
Disparities in colon and rectal cancer queried individually between Hispanics and Whites
Introduction
Colorectal cancer (CRC) is the third most commonly diagnosed cancer and the second leading cause of cancer related deaths in the United States (1). Furthermore, in 2012, CRC was the second most commonly diagnosed cancer in the Hispanic population, the fastest growing ethnic group in the U.S. (2-3). This makes studying CRC in this population, especially significant.
Consistent with the literature, our recent published study showed that the incidence of early-onset (EO) CRC (<50 years old) has been increasing in both the Hispanic and non-Hispanic white population (4). This is a concerning trend as EO CRC has been shown to be more aggressive and presents at a higher stage (5). Our study, in addition, demonstrated that disparities in CRC do exist between Hispanics and Whites for the late-onset (LO) population (>50 years old). Whites with LO CRC were found to have a decreasing incidence while Hispanics with LO CRC had an increasing incidence (4). It was unclear, however, whether this increase in EO CRC and disparity in LO CRC were attributable to colon cancer (CC) or rectal cancer (RC).
CC and RC cancer are largely grouped together as CRC; however, this may not be the most appropriate grouping for research and treatment purposes. There are alterations at the genomic level, vasculature and histology between CC and RC, as well as differences in outcomes, as patients with RC experience complications more often after surgery compared to patients with CC (6-8). Furthermore, there are different risk factors for CC vs. RC and stronger associations between one cancer type and a certain risk factor than the other; this occurs with factors such as family history, physical activity and cigarette smoking (9).
Due to the increase in incidence of the more aggressive EO CRC in Hispanics and Whites and the racial disparity that exists for LO CRC, our study seeks to query CC and RC individually in order to determine whether there are differences in incidence between the two cancer types.
Methods
Study population
Using the Surveillance, Epidemiology, and End Results (SEER) database, we performed a 10-year (2000 to 2010) retrospective analysis including white non-Hispanic and white-Hispanic patients with CC and RC that were reported.
Data source
The SEER Program of the National Cancer Institute (NCI) is an authoritative comprehensive source of population-based information in the United States that collects data on stage of cancer at the time of diagnosis, patient survival data, information on patient demographics, primary tumor site, tumor morphology, first course of treatment and follow-up for vital status. The SEER data are submitted to the NCI from population-based cancer registries that have collected data from various health providers including hospitals, clinics, laboratories and public records. The population data used in calculating cancer rates are obtained and updated from the US Census Bureau.
The SEER 18 registries consist of cancer data from Greater California, Greater Georgia, Kentucky, Louisiana, and New Jersey diagnosed from 2000 and later, along with the original SEER 13 registries consisting of cancer data from Los Angeles, San Jose-Monterey, rural Georgia, and the Alaska Native Tumor Registry diagnosed after 1992 and the original SEER 9 registries with cancer data from Atlanta, Connecticut, Detroit, Hawaii, Iowa, New Mexico, San Francisco-Oakland, Seattle-Puget Sound, and Utah that were added in 1973. SEER currently collects and publishes cancer incidence and survival data from population-based cancer registries covering approximately 28% of the US population [Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1973 to 2013), National Cancer Institute, DCCPS, Surveillance Research Program, Surveillance Systems Branch, released April 2016, based on the November 2015 submission]. SEER coverage in its current form includes 25% Whites, 26% African Americans, 38% Hispanics, 44% American Indians and Alaska Natives, 50% Asians, and 67% Hawaiian and Pacific Islanders.
Data points collected
The SEER database was accessed via the free public Web site at www.seer.cancer.gov, which provides limited access to the stored database. Using the Cancer Query System, the database was queried for incidence of CC and RC in white non-Hispanics and white-Hispanics for each year from 2000 to 2010 (the most recent year data can be queried). This query was run from SEER 18 registries. This was done for each predefined 5-year age group beginning with 0 to 4 years of age and ending with 85+ years old. Individual ages or other 5-year age groups cannot be selected within this system. These data were then exported to a Microsoft Excel spreadsheet and appropriate line graphs were created. Next, using the available option of combined data from all 18 registries (available since 2000) during 2000 to 2010, we determined the incidence of these cancers at different locations in the colon and rectum in each of these age groups. The available locations included cecum, appendix, ascending colon, hepatic flexure, transverse colon, splenic flexure, descending colon, sigmoid, recto-sigmoid and rectum. From these incidences, the percentage of tumors at each location was determined. The available stages of CC and RCs included localized (stage I and stage II), regional (stage III) and distant (stage IV) cancers. These data were then transferred to a spreadsheet for ease of comparison.
Outcome measures
The outcome measures were trends in incidence of CC and RCs in two age groups, the EO group (<50 years old) and LO group (>50 years old) and differences in gender, racial and stage of disease characteristics between white non-Hispanic and white-Hispanic patients. Incidence was defined as the number of cases diagnosed with CC and RC from 2000 through 2010.
Statistical analysis
Trend analysis was performed using the linear regression analysis. All statistical analyses were performed using Statistical Package for Social Sciences (SPSS, Version 20; SPSS, Inc., Chicago, IL, USA). This study was reviewed by the University of Arizona, Institutional Review Board and was determined to be exempt from the need for approval (IRB 1608829801).
Results
During the 10-year study period, there were a total of 23,847 CC cases and 8,474 RC cases reported for Hispanics and a total of 246,440 CC cases and 69,885 RC cases reported for Whites in the SEER database.
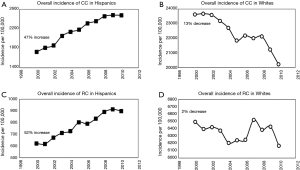
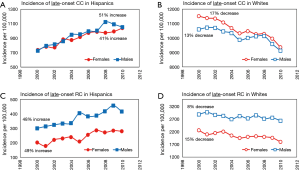
Trends in overall incidence of both CC and RC varied significantly between the two racial groups. In Hispanics, the overall incidence of CC and RC increased by 47% and 52%, respectively; while in Whites, the overall incidence of CC and RC decreased by 13% and 2% respectively (Figure 1). The difference in incidence trends between Hispanics and Whites for CC was found to be statistically significant at P<0.0001.
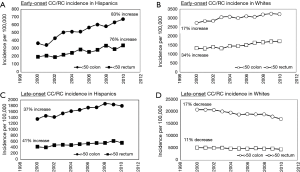
Incidence of EO CC increased in both Hispanics and Whites by 83% and 17% respectively. Moreover, similar increasing trends in incidence of EO RC were observed for both racial groups with a 76% increase in Hispanics and a 34% increase in Whites (Figure 2A,B). However, although both groups have an increasing incidence for EO RC, these trends were still found to have a P value less than alpha =0.05 (P=0.04) suggesting that the rates of increase vary significantly. In the case of LO CC, the incidence increased by 37% in Hispanics while it decreased by 17% in Whites; this data represents a statistical significance between LO CC incidence of Hispanics and Whites (P<0.0001). Similarly, for LO RC, the trend in incidence increased in Hispanics by 41%, but decreased in Whites by 11% (Figure 2C,D).
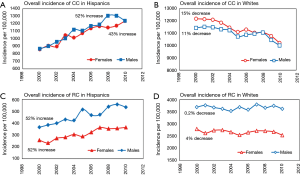
CC was more prevalent in Hispanic males and white females. The trend analysis revealed significant differences in incidence between the two racial groups (Figure 3A,B). While there was a startling increasing incidence of CC observed in Hispanic males (52%) and females (43%) (Figure 3A), the incidence of CC showed decreasing trends in both white males (11%) and white females (15%) (Figure 3B). RC was more prevalent in males for both racial groups. Similarly, as for CC, trends in overall incidence of RC varied significantly between Hispanics and Whites. Significant increases of 52% were seen in both Hispanic males and females (Figure 3C); however, a 4% decrease was observed in white females and a 0.2% decrease in white males (Figure 3D).
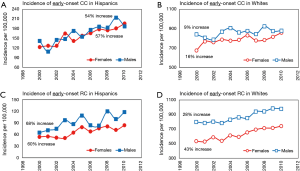
Both, EO CC and EO RC were more prevalent in males for both racial groups compared to females. Furthermore, incidence of both cancer types showed increasing trends in both genders. As documented in Figure 4A,B, a higher increase in incidence of EO CC was seen in Hispanic males (54%) and females (57%) compared to white males (9%) and females (16%). Similar trends were observed for EO RC but with a much higher increase seen in Whites. As shown in Figure 4C, incidence of EO RC increased in both Hispanic males and females by 68% and 60% respectively. Similarly, Figure 4D shows a 28% increase in white males and 43% increase in white females.
Despite increasing trends in incidence of EO disease for both cancer types (CC, RC) as well as for both genders and racial groups, racial differences were observed in trends of LO disease for both genders and both cancer types. As documented by Figure 5A,B, incidence of LO CC increased in both Hispanic males (51%) and Hispanic females (41%) while decreasing in white males (13%) and white females (17%). Similarly, increasing trends of approximately 48% were observed in incidence of LO RC in Hispanic males and females (Figure 5C), while there were decreasing trends observed in white males (8%) and white females (15%) as shown in Figure 5D.
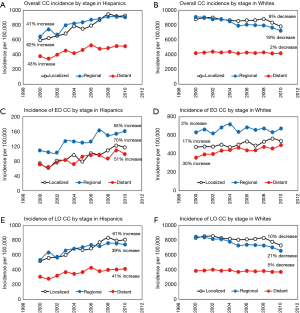
From a total number of CC tumors being diagnosed in Hispanics during the 10-year study period, 38% were localized, 40% regional and 22% distant (Figure S1). The overall incidence has increased for CC tumors of all stages (localized, regional and distant) during the 10-year study period for Hispanics while it decreased in Whites (Figure 6A,B). The most profound increase of 62% was observed in the group of Hispanic patients with regional tumors while the most profound decrease of 19% was seen in the same group of white patients. In Hispanics with EO CC, 30% of tumors were localized, 43% regional and 27% distant (Figure S1). Over the 10-year period, the incidence of localized EO CC tumors increased by 55%, regional tumors by 70% and incidence of distant tumors increased by an alarming 51% in Hispanics (Figure 6C). Similar trends with the highest increase in incidence of distant CC were observed in young Whites (Figure 6D). The rising trends in incidence of all stages of LO CC in Hispanics and decreasing trends in Whites mirrored the trends seen in overall incidence of CC for both racial groups (Figure 6E,F).
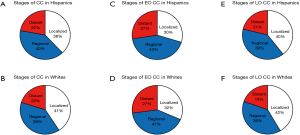
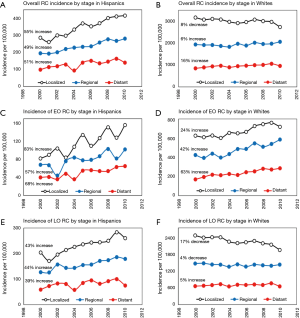
From a total number of RC tumors being diagnosed in Hispanics during the 10-year study period, 49% were localized, 33% regional and 18% distant (Figure S2). The overall incidence has increased for all stages of RC tumors by approximately 50% in Hispanics. In Whites, incidence of localized RC decreased by 8%, but incidence of regional and distant RC has increased by 6% and 16% respectively (Figure 7A,B). As with EO CC, incidence of EO RC showed increasing trends for both Hispanics and Whites with the highest 63% increase for distal EO CRC in Whites and 83% for localized tumors in Hispanics (Figure 7C,D). From all EO RC tumors, 47% of tumors were localized, 32% regional and 21% distant while in Whites there was 17% distant EO RC tumors (Figure S2). In addition, there was a 4% higher percentage of distant EO RC tumors compared to LO RC in Hispanics. The incidence of all stage LO RC tumors showed increasing trends in Hispanics with about 40% increase (Figure 7E). In Whites with LO RC tumors, the incidence of localized and regional tumors decreased by 17% and 5% respectively, while the incidence of distant LO RC tumors increased by 4% (Figure 7F).

Discussion
This 10-year SEER study showed that for both ethnicities, there is an increase in incidence of both EO CC (83% increase for Hispanics and 17% increase for Whites) and EO RC (76% increase for Hispanics and a 34% increase for Whites). The increase in incidence for EO CC and RC is consistent with a previous study analyzing CC vs. RC; however, this other study reported that in comparison to CC, RC incidence rates were increasing faster than CC incidence rates, which we only discovered to be true for the white population (10). We found that for Hispanics, there is a greater increase for CC than RC demonstrating the impact ethnicity can have on incidence. The reason EO CC and RC may be increasing in incidence is likely multifactorial. We postulate that there is an environmental component, including a change in the gut microbiome, as well as a genetic component as described in our previous molecular studies (11,12). The fact that the recommended screening age for CRC is 50 years old and colonoscopies are proven to help prevent CRC does not help the incidence in patients under 50 years old. Without screening patients do not have the opportunity to have polyps removed before they can become cancerous. Furthermore, in this younger population, key symptoms may go unrecognized, which may further contribute to increased incidence (13).
We found that for EO CC and RC in Hispanics, the incidence of distant tumors has increased over the 10-year period by 51% and 68% respectively. In Whites, this incidence is also increasing by 30% for EO CC and 63% for EO RC. These results are consistent with EO CRC being more aggressive as well as EO CRC being more likely to be found in the rectum (or distal colon) (13). Overall, these EO tumors have been found to be poorly differentiated, have mucinous and signet ring features, and present at advanced stages (13). Previous studies have shown that EO CRC may have a different molecular basis compared to LO making it important to distinguish between the two subsets (and even further differentiate between CC and RC) (11,12,14). This has also been demonstrated solely for sporadic EO rectal cancer demonstrating it is characterized by distinct molecular events compared to LO disease (11). However, it is important to note our finding that RC has a greater increasing incidence of distant tumors in comparison to CC because RC is associated with more complications compared to CC and also more greatly metastasizes to the thorax, nervous system and bone (8,15).
While the incidence of LO CC and RC in Whites is decreasing (decrease of 17% for LO CC and 11% for RC), the incidence of LO CC and RC in Hispanics is alarmingly increasing (37% increase for LO CC and 41% increase for LO RC). The decrease in LO CC and RC for Whites is what would be expected for all groups due to recommended CRC screening at 50; however, the increasing incidence for LO CC and RC in Hispanics represents a disparity. One study found that potentially identifiable groups of Hispanics (including greater reported fear of colonoscopy testing) were less likely to adhere to his/her physician’s screening colonoscopy recommendation (16). Another reason Hispanics may not be receiving colonoscopies is because they have the greatest percentage of low socioeconomic status (SES) patients (Whites have the greatest percentage of high SES patients) and this may be a barrier to screening (17).
We found that while overall the prevalence of CC and RC is greater in males than females, for Whites with LO CC, the prevalence was higher in females compared to males. This was not well established by our previous study where we found the LO CRC group for Whites had a greater proportion of males than females (4). This is because having CC and RC combined as CRC hid this finding. The reason for LO CC prevalence being greater in females than males may be due to the fact that women live longer than men and therefore there is a greater population of women that are susceptible to CC during the later ages of life in comparison to the number of living men. The reason this may not have been reflected in the RC group is that while the median age of diagnosis for CC is 68 in men and 72 in women, for RC it is the same for both sexes at a younger age of 63 years old, therefore allowing the trend of men with CRC having greater prevalence remaining prominent (18).
Conclusions
This study established that the incidence of CC and RC are different and there is racial disparity in incidence between Whites and Hispanics. This study, hopefully, will help in crafting public policy that might help in addressing this disparity.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: This study was reviewed by the University of Arizona, Institutional Review Board and was determined to be exempt from the need for approval (IRB 1608829801).
References
- Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin 2015;65:5-29. [Crossref] [PubMed]
- Jafri NS, Gould M, El-Serag HB, et al. Incidence and survival of colorectal cancer among Hispanics in the United States: a population-based study. Dig Dis Sci 2013;58:2052-60. [Crossref] [PubMed]
- Siegel R, Naishadham D, Jemal A. Cancer statistics for Hispanics/Latinos, 2012. CA Cancer J Clin 2012;62:283-98. [Crossref] [PubMed]
- Koblinski J, Jandova J, Nfonsam V. Disparities in incidence of early- and late-onset colorectal cancer between Hispanics and Whites: A 10-year SEER database study. Am J Surg 2018;215:581-5. [Crossref] [PubMed]
- Yantiss RK, Goodarzi M, Zhou XK, et al. Clinical, pathologic, and molecular features of early-onset colorectal carcinoma. Am J Surg Pathol 2009;33:572-82. [Crossref] [PubMed]
- Cancer Genome Atlas Network. Comprehensive molecular characterization of human colon and rectal cancer. Nature 2012;487:330-7. [Crossref] [PubMed]
- Pilati C, Blons H, Laurent-Puig P. Molecular differences between colon and rectal cancer. Eur J Cancer 2014;50:S1-8. [Crossref]
- Zafar SN, Shah AA, Hashmi ZG, et al. Outcomes after emergency general surgery at teaching versus nonteaching hospitals. J Trauma Acute Care Surg 2015;78:69-76; discussion 76-7. [Crossref] [PubMed]
- Wei EK, Giovannucci E, Wu K, et al. Comparison of risk factors for colon and rectal cancer. Int J Cancer 2004;108:433-42. [Crossref] [PubMed]
- Siegel RL, Fedewa SA, Anderson WF, et al. Colorectal Cancer Incidence Patterns in the United States, 1974-2013. J Natl Cancer Inst 2017. [Crossref] [PubMed]
- Nfonsam V, Xu W, Koblinski J, et al. Gene Expression Analysis of Sporadic Early-Onset Rectal Adenocarcinoma. Gastrointest Cancer (Jersey City) 2016;1(1).
- Jandova J, Xu W, Nfonsam V. Sporadic early-onset colon cancer expresses unique molecular features. J Surg Res 2016;204:251-60. [Crossref] [PubMed]
- Ahnen DJ, Wade SW, Jones WF, et al. The increasing incidence of young-onset colorectal cancer: a call to action. Mayo Clin Proc 2014;89:216-24. [Crossref] [PubMed]
- Silla IO, Rueda D, Rodriguez Y, et al. Early-onset colorectal cancer: A separate subset of colorectal cancer. World J Gastroenterol 2014;20:17288-96. [Crossref] [PubMed]
- Riihimäki M, Hemminki A, Sundquist J, et al. Patterns of metastasis in colon and rectal cancer. Sci Rep 2016;6:29765. [Crossref] [PubMed]
- Jibara G, Jandorf L, Fodera MB, et al. Adherence to Physician Recommendation to Colorectal Cancer Screening Colonoscopy Among Hispanics. J Gen Intern Med 2011;26:1124-30. [Crossref] [PubMed]
- Kim J, Artinyan A, Mailey B, et al. An interaction of race and ethnicity with socioeconomic status in rectal cancer outcomes. Ann Surg 2011;253:647-54. [Crossref] [PubMed]
- American Cancer Society. Colorectal Cancer Facts & Figures 2017-2019. Atlanta: American Cancer Society, 2017.


