Adjuvant intraoperative post-dissectional tumor bed chemotherapy—A novel approach in treating midgut neuroendocrine tumors
Introduction
Small bowel neuroendocrine tumor (NET) is a rare and indolent disease. In general, patient presents with non-specific and vague symptoms that eludes the accurate diagnosis for years. As a result, patients often were diagnosed at late advanced stage with extensive and boggy mesenteric lymph node metastasis and or liver metastasis. Worse of all, with the impression of a “benign” and indolent natural history of this rare malignancy, wait and see approach has been generally accepted and practiced by most physicians. Hence patients presenting at a referral center are usually extremely advanced with boggy and massive mesenteric lymphadenopathy and distant liver metastasis.
Such boggy and extensive mesenteric lymph node metastasis from midgut NETs can be a daunting and dire problem for both the patients and their treating physicians especially the surgeons because it often causes encasement of the mesenteric vessels thus leading to mal-absorption, intestinal angina, bowel ischemia or strangulation and in some untreated patients the eventual demise. The only viable option in treating this condition is surgical resection and debulking. However, in reality, patients with such advanced disease are often deemed unresectable and referred to comfort measures or hospice care only.
Surgical debulking and resection of mesenteric lymph nodes is an extremely difficult and potentially dangerous procedure as massive bleeding, vascular injury or manipulation induced thrombosis and worsening bowel ischemia from disrupting collateral vessels can all be the unwanted consequences. For years it has been considered a forbidden surgery. None the less, within the last 10-15 years, surgeons in the specialized medical centers around the world have begun to explore the possibility of resecting and/or debulking of this metastasis. Collectively, as a group or individually, surgeons have developed methods and gained experiences in the recent years in attempt to resolve such problems with resection or debulking.
In order to restore the mesenteric circulation and to relieve the associated symptoms, aggressive and delicate surgical resection must be undertaken. None the less, even with the most careful, deliberated, extensive and delicate dissection, micro or macro residual disease at the dissection sites remains a real possibility and concern. These residuals, even the microscopic ones, could potentially lead to local recurrence and or more concerning a possible late progression to distant disease eventually. Therefore additional novel intra-operative adjuvant therapy is in dire need to address this issue.
In order to eliminate the residual micro or macroscopic disease and to assure hemostasis after an extensive peri-vascular dissection to reduce post-operative local tumor recurrence and bleeding, the author has explored and developed a novel approach by adopting local application of adjunct chemotherapy in and around the surgical resection bed. Strips of 5-fluorouracil (5-FU) saturated gelfoam were incorporated into the mesenteric defect and the tumor resection bed after mesenteric lymph node dissection. I believe this local intra-operative intra-resection bed adjunct chemotherapy will aid in reducing or eliminating micro or macro residual disease, thus delaying or even preventing local recurrence. To the minimum, it would at least enhance the hemostatic effect of contact hemostatic agent.
Operative technique
Using open laparotomy, patients with midgut primary NETS and bulky mesenteric lymph nodes were explored. Lymphatic mapping was applied to guide the resection margin and dissection boundary (1). Small bowel primary and its associated draining mesentery were resected. Dedicated and extensive mesenteric lymph nodes dissection was then conducted to achieve a maximum and yet safe cytoreduction without the consequences of massive blood loss and thrombosis of vessels or worsening of pre-existing bowel ischemia. Small bowel anastamosis were then constructed in a side to side and functionally end to end fashion using a GIA staple. Abdomen was thoroughly irrigated and hemostasis were double checked and secured. Mesenteric defect were than closed in two layers using dissolvable sutures by first to re-approximate the posterior leaflet of the mesenteric peritoneum. Following the closing of the posterior leaflet of mesenteric peritoneum, strips of 5-FU treated gelfoam are then placed into the partially closed mesenteric defect. The anterior leaflet mesenteric peritoneum was then closed to contain the 5-FU soaked gelfoam strips in place like making a Chinese dumpling. The 5-FU solution is usually prepared with 40-60 mg of 5-FU to be dissolved in 40-60 cc of normal saline to give a concentration of 1 mg/cc. Two to four pieces of gelfoam were then soaked in this 5-FU solution. The gelfoam strips were then tailored and placed into the mesenteric defect once the gelfoam became saturated and softened. Abdomen was then closed to conclude the operation.
Methods
Retrospectively, charts of 62 consecutive midgut NET patients with boggy mesenteric lymphadenopathy who underwent cytoreductive debulking surgeries from 1/2007 to 12/2009 were reviewed. A total of 32 patients received an intraoperative application of 5-FU saturated gelfoam strips secured into the mesenteric defect following the extensive lymphadenectomy. A total of 30 untreated patients served as control.
Results
The 5-year survival after cytoreductive surgeries was 22/32 (68.8%) for the treated group, vs. 20/30 (66.7%) for the control. Six patients (6/32, 18.8%) among the study group required additional debulking surgeries, vs. 16 patients (16/30, 53.3%) in the control group. Upon reoperation, locoregional recurrence was noted in 9 of the 16 patients (56.3%) in the control group, vs. only 2/6 (33.3%) of treated patients. Overall, local recurrent rate is 6.25% (2/32) in the treated group vs. 30% (9/30) in the control group. Post-op complication rates are similar in the two arms.
Discussion
Midgut NETS is a rare disease with an incidence of 1/100,000-4.3/100,000 population (2). The presenting symptoms are usually vague and non-specific and the diagnosis is generally delayed. Patients often diagnosed at late advanced stage with extensive and boggy mesenteric lymph mode metastasis and or liver metastasis (3). To make the matter even worse, with the misguided conception of dealing with a “benign” or indolent rare malignancy, wait and see approach has been generally accepted and practiced by most physicians. As results of these popularized misleading information and wrongful impression of this disease, patients often present to tertiary center with extremely advanced disease with boggy and massive mesenteric lymphadenopathy and distant liver metastasis (4,5).
Boggy massive and extensive mesenteric lymph node metastasis from midgut NETS can be a daunting and dire problem for both patients and their treating surgeons because it often causes encasement of the mesenteric vessels which in turns leads to mal-absorption, intestinal angina, bowel ischemia or strangulation and in some untreated patients the eventual demise. The only viable option in treating this condition is surgical resection and debulking. However, in general patients with such advanced disease are often deemed unresectable and offered none or palliative treatment only.
Surgical debulking and resection of mesenteric lymph nodes is an extremely difficult and potentially dangerous procedure as massive bleeding, vascular manipulation or injury induced thrombosis and worsening bowel ischemia from disrupting collateral vessels can all be the unwanted consequences. For years it has been considered a forbidden surgery. However, surgeons in the specialized medical centers around the world have begun to take much aggressive and bold approach while confronted with such conditions in recent years. Exploration with attempt of possible resection and debulking is now the procedure of choice in specialized medical center to address such problems. Collectively, as a group or individual surgeons have developed methods and gained experiences in such resective and debulking procedure (6-8).
However, in order to have a successful surgical treatment to restore the mesenteric circulation and to relieve the associated symptoms, aggressive and delicate surgical resection must be performed. None the less, even with the most careful, deliberated, extensive and delicate dissection, micro or macro residual disease at the dissection sites remains a distinctive possibility. These residuals, even the microscopic ones, could potentially lead to local recurrence and or a possible progression to distant disease. Therefore additional novel intra-operative adjuvant therapy is in dire need to address this issue.
Well differentiated NETs are in general poor candidates for systemic chemotherapy due to the fact that there are only a few duplicating cells within the tumors that can be the treatment target of chemotherapy agents. Our laboratory studies, however, have revealed that 69% of the NETS cells are sensitive to 5-FU treatment while the agent is given directly into the culture media of living cancer cells in vitro (9). Our study has suggested that direct delivery of 5-FU to the tumor cells within diffusion distance might provide some tumoricidal or at least static effects to this slow growing tumor.
The 5-FU, a pyrimidine analog, is one of the well know and established chemotherapy agents that has been used to treat different kinds of cancers such as colorectal, stomach, pancreas, liver, ovarian, breast and head neck cancers for years. It can be administered via many different routes, most commonly given as intravenous infusion. However, oral administration, intra-peritoneal perfusion, intra-arterial infusion and more recently topical applications have all been utilized. In addition to its anti-neoplastic capacity, it also carries prothrombotic and procoagulant effects (10-12) and can enhance the hemostatic effect of contact hemostatic agents. It has been applied on the liver resection surface in combination with cergicell for hemostatic purpose.
Adjunctive 5-FU chemotherapy, is in general given systemically after initial surgical or radiation therapy by either intravenous or intra-arterial infusion or alternatively by oral administration. Intra-op intra-peritoneal chemoinfusion has gained some momentum in recent years to treat intra-peritoneal carcinomatosis following maximum deliberated surgical debulking. Local chemotherapy has been applied with some success in treating some early staged skin cancer. Intra-peritoneal local chemotherapy, in contrast, has never been utilized or reported.
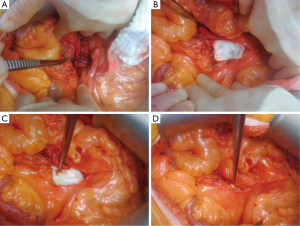
In order to eliminate the residual micro or macroscopic disease and to assure hemostasis after extensive mesenteric dissection to reduce the chance of local tumor recurrence and post-operative bleeding, the author has explored and developed a novel approach of incorporating local chemotherapy as an intra-operative adjuvant to treat the regional micro or macro residual disease. At completion of an extensive mesenteric resection or debulking, strips of 5-FU saturated gelfoam were secured into the mesenteric defect (Figure 1). We believe this local intra-resection bed and intra-operative chemotherapy aids in eliminating or suppressing micro or macro residual disease thus delaying or even preventing local recurrence. Our results confirm our hypothesis.
For systemic therapy the common doses of 5-FU range from 200-600 mg/sq meter with the highest dose not to exceed 800 mg/sq meter and for topical application the concentration of 5-FU is 0.5-5% in cream and 2-5% in solution. The common sides effects following systemic administration of 5-FU include loss of appetite, headache, nausea, vomiting, diarrhea, mucositis, myelosuppression, alopecia, photosensitivity, hand-foot syndrome and pruritic maculopapular eruption.
In order to have a sustained slow release of high dose 5-FU as local chemotherapy agent, we use gelform media to carry the therapeutic agent. Gelfoam is a very posed and dissolvable contact hemostatic agent. It has been proven to be an effective hemostatic tool that would eventually be degraded and reabsorbed in vivo within six weeks without any discernible residual side effect. It has also been used to function as a medicine carrying media by colorectal surgeons for years as a lidocaine jell/gelfoam suppository to be placed in the rectal cannel after a trans-anal procedure. To have the high enough concentration of in vitro locally releasing 5-FU without possible side effect, we decided to make a concentration of 1 mg/cc 5-FU solution by dissolving 40-60 mg of 5-FU in 40-60 cc of normal saline. Compared to 5-FU systemic chemotherapy, 40 to 60 mg of 5-FU to be placed in a small defect of 3-10 cm in length is a mega dose as a slow releasing direct contact agent. However due to the extensive dissection, tumor resection bed is relatively ischemic thus preventing this local chemotherapy from leaching into systemic circulation. Hence, it can prevent any systemic side effects.
Conclusions
Intraoperative application of chemotherapy is a safe and effective adjuvant for suppressing and or eliminating any potential microscopic residual disease after extensive cytoreductive surgeries in advanced stage NET patients with mesenteric lymph node metastasis. It provides patients with sustained, slow releasing, high dose of 5-FU within the surgical bed without any discernible side effects, whereby reducing local recurrence rates and decreased need of reoperation. Long-term follow up and a more robust database analysis is needed to sustain this initial promising observation and to further endorse this new innovative surgical approach.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Wang YZ, Joseph S, Lindholm E, et al. Lymphatic mapping helps to define resection margins for midgut carcinoids. Surgery 2009;146:993-7. [PubMed]
- Modlin IM, Sandor A. An analysis of 8305 cases of carcinoid tumors. Cancer 1997;79:813-29. [PubMed]
- Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer 2003;97:934-59. [PubMed]
- Sartori P, Mussi C, Angelini C, et al. Palliative management strategies of advanced gastrointestinal carcinoid neoplasms. Langenbecks Arch Surg 2005;390:391-6. [PubMed]
- Chambers AJ, Pasieka JL, Dixon E, et al. The palliative benefit of aggressive surgical intervention for both hepatic and mesenteric metastases from neuroendocrine tumors. Surgery 2008;144:645-51; discussion 651-3. [PubMed]
- Söreide JA, van Heerden JA, Thompson GB, et al. Gastrointestinal carcinoid tumors: long-term prognosis for surgically treated patients. World J Surg 2000;24:1431-6. [PubMed]
- Ohrvall U, Eriksson B, Juhlin C, et al. Method for dissection of mesenteric metastases in mid-gut carcinoid tumors. World J Surg 2000;24:1402-8. [PubMed]
- Hellman P, Lundström T, Ohrvall U, et al. Effect of surgery on the outcome of midgut carcinoid disease with lymph node and liver metastases. World J Surg 2002;26:991-7. [PubMed]
- Lyons JM 3rd, Abergel J, Thomson JL, et al. In vitro chemoresistance testing in well-differentiated carcinoid tumors. Ann Surg Oncol 2009;16:649-55. [PubMed]
- Oberhoff C, Winkler UH, Hoffmann O, et al. Adjuvant CMF-chemotherapy and haemostasis. Effect of "classical" and "modified" adjuvant CMF-chemotherapy on blood coagulation fibrinolysis in patients with breast cancer. Eur J Gynaecol Oncol 2000;21:147-52. [PubMed]
- Pectasides D, Tsavdaridis D, Aggouridaki C, et al. Effects on blood coagulation of adjuvant CNF (cyclophosphamide, novantrone, 5-fluorouracil) chemotherapy in stage II breast cancer patients. Anticancer Res 1999;19:3521-6. [PubMed]
- Rella C, Coviello M, Giotta F, et al. A prothrombotic state in breast cancer patients treated with adjuvant chemotherapy. Breast Cancer Res Treat 1996;40:151-9. [PubMed]