The localisation of cancer in the sigmoid, rectum or rectosigmoid junction using endoscopy or radiology—What is the most accurate method?
Introduction
Colorectal cancer is one of the most prevalent malignancies in the Western world (1,2). Surgery is the only curative option. In case of lymph node metastases, adjuvant chemotherapy is applied in order to increase the disease free survival and the five-year survival rate (3-5). In case of rectal cancer neo-adjuvant radiation therapy is often applied. In addition, if pathological lymph nodes and/or an involved meso-rectal fascia are present neo-adjuvant chemo-radiation is recommended (6,7). These differences in therapeutic approach between colon cancer and rectal cancer are important in cases of a cancer in the distal part of the sigmoid or proximal in the rectum. Pre-operative staging with CT-scan and/or MRI is used to differentiate between rectal cancer and cancer located in the sigmoid. Endoscopic anatomical localisation is also mentioned. In daily practice, with multi-disciplinary meetings on colorectal cancer, there is often discussion about the exact localisation. The radiological localisation is usually preferred and the endoscopic localisation of the tumour is not considered to be decisive.
For this reason a clinical study was done in consecutive patients, in whom rectal cancer or cancer in the sigmoid was diagnosed endoscopically, in order to evaluate the best method of localisation: colonoscopy or radiological imaging. The histological examination of the resected specimen was used as the gold standard for the definite localisation.
Materials and methods
All consecutive patients in a period of three years (2010, 2011, and 2012) in whom cancer in the sigmoid or rectum was diagnosed endoscopically were included.
The procedure was done because of the usual routine clinical indications, such as rectal bleeding, anaemia, bowel complaints etc. Colonoscopy was done after standard colon cleansing using Olympus or Fujinon video-endoscopes.
The distance of the tumour from the anal verge is routinely measured during retrieval of the endoscope. After taking biopsy specimens to confirm the macroscopic diagnosis, the tumour mostly was marked with an ink tattoo in order to enhance visibility during laparoscopic surgery. In daily practice, the endoscopist measures the distance from the anal verge and, depending on the number of folds between the tumour and the anal canal, defines the tumour either rectal or sigmoidal. In addition, rectal cancer is defined as a tumour located within reach of proper digital examination of the rectum.
After endoscopy patients underwent additional radiological examinations (CT-scan of the abdomen and MRI of the pelvic region) in order to stage the tumour.
Inclusion criterion for the present study was the availability of a resection specimen. Hence, only patients undergoing surgery were included in the analysis. Histological examination of the resected specimens served as gold standard for determining the definite anatomical localisation. Although a tumour diagnosed by digital rectal examination was considered rectal cancer, these tumours only were included in case of presence of a resection specimen.
If the tumour was surrounded by serosa than the cancer was definitely a sigmoid cancer. If the tumour was surrounded by perirectal fat with absence of a serosal surface, than it was rectal cancer. Finally, if the frontal edge of the tumour showed serosa and the dorsal plane perirectal fat than the tumour was located in the “rectosigmoid”, or the pelvic part of the rectum.
Statistical analysis was done with chi-square test for contingency tables and t-test. A P value below 0.05 was considered statistical significant.
Results
In the three year period 182 cancers in rectum and sigmoid were diagnosed by colonoscopy. Of eight patients (four rectal cancers and four cancers in the sigmoid) no further data was available because they were treated elsewhere. Twenty three patients with a tumour in the sigmoid had distant metastases at initial presentation. They did not undergo surgery, and were excluded from analysis. Fifteen patients with a rectal cancer had distant metastases, 6 did not undergo surgery because of co-morbidity rendering surgery to dangerous. In one case the tumour in the rectum appeared to be a squamous cell carcinoma originating from the cervix, and one patient had cancer in a rectal polyp which was removed radically via polypectomy.
Thus 128 surgical specimens were available for evaluation.
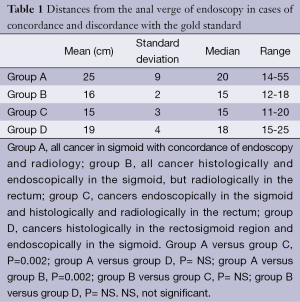
Fifty eight patients (39 men, 19 women) with a sigmoid cancer, according to endoscopic localisation, underwent surgical resection. Histological examination of the resection specimen revealed a cancer completely surrounded by serosa, hence definitely located in the sigmoid. In 43 cases the CT-scan located the tumour correctly in the sigmoid, in two cases only a pre-operative ultrasound was done with localisation in the sigmoid, in ten cases the CT-scan located the tumour in the rectum or rectosigmoid, in two cases the tumour was too small to be visualised by radiological examination, and, in one case CT-scan located the tumour in the descending colon. In the ten cases of faulty radiological results the tumour was endoscopically significantly closer to the anal verge compared with the 48 patients with clear sigmoidal localisation, mean distance 15.8 cm (SD 1.93) versus 25.3 (8.9) P=0.002 (Table 1).
Full table
Rectal cancer was diagnosed endoscopically in 82 patients (57 men, 25 women). Of these 54 underwent radiation or chemoradiation followed by surgery. In 53 cases MRI and/or CT-scan localised the tumour in the rectum, only in one case it was located in the sigmoid.
In 16 patients (10 men, 6 women) the tumour was located in the sigmoid endoscopically but after surgery, according to histology, the tumour was located clearly in the rectum in ten cases and in the rectosigmoid in six cases. These tumours were correctly situated in the rectum or rectosigmoid with MRI of the pelvis. The mean endoscopic distance to the anal verge was 15.2 cm (SD 3) in case of the rectal cancer and 18.5 cm (3.7) in case of a rectosigmoidal localisation (Table 1).
Of the 128 cancers with gold standard, endoscopy had the correct localisation in 112 (87.5%), and radiology in 114 (90.5%) cases. Concordance between both techniques was present in 80% of the cases. In 28 cases there was discordance. Ten sigmoidal cancers were located wrongly in the rectum, and one in the descending colon, with CT-scan and or MRI. One rectal cancer was placed in the sigmoid. In 16 cases the endoscopic localisation wrongly was the sigmoid.
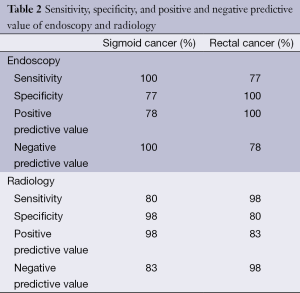
In Table 2 the results of sensitivity, specificity, and positive and negative predictive value noted.
Full table
Discussion
From daily practice it is a well-known fact that endoscopic localisation of colon, and even rectal cancer can be difficult. In daily practice, on the one hand, tumours localised adjacent to the ileocecal valve are correctly identified endoscopically. On the other hand, a malignancy located within 10 cm of the anal verge usually is considered a rectal cancer. Localisation of cancer in other parts of the colon can pose problems. Due to loops and curves the distance of a tumour from the anus can vary, even during the same procedure. For this reason the distance from the anal verge usually is measured during retrieval of the endoscope with a stretched colon. But even then, the exact anatomical localisation is difficult to assess. For this reason, especially in laparoscopic surgery, the tumour can be marked with an ink tattoo. Another accurate method of tumour localisation is placement of metal clips on the day of surgery, or intraoperative colonoscopy. Lesions in the upper rectum can be approached via intraoperative proctoscopy with or without suture placement (8). In case of tumour located in the proximal colon the exact anatomical localisation probably does not pose major problems during the laparoscopic approach. This will be definitely the case of the tumour is tattooed with ink. Furthermore, there will be no major impact on decisions regarding adjuvant systemic therapy. The differentiation between tumours in the distal sigmoid and the upper part of the rectum is of the utmost importance since the treatment strategies differ significantly. A distal colon cancer with mesenterial lymphnodes on the CT-scan is a N1 tumour that makes adjuvant chemotherapy necessary. Radiotherapy for distal colon cancer is not indicated. On the other hand rectal cancer is often treated with pre-operative radiation or chemoradiation.
CT-scan and MRI are essential for proper staging. With MRI of the rectum and pelvis insight can be gained into the depth of penetration into the wall or surrounding adipose tissue, lymph nodes and perirectal fascia. CT-scan probably is more suitable to assess metastatic disease. CT colonography with water enema can have role in the evaluation of patients. It can be used to in case of incomplete colonoscopy and investigate the colon in elderly patients (9).
Endoscopy is used for diagnosis and localisation. According to radiological criteria every tumour located caudally of the line from the promontorium to symphisis is considered a rectal cancer. However, the sigmoid can be very tortuous and return via several curves into the pelvic region. This makes it difficult for the radiologist to assess exactly the localisation of a cancer located in the lower part of the sigmoid. Feuerlein et al. studied staging CT without bowel preparation to accurately localise colonic tumours and compared the results to optical colonoscopy. They concluded that preoperative staging CT is more accurate than colonoscopy in the localisation of colonic tumours. However, rectal and cecal cancers were excluded (10).
Neri et al. compared the accuracy of conventional colonoscopy to CT-colonography. In terms of segmental localisation of masses, CT-colonography located precisely all lesions, whereas colonoscopy failed in 24% of the lesions, though six were missed because of incomplete colonoscopy (9%). In the remaining ten lesions, colonoscopy incorrectly located the tumour. The mismatch occurred in the rectum and sigmoid (n=5), but also the descending (n=1), transverse (n=2), ascending colon, and cecum. CT-colonography has better performance in the segmental localization of tumor (11).
The anatomical border between rectum and colon seems to be clear. The rectum is located below the peritoneum whereas the colon is located in the abdominal cavity. The resection specimen can provide the final details on anatomical localisation. The problem is that the peritoneal fold is not a straight horizontal line but can be oblique upward to the sacrum. This means that there is a transition zone with peritoneal coverage at the front and mesorectal fat and lymph nodes on the back. The best way to localise tumours in this zone is a combination of endoscopy, MRI, and digital examination.
The present study shows that endoscopy has specificity of 100% for rectal cancer. In other words, if the endoscopist claims the cancer is located in the rectum, he is correct. For radiological examination this is only 80%. For tumours located somewhat higher in the colon the specificity for cancer in the sigmoid is only 83% in case of endoscopy. In other words if the endoscopist thinks the tumour is located in the sigmoid it even might be a high rectal cancer. This is especially true for tumours located less than 20 cm from the anal verge.
The therapeutic strategy for tumours in this region is individualised and depends on the outcome of the multi-disciplinary meeting (12). The psychological burden of rectal cancer probably is greater because the patient has to undergo neo-adjuvant treatment before definite surgery. In case of a cancer located in the sigmoid the patient usually undergoes surgery within two weeks after diagnosis. On the other hand overtreatment can occur with adjuvant chemotherapy if a rectal cancer is considered sigmoidal. If there is discrepancy between endoscopy and radiology, especially, the CT-scan and the MRI should be studied very carefully in order to differentiate between a high rectal cancer or a low sigmoidal cancer. Only then a correct decision can be made regarding further treatment of the patient. Both the endoscopist and the radiologist should not be too overconfident in cases of high rectal or low sigmoidal cancer. Radiological examinations should be studied carefully, and loops of the sigmoid below the line of the promontorium should be taken into account.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Parkin DM, Bray F, Ferlay J, et al. Global cancer statistics, 2002. CA Cancer J Clin 2005;55:74-108. [PubMed]
- Rim SH, Seeff L, Ahmed F, et al. Colorectal cancer incidence in the United States, 1999-2004: an updated analysis of data from the National Program of Cancer Registries and the Surveillance, Epidemiology, and End Results Program. Cancer 2009;115:1967-76. [PubMed]
- de Gramont A, Van Cutsem E, Schmoll HJ, et al. Bevacizumab plus oxaliplatin-based chemotherapy as adjuvant treatment for colon cancer (AVANT): a phase 3 randomised controlled trial. Lancet Oncol 2012;13:1225-33. [PubMed]
- Haller DG, Tabernero J, Maroun J, et al. Capecitabine plus oxaliplatin compared with fluorouracil and folinic acid as adjuvant therapy for stage III colon cancer. J Clin Oncol 2011;29:1465-71. [PubMed]
- Twelves C, Scheithauer W, McKendrick J, et al. Capecitabine versus 5-fluorouracil/folinic acid as adjuvant therapy for stage III colon cancer: final results from the X-ACT trial with analysis by age and preliminary evidence of a pharmacodynamic marker of efficacy. Ann Oncol 2012;23:1190-7. [PubMed]
- Ngan SY, Burmeister B, Fisher RJ, et al. Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 2012;30:3827-33. [PubMed]
- Glimelius B. Neo-adjuvant radiotherapy in rectal cancer. World J Gastroenterol 2013;19:8489-501. [PubMed]
- Kim SH, Milsom JW, Church JM, et al. Perioperative tumor localization for laparoscopic colorectal surgery. Surg Endosc 1997;11:1013-6. [PubMed]
- Soyer P, Hamzi L, Sirol M, et al. Colon cancer: comprehensive evaluation with 64-section CT colonography using water enema as intraluminal contrast agent-a pictorial review. Clin Imaging 2012;36:113-25. [PubMed]
- Feuerlein S, Grimm LJ, Davenport MS, et al. Can the localization of primary colonic tumors be improved by staging CT without specific bowel preparation compared to optical colonoscopy? Eur J Radiol 2012;81:2538-42. [PubMed]
- Neri E, Turini F, Cerri F, et al. Comparison of CT colonography vs. conventional colonoscopy in mapping the segmental location of colon cancer before surgery. Abdom Imaging 2010;35:589-95. [PubMed]
- Glimelius B. Multidisciplinary treatment of patients with rectal cancer: Development during the past decades and plans for the future. Ups J Med Sci 2012;117:225-36. [PubMed]


