Advanced metastatic gastric adenocarcinoma identified within the placenta: a case report with literature review
Introduction
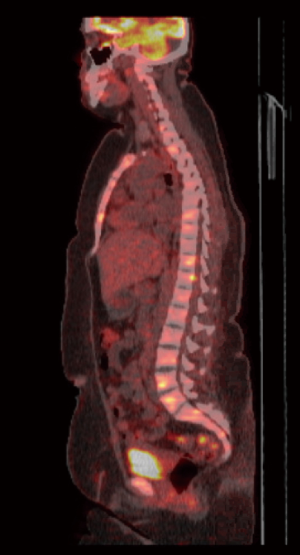
A 32-year-old woman, gravida 5, para 4 presented in her 35th week of gestation for evaluation of back pain. Prior to this visit, her pregnancy was uneventful. The patient’s medical history and family history was unremarkable. Labs were significant for alkaline phosphatase (ALP) 251 U/L, total bilirubin (T-bili) 1.2 mg/dL, lactate dehydrogenase (LDH) 728 U/L, uric acid 8.4 mg/dL, fibrinogen 157 mg/dL, international normalized ratio (INR) 1.5, prothrombin time (PT) 17.8 s, partial thromboplastin time (PTT) 35.8 s, platelet count (PLT) 33 K/µL, reticulocyte count 2.4% with peripheral smear significant for normochromic normocytic red blood cells without schistocytes, and no laboratory evidence of ADAMSTS-13 deficiency. Her labs were concerning for disseminated intravascular coagulation (DIC)/hemolysis, elevated liver enzymes and low platelet count (HELLP) syndrome, prompting an urgent cesarean section. The placenta was sent for pathological examination as part of the evaluation of this high-risk pregnancy. Cross section of the placental disk showed areas with intervillous and sub-chorionic fibrin deposition. In addition, scattered clusters of tumor cells were present within the intervillous spaces. The tumor cells had large somewhat eccentrically placed nuclei, irregular nuclear contours, and prominent nucleoli. The tumor appeared confined to the intervillous spaces, and no villous stromal invasion by tumor was seen (Figure 1A,B). A panel of immunohistochemical stains was positive for Ber-Ep4, cytokeratin 7 and MUC5AC, confirming a diagnosis of metastatic carcinoma. Computed tomography (CT) of the patient’s chest, abdomen, and pelvis with intravenous (IV) contrast reported a prominent nodular thickening of the anterior gastric body and antrum suggesting a mass (Figure 2). Magnetic resonance imaging (MRI) of the patient’s brain showed no evidence of metastasis. An MRI of her L-spine was significant for diffuse marrow signal changes compatible with hematopoietic bone marrow. The patient subsequently underwent esophagogastroduodenoscopy (EGD) revealing a large, fungating and ulcerated, non-circumferential mass in the gastric antrum. A biopsy of the EGD mass showed similar histological features and demonstrated an infiltrate of malignant signet ring type cells in the lamina propria. Tumor DNA sequencing showed KRAS, NRAS, BRAF, EGFR, HER2neu negative, with low mutation burden and microsatellite stable. A positron emission tomography-CT (PET-CT) scan found a hypermetabolic gastric antral lesion with extensive hypermetabolic lymphadenopathy in the periportal, retroperitoneal para-aortic, inferior mediastinal and left supraclavicular regions (Figure 3) along with diffusely increased bone marrow activity throughout the pelvis, vertebral bodies, and sternum (Figure 4).


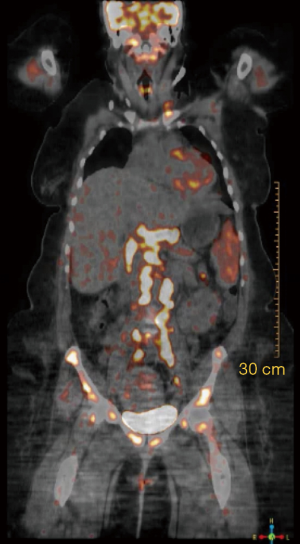
The patient was started on palliative FOLFOX as an inpatient. At times, treatment was delayed due to side effects and decreased quality of life affecting the patient’s ability to take care of her children. Four months later, a repeat PET scan showed residual wall thickening in the antral region of the stomach with almost complete interval resolution of the previously reported extensive metastatic lymphadenopathy in the abdomen, inferior mediastinum, and left supraclavicular regions. However, there was new, extensive ostial metastatic involvement in the thoracic and lumbar vertebrae, sternum, bilateral ribs, bilateral scapula, pelvis, and bilateral femur. There was also a prominent focus in the left posterior aspect of T11 vertebral body projecting into the adjacent spinal cord (Figure 5). The patient had no signs or symptoms of compression or spinal cord involvement but had considerable pain near the T11 vertebral region.
Two months later, the patient was readmitted with severe back pain, weakness of bilateral legs, and numbness of the left cheek extending to the gums and left lower eyelid (V2 distribution).
An MRI of her spine revealed infiltrates throughout the cervical, thoracic, and lumbar spine. An MRI of her brain showed no masses; however, a new pachymeningeal (dura-arachnoid) enhancement was seen. The patient underwent a lumbar puncture (LP) study, which was interpreted as having few atypical cells, highly suspicious for metastatic adenocarcinoma. The patient was diagnosed with malignant carcinomatosis meningitis and started on with palliative radiation to the spine and intrathecal methotrexate. Her disease progressed rapidly, and she was placed on hospice with pain management. Approximately 7 months following diagnosis, she expired. A follow-up exam of the newborn at 9 months found no evidence of metastasis.
Discussion
Gastric cancer is one of the deadliest diseases and frequently offers a poor prognosis. With only 31.0% of cases surviving 5 years. Based on 2011–2015 cases, the number of new cases of stomach cancers per year was 7.2 per 100,000 men and women. Based on 2013–2015 data, approximately 0.8% of men and women will be diagnosed with stomach cancer. In 2018, there were 26,240 estimated new cases; 1.5% of all new cancer cases (1).
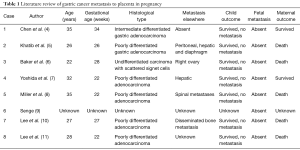
The coexistence of gastric carcinoma with pregnancy is rare; depending on the region of the world it accounts for anywhere between 0.026% to 0.1% of all pregnancies (2). Placental metastasis from maternal cancer is even rarer. Our search showed since Friedreich reported the first case of carcinoma metastasized to the fetus in 1866 (3) there have been only 36 reported cases of gastric cancer metastasis. Furthermore, the worldwide literature notes only 8 reported cases (see Table 1) of metastatic gastric cancer to a placenta. To our knowledge, in addition to placental metastasis, not a single reported case included metastasis to bone and leptomeninges, as in our case. Making this the first case of placental metastatic disease with a complex metastatic presentation involving extensive bone marrow involvement and leptomeningeal disease.
Full table
Gastric cancer associated with pregnancy is generally discovered at an advanced stage and consequently has a dismal prognosis. The poor prognosis of gastric cancer during pregnancy is derived from its rarity and delayed diagnoses secondary to symptoms interpreted as a part of normal physiological gestational symptoms, such as nausea, vomiting or abdominal pain or cramping (12). Of 92 cases of gastric cancer reviewed by Jaspers et al. (13), only two cases were found to be diagnosed early stage. Rapid progression and later diagnosis lead to a poor prognosis for these women, with 88.0% of patients expiring from the disease within 1 year.
Further, summarizing a total of 61 Japanese gastric cancer cases during pregnancy, Ueo et al. (14) reported about 97% of patients were at an advanced stage with a 21.1% 3-year survival rate. Based on their experience and review of the literature, the authors concluded that the poor prognosis for gastric cancer during pregnancy is a result of the favorable environment for the disease caused by estrogen surges, the immunosuppressive effect of pregnancy, limited therapeutic approaches, and the likelihood of delayed diagnosis.
In the present case, the patient was not known to have any prior malignancies and fetal development was progressing normally. The patient developed HELLP/DIC; therefore, we prioritized the mother’s survival and elected for a cesarean section. Our patient’s gastric mass biopsy indicated advanced-stage adenocarcinoma with signet ring cells that were not amiable to surgical intervention. However, for cases when gastric cancer is diagnosed early, it would usually be preferable to perform endoscopic surgery and continue the pregnancy for as long as possible.
The most common metastatic sites for gastric carcinoma are peritoneal surfaces, the liver, spleen, ovaries, lung, and brain. Gastric cancer infrequently metastasizes to the bone. This report describes an extremely rare case of progressive osseous metastasis. In comparison to other solid tumors, ostial metastasis in gastric cancer patients has been shown to exhibit poor prognosis, with a mean survival time of <5 months (15,16). Patients often suffer from extensive bone pain affecting the quality of life. Due to the extensive capillary network in the gastric mucosa and lack of lymphatic vessels in the bone marrow, the metastatic pathway of gastric cancer cells is generally hematogenous (17). High proliferation in bone marrow, causes disseminated carcinomatosis a majority of the time, as in our case. Cases of bone marrow metastatic spread occur most commonly with signet ring cell type or undifferentiated type. In a study by Ahn et al. (18), it was found that 19 of 2,150 patients with gastric carcinoma expressed metastasis to the bone (0.9%). All these cases suggest a relationship between poor differentiation and signet-ring type carcinoma and unusual locations for metastasis (18).
Leptomeningeal involvement is also very unusual and is considered a devastating outcome of gastric cancer. Our patient had a radiological abnormality of her pachymeningeal (dura-arachnoid) and cytological evidence of malignancy in the cerebrospinal fluid. Leptomeningeal carcinomatosis (LC) presents in approximately 2% to 4% of all patients with cancer, but its incidence is much lower in gastric carcinoma (19). Based on Vergoulidou’s literature review, LC is associated with incredibly poor prognosis and because of its rarity, there are limited treatment modalities. Leptomeningeal involvement often results in rapid deterioration refractory to conventional and intrathecal chemotherapy.
Fortunately, the patient’s newborn did not have any evidence of metastasis likely due to biological protective mechanisms. Maternal and fetal circulation are separated by the syncytiotrophoblasts (outer layer), the cytotrophoblasts (inner layer) that line the villous projections and the capillary wall. Maternal blood circulation in the placenta drains into the intervillous space, where the anchoring villous projections are located. Wang et al. (20), examined morphological changes of the placenta from a case of maternal acute lymphatic leukemia concluding that syncytium could play a role as a physical barrier in the prevention of vertical transplacental metastasis by phagocytosis and destruction of tumor cells. Want et al., made this conclusion based on discovering phagocytosis of nucleus-containing cells by the syncytiotrophoblast, cells with an abundant number of microtubular bundles within the villous stroma and dilatation of syncytial rough endoplasmic reticulum, numerous syncytial knots, and numerous autophagosomes.
In addition to trophoblasts, another defense mechanism may exist in the placenta to inhibit fetal metastasis. Literature has proposed that a primitive connective tissue, Wharton’s Jelly, laying between the amniotic epithelium and the umbilical vessels has been found to have human umbilical cord mesenchymal stem cells (hUCMSCs). (21) These cells are characterized by their self-renewal and multipotency. In in vitro and in vivo hUCMSC have proved to suppress tumorigenesis. The underlying mechanism is likely related to cell cycle arrest, stimulation of tumor cell apoptosis, and suppressed activities of protein kinases (22).
In conclusion, gastric carcinogenesis is a multistep and multifactorial process. While gastric cancer remains a deadly disease, the discoveries of new molecular markers, genetic and epigenetic alterations, and novel pharmacogenetic traits have facilitated improvement in patient care, fostered hope, and paved new directions. Thus, the potential for gastric carcinoma in pregnancy should not be ignored, particularly in females presenting with atypical digestive symptoms in later trimesters. Patients need early intervention to improve prognosis. We recommend a low threshold for screening.
Acknowledgments
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from the patients next of kin for publication of this case report and any accompanying images.
References
- Cancer of the Stomach - Cancer Stat Facts. Available online: https://seer.cancer.gov/statfacts/html/stomach.html
- Sakamoto K, Kanda T, Ohashi M, et al. Management of patients with pregnancy-associated gastric cancer in Japan: a mini-review. Int J Clin Oncol 2009;14:392-6. [Crossref] [PubMed]
- Friedreich N. Beitrage zur pathologic des krebses. Virchows Arch Path Anat 1866;36:30. [Crossref]
- Chen Y, Li Y, Wang H, et al. Maternal gastric carcinoma with metastasis to the placenta: A case report. Oncol Lett 2014;8:2509-10. [Crossref] [PubMed]
- Khatib F, Shaya M, Samueloff A. Gastric carcinoma with metastasis to the placenta and amniotic fluid: case report and review of the literature. Eur J Obstet Gynecol Reprod Biol 2003;107:208-9. [Crossref] [PubMed]
- Baker AM, Haeri S, Shafer A, et al. Maternal gastric carcinoma metastatic to the placenta. Eur J Obstet Gynecol Reprod Biol 2010;153:225-6. [Crossref] [PubMed]
- Yoshida M, Matsuda H, Furuya K. Successful treatment of gastric cancer in pregnancy. Taiwan J Obstet Gynecol 2009;48:282-5. [Crossref] [PubMed]
- Miller K, Zawislak A, Gannon C, et al. Maternal gastric adenocarcinoma with placental metastases: what is the fetal risk? Pediatr Dev Pathol 2012;15:237-9. [Crossref] [PubMed]
- Senge J. Beitr Path Anatom. 1912;53:532.
- Lee M, Kim S, Lee J. A case of placental metastasis from advanced gastric carcinoma. J Korean Cancer Assoc 1998;30:608-12.
- Lee H, Kim Y, Kim C. Placental metastasis of maternal gastric adenocarcinoma: a case report. Korean J Pathol 1999;33:214-6.
- Samuels P. Medical complications. In: Gabbe SG, Niebyl JR, Simpson JL. editors. Obstetrics: Normal and Problem Pregnancies. 7th ed. New York: Churchill Livingstone, 1986:931-2.
- Jaspers VK, Gillessen A, Quakernack K. Gastric cancer in pregnancy: do pregnancy, age or female sex alter the prognosis? Case reports and review. Eur J Obstet Gynecol Reprod Biol 1999;87:13-22. [Crossref] [PubMed]
- Ueo H, Matsuoka H, Tamura S, et al. Prognosis in gastric cancer associated with pregnancy. World J Surg 1991;15:293-7, discussion 298. [Crossref] [PubMed]
- Crivellari D, Carbone A, Sigon R, et al. Gastric cancer with bone marrow invasion at presentation: case-report and review of the literature. Tumori 1995;81:74-6. [Crossref] [PubMed]
- Hussain S, Chui S. Gastric carcinoma presenting with extensive bone metastases and marrow infiltration causing extradural spinal haemorrhage. Br J Radiol 2006;79:261-3. [Crossref] [PubMed]
- Kobayashi M, Okabayashi T, Sano T, et al. Metastatic bone cancer as a recurrence of early gastric cancer -- characteristics and possible mechanisms. World J Gastroenterol 2005;11:5587-91. [PubMed]
- Ahn JB, Ha TK, Kwon SJ. Bone metastasis in gastric cancer patients. J Gastric Cancer 2011;11:38-45. [Crossref] [PubMed]
- Vergoulidou M. Leptomeningeal Carcinomatosis in Gastric Cancer: A Therapeutical Challenge. Biomark Insights 2017;12:1177271917695237. [Crossref] [PubMed]
- Wang T, Hamann W, Hartge R. Structural aspects of a placenta from a case of maternal acute lymphatic leukaemia. Placenta 1983;4:185-95. [Crossref] [PubMed]
- Wang HS, Hung SC, Peng ST, et al. Mesenchymal stem cells in the Wharton's jelly of the human umbilical cord. Stem Cells 2004;22:1330-7. [Crossref] [PubMed]
- Ma Y, Hao X, Zhang S, et al. The in vitro and in vivo effects of human umbilical cord mesenchymal stem cells on the growth of breast cancer cells. Breast Cancer Res Treat 2012;133:473-85. [Crossref] [PubMed]