Adenosquamous carcinoma of the pancreas, also referred
to as “adenocanthoma” and “mucoepidermoid carcinoma”
(
1,
2) is a rare entity, representing only 1-4% of all known
pancreatic malignancies (
3-5). Similar to adenocarcinoma,
the most common symptoms associated with ASC are
weight loss, anorexia, malaise, abdominal pain, fatigue and
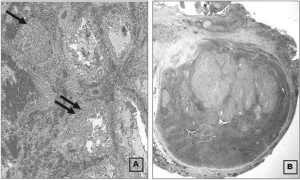
nausea. These tumors possess components of both glandular
and malignant squamous cell origins, which should both
be present to ensure proper diagnosis. Diagnosis of ASC
is challenging and frequently not made until the time of
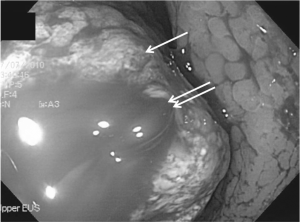
surgery or during post-mortem examination. The use of
ultrasound-guided FNA or ERCP-guided aspiration for
making a pre-operative diagnosis remains controversial.
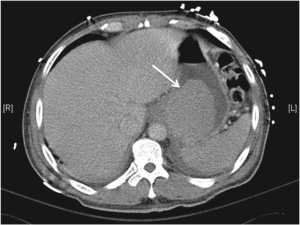
No imaging criteria are specific to ASC, causing most of
these tumors to be mistaken for ductal adenocarcinoma of
the pancreas when initially imaged. However, CT findings
of large pancreatic lesions with infiltration of surrounding
tissues and central necrosis have been reported and should
raise one’s suspicion for ASC (
6).
Widely disseminated disease is commonly present at the
time of initial presentation. Although diffuse disease usually
prevents resection, palliative surgery may still be indicated
in cases of hemorrhage, perforation or obstruction.
Even when potentially curative surgical resection is
performed, prognosis is generally regarded as extremely
poor. In 2008, Okabayashi et al reviewed 39 cases of ASC
treated with pancreatic resection (pancreaticodudenectomy,
distal pancreatectomy or total pancreatectomy) spanning
1980 through 2007 (
7). In this review, the 1-year and 3-year
survival rates following pancreatic resection were 25%
and 14%. Nevertheless, some reports have demonstrated a
survival benefit for patients undergoing an R0 resection (
8).
Similarly, Voong et al showed a survival benefit for patients
treated with adjuvant chemoradiation therapy (
4).
While direct invasion of adjacent organs has been
reported for ASC (
5), it usually does not lead to erosion
through the wall of hollow viscera. When present, this
presents an obvious challenge to the surgeon, but should
not be interpreted as a contraindication to surgical resection. Gastrointestinal bleeding has been associated
with tumors of multiple abdominal organs, but rarely so
with primary lesions of the pancreas. Several treatment
strategies for malignancy-related GI bleeding are commonly
employed, including endoscopic techniques, angiographic
embolization and surgical therapy (
9). All modalities are
useful in the appropriate setting, but treatment must be
individualized for each case.
In conclusion, we present a case of a 57 year-old male
with adenosquamous carcinoma of the pancreas. Our case
is unique in that we consider it to be the first that presented
as a massive, acute upper gastrointestinal bleed after erosion
through the posterior gastric wall. This case illustrates an
atypical presentation for this disease, forcing us to heighten
our awareness of these lesions in order to ensure prompt
diagnosis in future cases.