Radiotherapy versus stenting in treating malignant dysphagia
Introduction
Esophageal cancer is diagnosed in about 400,000 patients each year worldwide, and its incidence is increasing (1), it is the sixth leading cause of death from cancer (2). In Europe, while incidence of SCC has remained stable or declined during the past few decades, the incidence of esophageal adenocarcinoma has been rising. This increase has been more prominent in Northern Europe, notably in the United Kingdom and Ireland (3,4).
The majority of the patients suffering from a cancer of the esophagus presents with symptoms of dysphagia and weight loss because of an obstructive tumor (5).
Several management options have been developed to palliate malignant dysphagia. These include endoluminal stenting or surgery and external beam radiation, brachytherapy, chemotherapy, chemoradiotherapy, laser treatment, photodynamic therapy or ablation using injection of alcohol or chemotherapeutic agents (6-8).
Placement of self-expanding metallic stents (SEMS) made up of an alloy, usually nitinol or stainless steel, and deployed using endoscopic or fluoroscopic techniques, is a newer method for relief of dysphagia in these patients (9).
External beam radiotherapy (EBRT) is known to provide durable and effective relief of dysphagia. However, there is a time lag before symptomatic relief occurs, and up to 6 weeks are required for maximum benefit (8).
Survival advantage of combined stenting and radiotherapy was first suggested by Ogilvie et al. (10), other studies (11,12) have also investigated the effect of combined stenting and radiotherapy on survival of patients with advanced esophageal cancer and reported superior results with regard to both relief of dysphagia and survival for stenting followed by radiotherapy in those patients.
In view of promising results of stenting and radiotherapy, we conducted this study to compare stenting alone and radiotherapy with or without stenting in patients of locally advanced cancer esophagus regarding overall survival.
Patients and methods
This is a prospective data of ninety-one patients with locally advanced or metastatic esophageal cancer who were treated at Northamptonshire Oncology Centre from 1/1/1999 till 1/1/2007.
Eligibility criteria included patients with locally advanced or metastatic (T3, T4, any N, any M) previously untreated cancer esophagus with Eastern Cooperative Oncology Group (ECCOG) performance status ≤3, age greater than 18 years, adequate bone marrow function, renal and hepatic functions. Patients are not eligible to any radical treatment. Patients included in this study were divided into three groups, group I (GI) 30 Patients received radiotherapy only, 35 patients underwent stenting only (GII) and 26 patients underwent radiotherapy followed by stenting (GIII).
Pretreatment and follow-up evaluation
Pretreatment evaluation included a detailed history taking, physical examination, and routine laboratory examinations.
All patients underwent a baseline CT of the neck, chest and abdomen examination, upper gastrointestinal endoscopy and biopsy. Barium swallow and endoscopic ultrasound were only done in some patients. These studies were only repeated as and when necessary (e.g., if the patient is having palliative chemotherapy).
Treatment
Radiotherapy
Patients were treated by 2 D conventional EBR, which was delivered with linear accelerator 6 MV energy, conventional simulation planning two parallel opposing filed was used, the target volume included the initial lesion with a margin of 3 to 5 cm at both proximal and distal ends of the esophagus. The total radiation dose ranged from 20 Gy in 5 fractions over one week to 30 Gy in 10 fractions over two weeks.
Stenting
The stent of proper length was selected, placed and released along the site of stenosis by endoesophageal stent introducer. Stent should extend about 2 cm proximal and distal to the tumor. After placement, patients were advised to drink adequate warm water, making the stent expand properly. One week after examination was carried out through upper digestive tract fluoroscopy with barium.
Radiotherapy and stent
EBRT was used first and after progression of their dysphagia patients were offered stent placement, radiotherapy dose ranged from 20 Gy in 5 fractions to 30 Gy in 10 fractions. Only two patients received 40 Gy in 20 fractions over 4 weeks.
Statistical methods
The study endpoint was overall survival and it was calculated from the day of the start of treatment to the day of death or of lost follow-up.
The data were coded and entered into a computer using Statistical Package for Social Sciences (SPSS) version 15.0. Results were expressed as number, percentiles and medians. Categorical variables were compared using chi-square tests. Survival functions (OAS) were estimated using Kaplan Meier test, comparison between survival curves was achieved by the Log Rank test.
P-value of <0.05 taken to indicate statistical significance.
Results
Patient’s characteristics
The characteristics of the 91 patients of groups I, II and III are shown in Table 1. The three patient groups were balanced; the most common pathological type was squmous cell carcinoma 60% in GI, 48.6% in GII and 53.8% in GIII, followed by adenocarcinoma, all patients had dysphagia, 14.3% had metastasis and the most common sites of metastasis were lung and liver.
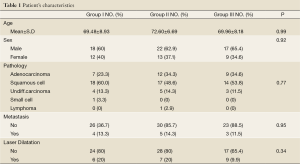
Full table
There was no significance difference between the median radiation dose given for GI and GIII, it was 24.66 and 26.29 in G1and GIII respectively, stent migration occurred in 3 patients of GII and in 1 patient of GIII. All patients underwent stent had complications included transient chest pain after stent placement and gastroesophageal reflux.
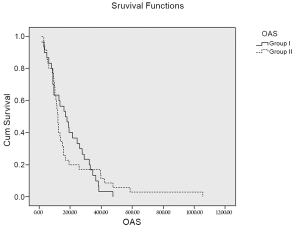
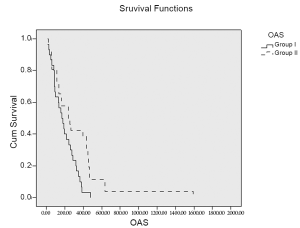
The median overall survival (OAS) was 169 days (95% CI, 96.53-241.46) in GI, 119 days (95% CI, 106.48-131.51) in GII and 237 days (95% CI, 107.07-366.92) in GIII. The difference between GI &II was statistically insignificant (P=0.86) while the difference between GI &III was significant (P=0.01) (Figures 1,2).
Discussion
Esophageal cancer is increasing in last few years, unfortunately the majority of patients will present with locally advanced or metastatic disease which is difficult to control. Considering this fact, it is important to offer treatment providing adequate and rapid palliation of symptoms especially the obstructive symptoms which reflect on the quality of life. Radiotherapy for esophageal cancer is a relatively effective treatment and provides survival benefits.
In the present study 91 patients enrolled 30 patients received radiotherapy, 35 patients underwent stent and 26 patients underwent stent and received radiotherapy, relief of dysphagia occurs rapidly in stent groups than in radiotherapy alone group (8) and was more standing in stent plus radiotherapy group, recurrence of dysphagia occurs in 8.5% in GII and 3.8% in GIII this is due to tumor over growth on the stent in GII.
The median overall survival time was 169 days for patients receiving radiotherapy and this comparable to reported by Slabber et al. (13), who reported 144 days median over all survival, the median radiation dose was 24.66±5.07 in GI and 26.29±6.17 GIII, doses more than 40 Gy increase toxicity. Median overall survival for stent only patients was 119 days and this results similar to that reported by Homs et al. (14), and Conio et al. (15), however, Han et al. (12) reported 312 days median overall survival in stent alone patients. The present study shows survival benefits for addition of radiotherapy to stent patients of locally advanced disease, its median overall survival time was 237d days, Han et al. (12)reported 499 days, while Song et al. (16) reported 161 days, this advantage may be due to tumor local control by radiotherapy. Yu et al. in a their trail of offering radiotherapy 4-7 days after stent replacement has reported mean survival of 510 days but this was a very small series (17).
In the future, it can be expected that removable stents will be used as a bridge to surgery or radiotherapy to maintain luminal patency during neoadjuvant treatment. However it is difficult to assess the survival benefit in these approaches for each treatment modalities as some patients underwent surgery or radical chemoradiotherapy thereafter (18,19).
It is very likely that the survival benefit in group III were due to selection bias as this study was not intended to be a randomized trial. Also patients who offered stent as first step were those who are having Grade III or more dysphgaia and their survival is expected to be limited. The role of combined EBRT and stent as opposed to either alone is a relevant area of investigation and a randomized phase III study of SEMS +/- EBRT is due to open shortly in the UK (ROCS).
In conclusion, combinations of stent and RT may provide survival benefit in patients with malignant dysphagia. A randomized clinical trial is recommended.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Siersema PD. Esophageal cancer. Gastroenterol Clin North Am 2008;37:943-64. [PubMed]
- Falk J, Carstens H, Lundell L, et al. Incidence of carcinoma of the oesophagus and gastric cardia. Changes over time and geographical differences. Acta Oncol 2007;46:1070-4. [PubMed]
- Karim-Kos HE, de Vries E, Soerjomataram I, et al. Recent trends of cancer in Europe: a combined approach of incidence, survival and mortality for 17 cancer sites since the 1990s. Eur J Cancer 2008;44:1345-89. [PubMed]
- Steevens J, Botterweck AA, Dirx MJ, et al. Trends in incidence of oesophageal and stomach cancer subtypes in Europe. Eur J Gastroenterol Hepatol 2010;22:669-78. [PubMed]
- Watt E, Whyte F. The experience of dysphagia and its effect on the quality of life of patients with oesophageal cancer. Eur J Cancer Care (Engl) 2003;12:183-93. [PubMed]
- Weigel TL, Frumiento C, Gaumintz E. Endoluminal palliation for dysphagia secondary to esophageal carcinoma. Surg Clin North Am 2002;82:747-61. [PubMed]
- Allum WH, Griffin SM, Watson A, et al. Guidelines for the management of oesophageal and gastric cancer. Gut 2002;50:v1-23. [PubMed]
- Bown SG. Palliation of malignant dysphagia: surgery, radiotherapy, laser, intubation alone or in combination? Gut 1991;32:841-4. [PubMed]
- O’Donnell CA, Fullarton GM, Watt E, et al. Randomized clinical trial comparing self-expanding metallic stents with plastic endoprostheses in the palliation of oesophageal cancer. Br J Surg 2002;89:985-92. [PubMed]
- Ogilvie AL, Dronfield MW, Ferguson R, et al. Palliative intubation of oesophagogastric neoplasms at fibreoptic endoscopy. Gut 1982;23:1060-7. [PubMed]
- Zhong J, Wu Y, Xu Z, et al. Treatment of medium and late stage esophageal carcinoma with combined endoscopic metal stenting and radiotherapy. Chin Med J (Engl) 2003;116:24-8. [PubMed]
- Han YT, Peng L, Fang Q, et al. Value of radiotherapy and chemotherapy after SEMS implantation operation in patients with malignant esophageal stricture. Ai Zheng 2004;23:682-4. [PubMed]
- Slabber CF, Nel JS, Schoeman L, et al. A randomized study of radiotherapy alone versus radiotherapy plus 5-fluorouracil and platinum in patients with inoperable, locally advanced squamous cancer of the esophagus. Am J Clin Oncol 1998;21:462-5. [PubMed]
- Homs MY, Steyerberg EW, Eijkenboom WM, et al. Single-dose brachytherapy versus metal stent placement for the palliation of dysphagia from oesophageal cancer: multicentre randomised trial. Lancet 2004;364:1497-504. [PubMed]
- Conio M, Repici A, Battaglia G, et al. A randomized prospective comparison of self-expandable plastic stents and partially covered self-expandable metal stents in the palliation of malignant esophageal dysphagia. Am J Gastroenterol 2007;102:2667-77. [PubMed]
- Song HY, Lee DH, Seo TS, et al. Retrievable covered nitinol stents: experiences in 108 patients with malignant esophageal strictures. J Vasc Interv Radiol 2002;13:285-93. [PubMed]
- Yu YT, Yang G, Liu Y, et al. Clinical evaluation of radiotherapy for advanced esophageal cancer after metallic stent placement. World J Gastroenterol 2004;10:2145-6. [PubMed]
- Hirdes MM, Vleggaar FP, Siersema PD. Stent placement for esophageal strictures: an update. Expert Rev Med Devices 2011;8:733-55. [PubMed]
- Langer FB, Schoppmann SF, Prager G, et al. Temporary placement of self-expanding oesophageal stents as bridging for neo-adjuvant therapy. Ann Surg Oncol 2010;17:470-5. [PubMed]