The association of H. pylori and colorectal adenoma: does it exist in the US Hispanic population?
Introduction
Helicobacter pylori (H. pylori), a spiral-shaped pathogenic bacterium found on the human gastric mucosa, was first isolated by Warren and Marshall (1). According to the CDC data, the estimated prevalence of H. pylori infection is 70% in developing countries and 30-40% in the United States and other industrialized countries (2). Seroprevalence of H. pylori increases with age, lower socioeconomic class and race with a higher incidence and prevalence found in Hispanic and African Americans versus Whites (3).
H. pylori infection has been associated with inflammatory processes like chronic gastritis, peptic ulcer disease and gastric adenocarcinoma (4). An association between H. pylori and colorectal adenoma has been demonstrated in non-Hispanic populations (5,6). From in vivo and in vitro experiments, it appears that H. pylori infection promotes tumor formation in extra-gastric organs through at least two hypothesized mechanisms (7-9). One explanation may occur through a direct carcinogenic effect from the H. pylori’s contact with the colonic mucosa. Another etiology may occur indirectly through increased gastrin levels caused by H. pylori infection, leading to a trophic effect on colonic epithelial cell growth and differentiation (10,11).
Data regarding colorectal adenomas and their association with H. pylori infection is scarce in the Hispanic population. Our aim was to study the association of adenoma detection and biopsy proven H. pylori infection in a cohort of Hispanic population.
Methods
Study population
Data were collected from Nassau University Medical Center, a 530-bed tertiary care teaching hospital in East Meadow, New York. Patients who underwent both an esophagogastroduodenoscopy (EGD) and colonoscopy from July 2009 to March 2011 were pulled from an electronic database. A total of 1,737 patients completed colonoscopies during this time with 95 excluded for the following reasons: 17 inflammatory bowel disease, 12 malignancy, 22 prior history of colorectal adenoma, and 44 were incomplete colonoscopies defined as no cecal intubation. Among the colonoscopies included for this study, 799 patients had EGD’s performed prior to colonoscopies for evaluation of gastrointestinal bleeding, dysphagia, unexplained iron deficiency anemia, unintentional weight loss, persistent abdominal pain and esophageal reflux symptoms despite appropriate treatment (12). Of these individuals, 335 were Hispanic patients. The EGD biopsies were reviewed for H. pylori organisms with the results recorded as either H. pylori positive or negative. These 335 Hispanic patients also underwent either screening or diagnostic colonoscopy results were reviewed and recorded.
Statistical analysis
The following variables were recorded for each subject: age, sex, race, BMI, diabetes, hypertension, dyslipidemia, alcohol use, tobacco use, family history of colorectal cancer and H. pylori status. Additionally, presence, number, size and location of colorectal adenomas were recorded.
Analyses were conducted using SAS version 9.1 (SAS Institute, Cary, NC).
Associations between groups were tested using a Chi-Square statistic for categorical variables and a t-test for continuous variables. Age, sex, race, alcohol use and tobacco use -adjusted odds ratios and their 95% confidence intervals (CIs) were estimated using unconditional logistic regression models. Statistical significance was assessed using a two sided test at the alpha =0.05 level for all studies.
Results
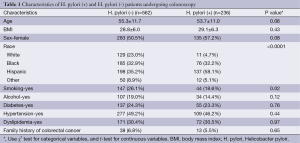
Table 1 shows the characteristics of the H. pylori negative and positive patient populations meeting the criteria for our study. The mean age of the H. pylori positive and negative groups was 53.7 and 55.3 respectively but this did not reach statistical significance (P=0.06). The mean body mass index (BMI) between the two groups was in the overweight range of 29.1 and 28.8 respectively and was also not different (P=0.43). The racial discrepancy in the H. pylori positive group was significantly different between the groups (P<0.0001). In the H. pylori positive population, 58.1% (n=137) were Hispanic vs. 35.3% (n=198) in the H. pylori negative patients. In contrast, 4.7% were White in the H. pylori positive group vs. 23.0% (n=129) in the H. pylori negative population. The majority of patients in our population were Hispanics followed by Blacks and Whites respectively (P<0.001). Smoking and alcohol were lower in the H. pylori group, 18.6% (n=44) vs. 26.1% (n=147) for smoking (P=0.02) and 14.4% (n=34) vs. 19% (n=107) for alcohol (P=0.12), respectively. Diabetes, dyslipidemia and hypertension distribution did not differ between the two groups.
Full table
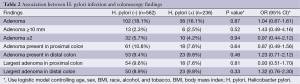
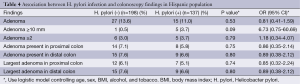
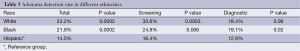
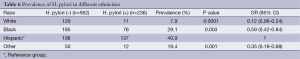
Table 2 shows the association between H. pylori and combined colonoscopic findings. There were no statistically significant associations seen between H. pylori infection and colonoscopic findings. Table 3 shows the demographic characteristics of the Hispanic population meeting inclusion criteria. There were no statistically significant differences between H. pylori positive and negative individuals in terms of mean age, BMI, sex, smoking, alcohol, diabetes, hypertension, dyslipidemia, or history of colorectal cancer. Table 4 shows that there were no significant associations between H. pylori infection and colonoscopic findings in the Hispanic study population. Table 5 shows the total adenoma detection rate (ADR) was highest in the Whites (23.2%, P=0.0002) followed by Blacks (21.8%, P=0.0002) in comparison to the Hispanics (14.5%). Table 6 compares prevalence of H. pylori in Hispanics with other races. It shows that highest prevalence was seen in Hispanics 40.9% vs. BBlacks (29.1%, P=0.003) followed by other races (19.4%, P=0.001) then Whites (7.9%, P=0.0001).
Full table

Full table
Full table
Full table
Full table
Discussion
In our Hispanic cohort we did not find an association between H. pylori infection and the presence of colorectal adenoma. Meta-analysis have previously shown a small to modest association between colorectal adenoma and H. pylori prevalence in non-Hispanic populations OR 1.66, 95% CI: 1.39-1.97 and OR 1.36, 95% CI: 1.10-1.68 (13,14). In addition to different genetic susceptibility or environmental factors, inconsistent and discrepancies maybe explained by small sample sizes, uncontrolled biases, differences in selection of controls and inadequate consideration of confounding in previously published data (15-20).
Per the Centers for disease control and prevention (CDC) data in 2010 (21), Blacks had the highest rate of colorectal cancer, followed by Whites, Hispanics, Asian/Pacific Islanders, and American Indian/Alaska Natives. Siegel et al. (22) reported that Hispanics had a lower risk of colorectal cancer when compared to Whites. Conflicting data exists on the association between race and colorectal adenomas. One retrospective analysis of 1,656 patients indicated a lower prevalence of colorectal adenomas in Hispanic versus non-Hispanic subjects (14.8% vs. 22.5%, P<0.01) (23). Conversely, an analysis of over 5,000 patients reported a higher prevalence of larger adenomas (>10 mm in size) in Hispanics; and the overall prevalence was not lower in Hispanics compared to White patients (24). The difference in the findings may be explained by the predominant South American ancestry versus the Dominican and Caribbean descent found in the later study. The Veterans Administration Colonoscopy Screening study found that African Americans had a higher risk of polyps larger than 9 mm (8%) in comparison to the White population (6%) (25). This difference was especially pronounced in African American women compared with White women.
Despite a high prevalence of H. pylori infection in our Hispanic population, there was no association between H. pylori and colonoscopic findings. One explanation could be confounding factors such as genetic differences that result in lower adenoma prevalence in Hispanics or perhaps no association at all. Additionally, discrepancies between studies may be the result of assay differences in the detection of H. pylori infection. Most studies reporting a positive association between H. pylori and colorectal adenomas and adenocarcinomas have utilized seroprevalence of H. pylori while our study utilized histologically proven H. pylori infection. Although there are genetic and environmental factors that may play a role in differing colorectal cancer etiologies in different races, further studies assessing the relationship between H. pylori infection and colonoscopic findings are needed. Biological details such as the specific strain of H. pylori infection may address the differences between studies.
In an analysis of 7,465 participants (National Health and Nutritional Examination Survey database), age-adjusted prevalence of H. pylori was found to be substantially higher among Hispanic Americans (61.6%) than non-Hispanic Blacks (52.7%) and non-Hispanic Whites (26.2%) (26). Despite the reported association of H. pylori and colorectal adenoma (13,14), and a higher prevalence of H. pylori in Hispanics the global prevalence of colorectal cancer in Hispanics compared to Whites and Blacks remains lower (22). This is comparable to our data where Hispanics had the highest prevalence around 40.9% compared to Blacks 29.1% then non-hispanic Whites 7.9%, and our adenoma detection rate was also lower in this group.
We found that the H. pylori positive population had a statistically lower prevalence of smoking compared to H. pylori negative population hinting towards a protective effect of smoking. While reports in the literature associate smoking with H. pylori infection, other studies have yielded an inverse relationship similar to our findings (26-31). In a Japanese study of 8,837 subjects (32), smoking was negatively associated with H. pylori infection. The risk of H. pylori seropositivity decreased linearly with cigarette consumption per day. A possible basis of smoking’s protective effect may be due to an increased smoking related gastric acidity which then protects against H. pylori.
Limitations of our study include the small sample size, and retrospective design. Furthermore, the ethnic diversity of the Hispanic population also limits generalizations. Most of our patients were South American; however this data was not available in medical records. Major strengths of our study included the selection of a diverse patient population sample. Additionally, our statistical analysis took into account multiple factors that could influence adenoma growth and detection, thus limiting confounders. Finally, we diagnosed H. pylori by biopsy, which is more accurate for diagnosing infection.
Conclusions
While previous literature has shown an association between H. pylori positive patients and colorectal adenomas, we did not find this in our Hispanic population. With the growing population of Hispanics in the U.S, large scale studies are needed to conclusively characterize the role of H. pylori infection in colorectal adenoma and adenocarcinoma. Our findings may be due to different environmental factors such as dietary/colonic flora, or genetic susceptibility. Our results support further investigation of these findings in Hispanics to further characterize the risk associated with H. pylori and colorectal adenoma in this population.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Unidentified curved bacilli on gastric epithelium in active chronic gastritis. Lancet 1983;1:1273-5. [PubMed]
- Barzilay EJ, Fagan RP. Helicobacter pylori. Available online: http://wwwnc.cdc.gov/travel/yellowbook/2014/chapter-3-infectious-diseases-related-to-travel/helicobacter-pylori
- Everhart JE, Kruszon-Moran D, Perez-Perez GI, et al. Seroprevalence and ethnic differences in Helicobacter pylori infection among adults in the United States. J Infect Dis 2000;181:1359-63. [PubMed]
- Rothenbacher D, Brenner H. Burden of Helicobacter pylori and H. pylori-related diseases in developed countries: recent developments and future implications. Microbes Infect 2003;5:693-703. [PubMed]
- Meucci G, Tatarella M, Vecchi M, et al. High prevalence of Helicobacter pylori infection in patients with colonic adenomas and carcinomas. J Clin Gastroenterol 1997;25:605-7. [PubMed]
- Breuer-Katschinski B, Nemes K, Marr A, et al. Helicobacter pylori and the risk of colonic adenomas. Colorectal Adenoma Study Group. Digestion 1999;60:210-5. [PubMed]
- Limburg PJ, Stolzenberg-Solomon RZ, Colbert LH, et al. Helicobacter pylori seropositivity and colorectal cancer risk: a prospective study of male smokers. Cancer Epidemiol Biomarkers Prev 2002;11:1095-9. [PubMed]
- Hartwich A, Konturek SJ, Pierzchalski P, et al. Helicobacter pylori infection, gastrin, cyclooxygenase-2, and apoptosis in colorectal cancer. Int J Colorectal Dis 2001;16:202-10. [PubMed]
- Grahn N, Hmani-Aifa M, Fransén K, et al. Molecular identification of Helicobacter DNA present in human colorectal adenocarcinomas by 16S rDNA PCR amplification and pyrosequencing analysis. J Med Microbiol 2005;54:1031-5. [PubMed]
- Hamid HK, Mustafa YM. The Role of Infectious Agents in Colorectal Carcinogenesis. In: Ettarh R. eds. Colorectal Cancer Biology- From Genes to Tumor. Rijeka: InTech, 2012:341-74.
- Renga M, Brandi G, Paganelli GM, et al. Rectal cell proliferation and colon cancer risk in patients with hypergastrinaemia. Gut 1997;41:330-2. [PubMed]
- ASGE Standards of Practice Committee, Early DS, Ben-Menachem T, et al. Appropriate use of GI endoscopy. Gastrointest Endosc 2012;75:1127-31. [PubMed]
- Hong SN, Lee SM, Kim JH, et al. Helicobacter pylori infection increases the risk of colorectal adenomas: cross-sectional study and meta-analysis. Dig Dis Sci 2012;57:2184-94. [PubMed]
- Wu Q, Yang ZP, Xu P, et al. Association between Helicobacter pylori infection and the risk of colorectal neoplasia: a systematic review and meta-analysis. Colorectal Dis 2013;15:e352-64. [PubMed]
- Moss SF, Neugut AI, Garbowski GC, et al. Helicobacter pylori seroprevalence and colorectal neoplasia: evidence against an association. J Natl Cancer Inst 1995;87:762-3. [PubMed]
- Thorburn CM, Friedman GD, Dickinson CJ, et al. Gastrin and colorectal cancer: a prospective study. Gastroenterology 1998;115:275-80. [PubMed]
- Fireman Z, Trost L, Kopelman Y, et al. Helicobacter pylori: seroprevalence and colorectal cancer. Isr Med Assoc J 2000;2:6-9. [PubMed]
- Shmuely H, Passaro D, Figer A, et al. Relationship between Helicobacter pylori CagA status and colorectal cancer. Am J Gastroenterol 2001;96:3406-10. [PubMed]
- Siddheshwar RK, Muhammad KB, Gray JC, et al. Seroprevalence of Helicobacter pylori in patients with colorectal polyps and colorectal carcinoma. Am J Gastroenterol 2001;96:84-8. [PubMed]
- Henley SJ, Singh S, King J, et al. Invasive cancer incidence - United States, 2010. MMWR Morb Mortal Wkly Rep 2014;63:253-9. [PubMed]
- Lieberman DA, Weiss DG, Bond JH, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. Veterans Affairs Cooperative Study Group 380. N Engl J Med 2000;343:162-8. [PubMed]
- Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin 2012;62:10-29. [PubMed]
- Zheng XE, Li T, Lipka S, et al. Location-dependent ethnic differences in the risk of colorectal adenoma: a retrospective multiethnic study. J Clin Gastroenterol 2014;48:e1-7. [PubMed]
- Lebwohl B, Capiak K, Neugut AI, et al. Risk of colorectal adenomas and advanced neoplasia in Hispanic, black and white patients undergoing screening colonoscopy. Aliment Pharmacol Ther 2012;35:1467-73. [PubMed]
- Dimou A, Syrigos KN, Saif MW. Disparities in colorectal cancer in African-Americans vs Whites: before and after diagnosis. World J Gastroenterol 2009;15:3734-43. [PubMed]
- Kanbay M, Gür G, Arslan H, et al. The relationship of ABO blood group, age, gender, smoking, and Helicobacter pylori infection. Dig Dis Sci 2005;50:1214-7. [PubMed]
- Özden A. Helicobacter pylori 2006. Güncel Gastroenteroloji 2006;10:287-91.
- Braverman DZ, Rudensky B, Dollberg L, et al. Campylobacter pylori in Israel: prospective study of prevalence and epidemiology. Isr J Med Sci 1990;26:434-8. [PubMed]
- Graham DY, Malaty HM, Evans DG, et al. Epidemiology of Helicobacter pylori in an asymptomatic population in the United States. Effect of age, race, and socioeconomic status. Gastroenterology 1991;100:1495-501. [PubMed]
- Bateson MC. Cigarette smoking and Helicobacter pylori infection. Postgrad Med J 1993;69:41-4. [PubMed]
- Fontham ET, Ruiz B, Perez A, et al. Determinants of Helicobacter pylori infection and chronic gastritis. Am J Gastroenterol 1995;90:1094-101. [PubMed]
- Ogihara A, Kikuchi S, Hasegawa A, et al. Relationship between Helicobacter pylori infection and smoking and drinking habits. J Gastroenterol Hepatol 2000;15:271-6. [PubMed]


