariable Cox regression analysis were used to assess for covariables associated with survival differences. All analyses were conducted using SPSS 24.0 and all tests were two sided with a P value <0.05 as the threshold for significance.
Results
General characteristics
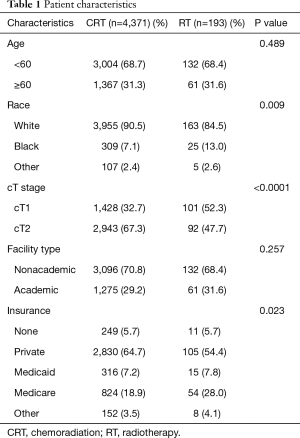
There were 4,564 patients included in the present study, of whom 4,371 (95.8%) received CRT and 193 (4.2%) received radiation alone. Median follow up was 49.8 months overall, 49.8 months in the CRT group and 48.4 months in the radiation alone group. About 86.5% of patients were still alive at last follow up, 87.2% in the CRT group and 77.7% in the radiation alone group. About 33.5% of patients had cT1N0 disease, while 66.5% of patients had cT2N0 disease. Further details of patient characteristics are available in Table 1.
Full table
Use of CRT
There was an association between CRT use and race (P=0.009), cT stage (P<0.0001) and insurance status (P=0.023) but not age (P=0.489) or facility type (P=0.257).
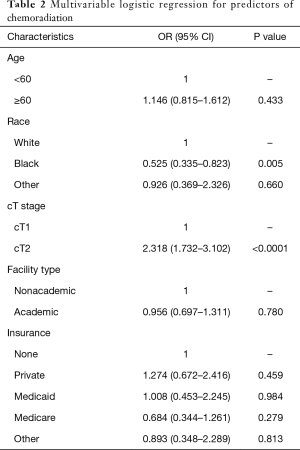
Multivariable logistic regression (Table 2) indicated that patients were less likely to receive CRT if they were of Black race compared with White race (OR 0.525, 95% CI: 0.335–0.823), and more likely to receive CRT if they had T2 disease (OR 2.318, 95% CI: 1.732–3.102). Age, facility type and insurance status were not associated with use of CRT on multivariable logistic regression.
Full table
Survival
Five-year OS was 86.3% overall, 86.6% for CRT and 79.1% for RT (Figure 1) (P=0.001). For T1 patients, 5-year OS was 89.9% overall, 90.3% with CRT and 84.7% with RT (Figure 2) (P=0.114). For T2 patients, 5-year OS was 84.4% overall, 84.7% with CRT and 72.8% with RT (Figure 3) (P<0.0001).
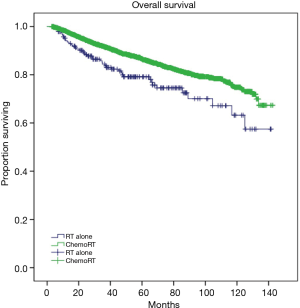
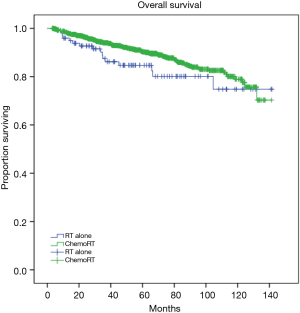
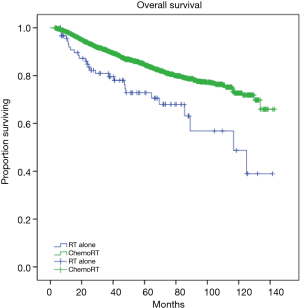
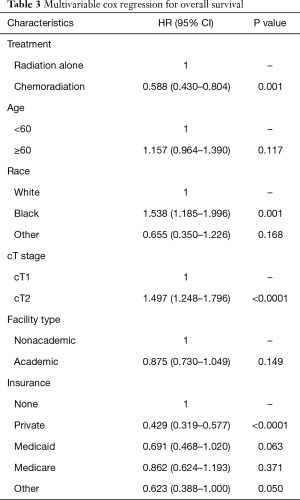
Multivariable Cox regression analysis (Table 3) confirmed significance of association between survival and CRT use (HR 0.588, 95% CI: 0.430–0.804, P=0.001) for the full cohort. Repeat multivariable analysis on the subset of T2N0 patients also confirmed significance of association between CRT and improved survival (HR 0.515, 95% CI: 0.349–0.761, P=0.001). For the subset of T1N0 patients, however, survival was not improved with the use of CRT on multivariable analysis (HR 0.731, 95% CI: 0.434–1.232, P=0.239). Overall survival was also significantly improved for patients of White race (P=0.001 compared with Black race), cT1N0 disease (P<0.0001), as well as private insurance (P=0.023).
Full table
Discussion
This hospital-based study of 4,564 patients with T1-T2N0M0 anal cancer treated with CRT versus radiation alone identified several key findings. First, there were extremely high rates of utilization of CRT in this cohort, 95.8%. We also found a significant difference in overall survival between the two groups: 5-year OS 86.6% for CRT and 79.1%% for radiation alone (P=0.001). This finding was sustained on multivariate analysis (HR 0.588, 95% CI: 0.430–0.804, P=0.001). However, on subset analysis, the survival benefit was limited to T2 tumors (HR, 95% CI) and not seen with T1 tumors (HR, 95% CI).
To date, there have been no controlled trials which have found an improvement in overall survival particularly for T1-2N0 disease. However, several randomized control trials have given objective assessments of the value of combined CRT over radiation therapy alone for all patients with anal SCC. In their study of CRT therapy versus radiation alone, Bartelink et al. randomized 110 patients with T3-T4N0-3 or T1-2N1-3 anal cancer to 45 Gy alone, versus combined fluorouracil and mitomycin and radiation therapy. The investigators found a complete remission rate of 80% vs. 54% (not including results after surgical resection), respectively, a colostomy free rate 32% higher in the combined therapy group, a significantly improved progression free survival, and no significant differences in toxicity between the two arms (4). Although the authors did not report a significant difference in survival between the two groups (3-year survival 72% vs. 65%, P=0.17), this may likely be due to the lower power given the sample size and the short median follow up time of 42 months in patients with locally advanced disease (4). Because patients with T1-2N0 disease were not included in their study, however, its findings may not be generalizable to patients with earlier stage tumors.
The United Kingdom Coordinating Committee on Cancer Research (UKCCCR) Anal Canal Trial Working Party performed the ACT I trial, which randomized 585 patients with anal cancer to radiation therapy alone versus radiation with concurrent chemotherapy (5). Local control was significantly improved in the combined CRT therapy group (64% vs. 41%, P<0.0001). The mortality rate from anal cancer at 3 years was also significantly higher in the radiotherapy alone arm (28% vs. 39%, P=0.02) although, the 3-year overall survival did not differ between the arms (65% vs. 58%, P=0.25) (5). In a 13-year follow-up of the first UKCCCR Anal Cancer Trial, Northover et al. reported a 25% reduction in locoregional relapse (HR 0.46, P<0.001), and a statistically significant reduction in the risk of dying from anal cancer (HR 0.67, P=0.004). The authors attributed a lack of significance in overall survival to an excess of deaths not from anal cancer in the CMT group in the first 5 years (7). Although these results are significant for patients with advanced tumor characteristics, T1N0 patients were excluded from this study.
Our study showed an extremely high utility rate of CRT. Unfortunately, there is a lack of data regarding optimal treatment approach for early stage anal cancer. Although the aforementioned large clinical trials had underrepresented cT1-T2N0 subjects, if not outright excluded them, they were still included in some studies showing improved outcomes, likely explaining the high usage rate. An additional explanation for the large percentage of patients receiving CRT in our study may be that we selected for patients more likely to tolerate chemotherapy due to younger age and fewer comorbidities. A prior NCDB study of 11,918 patients age >50 years with anal SCC found that 49.5% of patients did not complete recommended chemoRT. Factors associated with failure to complete therapy included older age at diagnosis and higher Charlson-Deyo score (8). In the present study, we excluded patients >70 years old and Charlson-Deyo of 1 or higher.
Still, some retrospective studies have shown differing results on the need for multimodal treatment. In a SEER study with a slightly older population Medicare population, Buckstein et al. found that, after propensity scoring for potential confounding factors, 200 patients received CRT versus 99 patients who received radiation alone, and there was no difference in overall survival, cause-specific survival, colostomy free survival, or disease-free survival with the use of CRT (9). In another retrospective study of 69 patients with Tis and T1 anal cancer, Ortholan et al. demonstrated a 5-year survival rate of 94% with only radiation therapy (40–60 Gy) (10). While these two studies have shown lack of additional benefit of chemotherapy, in another study, crude survival rates of 81% and 78% in T1 and T2 patients treated with only RT, were improved to 92% and 91.5% for T1 and T2, after the addition of a pool of patients who received concomitant chemoRT (11). Similarly, Myerson et al. observed a 5-year DFS rate of 93% and 87% with CRT in T1 and T2 patients, respectively (12). Due to multiple studies showing opposing findings, the use of combined CRT in early stage anal cancer is controversial, and concurrent chemoRT is recommended as first-line treatment only for patients with stage II or higher disease (13).
In an NCDB study by Churilla et al, amongst 7,800 patients with T1-T2N0M0 SCC of the anal canal, the authors found that 93.5% of patients received CRT (14). Additionally, they reported that patients who did not receive chemotherapy were more likely to receive high-dose radiation therapy. Although treatment decisions may favor dose-escalation when chemotherapy is either not preferred or contraindicated, this practice may not have additional benefits to patients: in their NCDB study, Prasad et al. demonstrated that high-dose RT (≥5,940 cGy) was not associated with improved overall survival in patients with tumor size >5 cm (15). There are a few differences between our study and the aforementioned study by Churilla and co-authors. Our study found 96% of patients with early stage anal SCC received CRT. This small difference is likely due to differences in patient selection as we limited inclusion to patients younger than 70 years old, who received radiation doses between 4,500–5,940 cGy. Additionally, the purpose of their study was to characterize associations between variations in radiation dose, single versus multi-agent chemotherapy, and patient/tumor characteristics, whereas the purpose of our study was to describe patterns between receipt of RT versus CRT and patient/tumor characteristics, and impact on overall survival between the two treatment arms (14).
Finally, we found that overall survival was significantly improved for the subset of patients with cT2N0 disease. These results underscore the benefits of multimodality therapy in patients with tumors smaller than 5 cm, as size >5 cm was shown to be associated with poor survival despite the use of CRT (16). Similarly, Flam et al. reported that the only stratifying variable that significantly influenced the presence of residual disease was primary tumor size less than 5 cm (93% vs. 83%, P=0.02) (17). Surprisingly, Bartelink et al. did not find that age, initial performance status, or tumor length had any significant prognostic value (4). However, the authors only included patients with T3-T4N0 or T1-T2N1-3 disease, tumor characteristics which have been confirmed to have a worse prognostic role in locoregional control, distant control, disease free survival, and overall survival (18-20).
The limitations of our study are akin to those of any retrospective data such as inability to account for selection bias. Additionally, we were not able to assess patient HIV status. Since anal cancer is not an AIDS defining illness, patients with HIV may still have a Charlson Deyo score of 0, compared to patients with AIDS who have a minimum score of 6. The HIV status may also have influenced decisions regarding receipt of chemotherapy. Other limitations include nonverification of coding, lack of information regarding specific chemotherapy received, cancer recurrence or cause of death. The strengths of this study include the large patient sample from a highly representative database.
In conclusion, our NCDB study of 4,564 early stage anal cancer patients found that patients are more likely to receive combined CRT therapy if they are of younger age, with higher performance status, and larger primary tumor size. We also found an improved overall survival in patients receiving combined modality treatment versus radiation therapy alone.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Exemption was obtained from the institutional review board of the NY Harbor Healthcare System Department of Veterans Affairs before the initiation of the study.
References
- Salati SA, Al Kadi A. Anal cancer - a review. Int J Health Sci (Qassim) 2012;6:206-30. [Crossref] [PubMed]
- Uronis HE, Bendell JC. Anal cancer: an overview. Oncologist 2007;12:524-34. [Crossref] [PubMed]
- Nigro ND. An evaluation of combined therapy for squamous cell cancer of the anal canal. Dis Colon Rectum 1984;27:763-6. [Crossref] [PubMed]
- Bartelink H, Roelofsen F, Eschwege F, et al. Concomitant radiotherapy and chemotherapy is superior to radiotherapy alone in the treatment of locally advanced anal cancer: results of a phase III randomized trial of the European Organization for Research and Treatment of Cancer Radiotherapy and Gastrointestinal Cooperative Groups. J Clin Oncol 1997;15:2040-9. [Crossref] [PubMed]
- Epidermoid anal cancer: results from the UKCCCR randomised trial of radiotherapy alone versus radiotherapy, 5-fluorouracil, and mitomycin. UKCCCR Anal Cancer Trial Working Party. UK Co-ordinating Committee on Cancer Research. Lancet 1996;348:1049-54. [Crossref] [PubMed]
- Glynne-Jones R, Nilsson PJ, Aschele C, et al. Anal cancer: ESMO-ESSO-ESTRO clinical practice guidelines for diagnosis, treatment and follow-up. Eur J Surg Oncol 2014;40:1165-76. [Crossref] [PubMed]
- Northover J, Glynne-Jones R, Sebag-Montefiore D, et al. Chemoradiation for the treatment of epidermoid anal cancer: 13-year follow-up of the first randomised UKCCCR Anal Cancer Trial (ACT I). Br J Cancer 2010;102:1123-8. [Crossref] [PubMed]
- Motz BM, Lorimer PD, Walsh KK, et al. Utilization of primary chemoradiotherapy for anal squamous cell carcinoma in the elderly: An analysis of the NCDB. J Clin Oncol 2017;35:abstr 726.
- Buckstein M, Arens Y, Wisnivesky J, et al. A population-based cohort analysis of chemoradiation versus radiation alone for definitive treatment of stage I anal cancer in older patients. Dis Colon Rectum 2018;61:787-94. [PubMed]
- Ortholan C, Ramaioli A, Peiffert D, et al. Anal canal carcinoma: early-stage tumors & < or =10 mm (T1 or Tis): therapeutic options and original pattern of local failure after radiotherapy. Int J Radiat Oncol Biol Phys 2005;62:479-85. [Crossref] [PubMed]
- Deniaud-Alexandre E, Touboul E, Tiret E, et al. Results of definitive irradiation in a series of 305 epidermoid carcinomas of the anal canal. Int J Radiat Oncol Biol Phys 2003;56:1259-73. [Crossref] [PubMed]
- Myerson RJ, Outlaw ED, Chang A, et al. Radiotherapy for epidermoid carcinoma of the anus: thirty years' experience. Int J Radiat Oncol Biol Phys 2009;75:428-35. [Crossref] [PubMed]
- Zilli T, Schick U, Ozsahin M, et al. Node-negative T1-T2 anal cancer: radiotherapy alone or concomitant chemoradiotherapy? Radiother Oncol 2012;102:62-7. [Crossref] [PubMed]
- Churilla TM, DeMora L, Handorf E, et al. Deviations from standard chemoradiation among early-stage anal cancer patients. Int J Radiat Oncol Biol Phys 2018;100:945-9. [Crossref] [PubMed]
- Prasad RN, Elson J, Kharofa J. The effect of dose escalation for large squamous cell carcinomas of the anal canal. Clin Transl Oncol 2018;20:1314-20. [Crossref] [PubMed]
- Kapacee ZA, Susnerwala S, Wise M, et al. Chemoradiotherapy for squamous cell anal carcinoma: a review of prognostic factors. Colorectal Dis 2016;18:1080-6. [Crossref] [PubMed]
- Flam M, John M, Pajak TF, et al. Role of mitomycin in combination with fluorouracil and radiotherapy, and of salvage chemoradiation in the definitive nonsurgical treatment of epidermoid carcinoma of the anal canal: results of a phase III randomized intergroup study. J Clin Oncol 1996;14:2527-39. [Crossref] [PubMed]
- Das P, Bhatia S, Eng C, et al. Predictors and patterns of recurrence after definitive chemoradiation for anal cancer. Int J Radiat Oncol Biol Phys 2007;68:794-800. [Crossref] [PubMed]
- Gunderson LL, Moughan J, Ajani JA, et al. Anal carcinoma: impact of TN category of disease on survival, disease relapse, and colostomy failure in US Gastrointestinal Intergroup RTOG 98-11 phase 3 trial. Int J Radiat Oncol Biol Phys 2013;87:638-45. [Crossref] [PubMed]
- Myerson RJ, Kong F, Birnbaum EH, et al. Radiation therapy for epidermoid carcinoma of the anal canal, clinical and treatment factors associated with outcome. Radiother Oncol 2001;61:15-22. [Crossref] [PubMed]


