Coexistence of intestinal Kaposi sarcoma and plasmablastic lymphoma in an HIV/AIDS patient: case report and review of the literature
Introduction
Human immunodeficiency virus (HIV) infection or acquired immunodeficiency disease (AIDS) is associated with increased risk for various malignancies including Kaposi sarcoma (KS) and lymphoma (1-3). Although the skin is the most common site of involvement for KS, the gastrointestinal (GI) tract is also often involved in HIV/AIDS patients (4). Lymphoma is another common GI malignancy seen in AIDS patients. Here we report a case of HIV/AIDS with multiple HIV-associated malignancies involving the GI tract.
Case presentation
A 32-year-old Hispanic male patient with a history of HIV and cutaneous KS presented to the ED with bloody diarrhea. Lab tests confirmed HIV with increased HIV viral load in peripheral blood (590K copies/mL) and decreased CD4 count (251/µL, 12%). The patient was receiving highly active antiretroviral therapy (HAART) treatment previously and was suspected to be non-compliant with his medication regimen. Esophagogastroduodenoscopy suggested esophagitis in the middle and distal thirds of the esophagus and multiple erythematous nodules were found in the second and third portions of the duodenum. Colonoscopy also revealed numerous erythematous nodules in the colon. Multiple biopsies from the GI tract were taken for pathological examination.
Histopathology
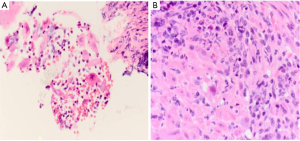
The esophageal biopsies showed ulcerative esophagitis with prominent lymphoplasmacytic infiltrate positive for herpetic viral and cytomegaloviral inclusions, indicative of immunodeficiency in the patient (Figure 1).
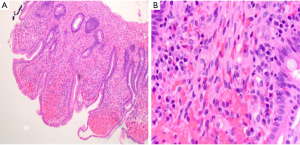
Multiple biopsies of the duodenum showed histopathological findings consistent with GI KS (Figure 2): spindle cells form slit-like spaces containing red blood cells as well as presence of extravasated red blood cells. The lesion packed the lamina propria accompanied by a variably mixed mononuclear inflammatory cell infiltrate. Usually, the tumor cells display strong immunoreactivity for HHV8 LNA-1 antibody. In the current case, given the history of HIV and presence of multiple skin KSs combined with typical histopathological findings of KS, no HHV8 LNA-1 immunostaining was performed.
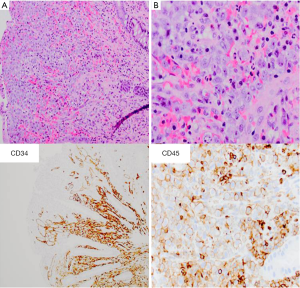
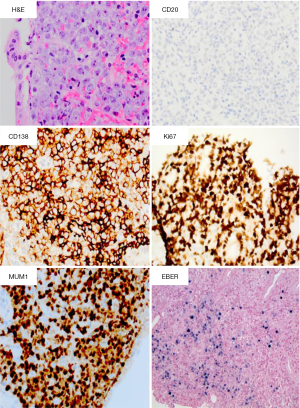
Interestingly, in the multiple fragments from colonic mucosa, as in the duodenum, KS was identified and the haphazard vascular network of KS was highlighted by CD34 (Figure 3). Furthermore, foci of atypical large cell infiltration were found on the surface of the colonic mucosa separate from the KS lesion. These large cells often appeared plasmacytoid/immunoblastic with abundant cytoplasm, eccentric nuclei and variably prominent nucleoli with disruption of the lamina propria and mucosal surfaces demonstrated. The large cells were CD45 positive, suggestive of hematopoietic cell lesions. Further immunohistochemical studies were carried out to help diagnose the colonic lesions. The atypical large cells were positive for CD138, MUM-1, CD30, and CD4 but negative for CD20. Ki-67 stain showed a very high proliferative index (Figure 4). Given the patient’s history of HIV infection, the morphological and immunophenotypic features were most consistent with the diagnosis of plasmablastic lymphoma (PBL). Further testing for positive EBV (EBER) and negative anaplastic lymphoma kinase (ALK) confirmed the diagnosis.
Discussion
HIV/AIDS is associated with increased risk for multiple malignancies, including KS and lymphoma (1-3). In the current case, the HIV patient presented with multiple KSs and coexistent PBL in the GI tract. The patient also displayed esophagitis associated with multiple viral infections including herpes and cytomegalovirus. This unique case fully exemplified that immunodeficiency in HIV/AIDS patients may lead to multiple viral infections and increased risk for various malignancies in the intestinal tract.
PBL is a rare form of AIDS-related lymphoma, only accounting for approximately 2.6% of lymphomas. The exact incidence of PBL is not known, but almost all of them are associated with HIV infection or conditions of immunosuppression (5-8). In a comprehensive review of PBL by Castillo et al., most of the PBL occurred in the oral cavity with only approximately 13% of the 112 reported PBL originating in the GI tract (9). Similar to other common lymphomas in the GI tract, clinical symptoms of PBL include abdominal pain, diarrhea, nausea and GI bleeding (9). HIV-associated PBL is aggressive, and 60% of patients present with advanced clinical stage at diagnosis (9-11).
The exact mechanism of lymphomagenesis in HIV patients is not completely understood. HIV is not regarded as a directly transforming virus due to lack of consistent insertion at a transformative site (11). Instead, HIV infection disrupts normal immunomodulatory functions, which allows super-infection by other oncogenic viral pathogens such as Epstein-Bar virus and Kaposi-sarcoma virus, subsequently leading to multiple malignancies such as various lymphomas and KSs (12).
HIV targets human CD4 “Helper” T-cells due to high affinity of viral gp120 proteins for the CD4 molecules. CD4 T-cells function as immune system modulators in both adaptive immune system (i.e., B cells) as well as the innate immune system (e.g., macrophages and monocytes). Once infected by HIV, CD4 cells cannot execute the normal immunomodulatory functions, and eventually are depleted through activation-induced cell death (13,14).
EBV infection has been postulated in the development of many lymphomas. Most lymphomas in HIV-infected patients also show EBV positivity, especially PBL, 60-100% of which are EBV positive (6,8,15). EBV may contribute to lymphomagenesis in variety of ways. The EBV genome encodes a variety of products promoting EBV infection and transformation. For example, the EBV latent membrane protein 1 (LMP1), a constitutively active viral protein, was able to transform lymphocytes in mouse cell models and is required for EBV-mediated B-cell transformation (16,17). LMP2A increases the expression of genes associated with cell cycle induction and inhibition of apoptosis, and alters gene expression profile similar to those described in Hodgkin/Reed-Sternberg (HRS) cells of Hodgkin lymphoma. LMP2A expression may lead to development of Hodgkin lymphoma (18). Epstein Barr nuclear antigens (EBNAs) can directly interfere with P53 and P16 functions (19,20). Furthermore, recent data suggest that HIV may directly contribute to the development of lymphomas in HIV patients by inducing B-cell activation. HIV gp120 has been shown to activate B cells and induce class switch recombination from IgM to IgA and IgG by up-regulating activation-induced cytidine deaminase (21). Recently, another HIV P17 matrix protein with different variants has been found being able to directly promote B-cell growth and thus possibly contribute to malignant transformation of B cells (22).
Lymphomagenesis is complex, and the mechanisms for the pathogenesis of different types of lymphomas in HIV patients are far from clear. PBL is thought to derive from post germinal-center, terminally differentiated B cells, probably in transition from immunoblast to plasma cells (23,24). A recent study has shown that recurring rearrangements involving MYC, a well-known oncogene with the immunoglobulin gene, in PBL (25).
Diagnosis of GI PBL needs endoscopic biopsy and pathological examination. The 2008 World Health Organization (WHO) classification of Tumors of Hematopoietic and Lymphoid Tissues specifically recognizes PBL as a diffuse immunoblastic lymphoma. Morphologically, the cells resemble immunoblasts with some plasmacytic differentiation. They are large and have round to oval nuclei that may be eccentrically located. A single central prominent nucleolus or several peripherally located nucleoli are present, and the cytoplasm is moderate to abundant with a paranuclear hof. However, a plasmablastic morphology may be seen in other lymphoproliferative disorders, such as multiple myeloma, Burkitt lymphoma, diffuse large B-cell lymphoma (DLBCL) with plasmacytoid differentiation and ALK-positive DLBCL. Immunophenotyping has great value in differentiating PBL from other neoplasms. PBL has the features of plasma cells such as CD138 and IRF4/MUM1 positivity, but are negative or weakly positive for CD20 or PAX5. EBV by EBER in situ hybridization is positive in most cases, but LMP1 is variably expressed due to low sensitivity. The cytogenetic changes of PBLs are unclear yet. But deregulation of MYC gene expression through translocation or amplification has been reported in 49% of the cases. The common translocations include immunoglobulin heavy-chain, kappa or lambda light-chain genes, like Burkitt lymphoma (23,24).
KS is a rare mesenchymal tumor involving blood and lymphatic vessels, and was first described by Dr. Kaposi in 1872 (26). However, the incidence increases significantly in the HIV/AIDS population, and the rate of epidemical KS was 100,000-fold greater than that of the general population (27). KS is classified into four forms: classic KS, endemic African KS, iatrogenic/immunosuppressive KS, and AIDS-related KS. AIDS-related KS is the most aggressive form. KS is primarily a skin lesion, but sometimes involves visceral organs. Visceral involvement, such as GI tract involvement, is especially common in AIDS-KS with nearly a quarter of patients having GI tract involvement (28-31).
Human herpesvirus-8 (HHV8), also known as KS-associated herpesvirus (KSHV), is etiologically associated with KS (32,33). Following the acute infection, the virus establishes latent infection inside cells. KSHV codes for a functional bcl-2 homologue, which disrupts the antiapoptotic effects of bcl-2 protein and may contribute to neoplastic cell expansion (34). KSHV-encoded G-protein couple receptor (GPCR) may also act as a vial oncogene. KSHV also codes for proteins mimicking human cytokines such as IL-6, IL-6, which can activate VEGF and induce angiogenesis (35). Expression of those viral genes disrupts immune response and signaling pathways, leading to increased cell proliferation, angiogenesis and local inflammation and eventually the initiation and progression of KS (29). KS growth is further enhanced by HIV coinfection. HIV infection significantly decreases the host immune surveillance, which plays a key role in eliminating the virus during the acute infection and suppressing viral reactivation. HIV-1 virus also induces various inflammatory cytokines and growth factors that enhance tumor growth (2,36,37).
Clinical presentations of GI tract involvement by KS vary from asymptomatic to diarrhea and intestinal bleeding. As the lesions grow, symptoms of intestinal obstruction and intussusception may occur (38-40). The gross appearances of GI tract KS under endoscopy vary from erythematous macules or papules to polypoid lesions (41-43).
The histological features of GI KS are similar to cutaneous KS, which show spindle cells forming slit-like spaces containing red blood cells and pack the intestinal lamina propria. The lesions can sometimes infiltrate the overlying mucosa (29,44,45). KS cells are usually positive with the endothelial markers such as CD31, CD34, and factor VIII-related antigen. The diagnosis of KS has been greatly simplified using immunohistochemical stain for HHV-8 latent nuclear antigen (LNA-1) in regards to differentiation from other vascular lesions (46-48).
Several lesions in the GI tract may mimic KS including GI angiosarcoma, bacillary angiomatosis and pyogenic granuloma. Both angiosarcomas and KS are positive for vascular endothelial markers, however, clinically angiosarcomas are not associated with HIV/AIDS or immunosuppression (49-51). Bacillary angiomatosis also often occurs in immunocompromised patients such as those with HIV infection. It often presents as a cutaneous lesion but occasionally occurs in GI tract. However, Warthin-Starry staining will reveal the existence of extracellular bacilli (52-54). Pyogenic granuloma is a lobular hemangioma which commonly occurs in skin but occasionally occurs in the GI tract. Histologically the features of slit-like vessel channels, endothelial nuclear atypia, and red blood cell extravasation often present in KS will not be present in pyogenic granuloma (55-57). In difficult cases, HHV-8 latent nuclear antigen (LNA-1) staining can help, and it is positive in KS and negative in other lesions.
In conclusion, this case shows concurrence of two HIV-associated malignancies in the GI tract: a relatively common malignancy of KS, and an uncommon malignancy of PBL. The coexistence of these two malignancies exemplified the increased risk for various malignancies in immunocompromised HIV/AIDS patients.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Rubinstein PG, Aboulafia DM, Zloza A. Malignancies in HIV/AIDS: from epidemiology to therapeutic challenges. AIDS 2014;28:453-65. [PubMed]
- Aboulafia DM. Human immunodeficiency virus-associated neoplasms: epidemiology, pathogenesis, and review of current therapy. Cancer Pract 1994;2:297-306. [PubMed]
- Grulich AE, van Leeuwen MT, Falster MO, et al. Incidence of cancers in people with HIV/AIDS compared with immunosuppressed transplant recipients: a meta-analysis. Lancet 2007;370:59-67. [PubMed]
- Hengge UR, Ruzicka T, Tyring SK, et al. Update on Kaposi's sarcoma and other HHV8 associated diseases. Part 1: epidemiology, environmental predispositions, clinical manifestations, and therapy. Lancet Infect Dis 2002;2:281-92. [PubMed]
- Carbone A, Gloghini A. Plasmablastic lymphoma: one or more entities? Am J Hematol 2008;83:763-4. [PubMed]
- Raphael M, Said J, Borisch B, et al. eds. Lymphomas associated with HIV infection. In: Swerdlow SH, Campo E, Harris NL, et al. eds. World Health Organization classification of tumors. Pathology and genetics of tumors of heamatopoietic and lymphoid tissues. Lyon: IARC Press, 2008:340-2.
- Castillo J, Pantanowitz L, Dezube BJ. HIV-associated plasmablastic lymphoma: lessons learned from 112 published cases. Am J Hematol 2008;83:804-9. [PubMed]
- Castillo JJ, Winer ES, Stachurski D, et al. Clinical and pathological differences between human immunodeficiency virus-positive and human immunodeficiency virus-negative patients with plasmablastic lymphoma. Leuk Lymphoma 2010;51:2047-53. [PubMed]
- Kaplan LD. HIV-associated lymphoma. Best Pract Res Clin Haematol 2012;25:101-17. [PubMed]
- Ho-Yen C, Chang F, van der Walt J, et al. Gastrointestinal malignancies in HIV-infected or immunosuppressed patients: pathologic features and review of the literature. Adv Anat Pathol 2007;14:431-43. [PubMed]
- Mitchell RS, Beitzel BF, Schroder AR, et al. Retroviral DNA integration: ASLV, HIV, and MLV show distinct target site preferences. PLoS Biol 2004;2:E234. [PubMed]
- Mahe E, Sur M. Benign and malignant lymphoproliferative disorders in HIV/AIDS. In: Dumais N, editor. HIV and AIDS-Updates on Biology, Immunology, Epidemiology and Treatment Strategies. Rijeka, Croatia: In Tech, 2011.
- McCune JM. The dynamics of CD4+ T-cell depletion in HIV disease. Nature 2001;410:974-9. [PubMed]
- Wain-Hobson S. HIV. One on one meets two. Nature 1996;384:117-8. [PubMed]
- Carbone A, Cesarman E, Spina M, et al. HIV-associated lymphomas and gamma-herpesviruses. Blood 2009;113:1213-24. [PubMed]
- Wang D, Liebowitz D, Kieff E. An EBV membrane protein expressed in immortalized lymphocytes transforms established rodent cells. Cell 1985;43:831-40. [PubMed]
- Kaye KM, Izumi KM, Kieff E. Epstein-Barr virus latent membrane protein 1 is essential for B-lymphocyte growth transformation. Proc Natl Acad Sci U S A 1993;90:9150-4. [PubMed]
- Portis T, Dyck P, Longnecker R. Epstein-Barr Virus (EBV) LMP2A induces alterations in gene transcription similar to those observed in Reed-Sternberg cells of Hodgkin lymphoma. Blood 2003;102:4166-78. [PubMed]
- Yi F, Saha A, Murakami M, et al. Epstein-Barr virus nuclear antigen 3C targets p53 and modulates its transcriptional and apoptotic activities. Virology 2009;388:236-47. [PubMed]
- Maruo S, Zhao B, Johannsen E, et al. Epstein-Barr virus nuclear antigens 3C and 3A maintain lymphoblastoid cell growth by repressing p16INK4A and p14ARF expression. Proc Natl Acad Sci U S A 2011;108:1919-24. [PubMed]
- He B, Qiao X, Klasse PJ, et al. HIV-1 envelope triggers polyclonal Ig class switch recombination through a CD40-independent mechanism involving BAFF and C-type lectin receptors. J Immunol 2006;176:3931-41. [PubMed]
- Giagulli C, Marsico S, Magiera AK, et al. Opposite effects of HIV-1 p17 variants on PTEN activation and cell growth in B cells. PLoS One 2011;6:e17831. [PubMed]
- Castillo JJ, Reagan JL. Plasmablastic lymphoma: a systematic review. ScientificWorldJournal 2011;11:687-96. [PubMed]
- Stein H, Harris N, Campo E. Plasmablastic lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al, editors. World Health Organization classification of tumors. Pathology and genetics of tumors of hematopoietic and lymphoid tissues. Lyon: IARC Press, 2008:256-7.
- Valera A, Balagué O, Colomo L, et al. IG/MYC rearrangements are the main cytogenetic alteration in plasmablastic lymphomas. Am J Surg Pathol 2010;34:1686-94. [PubMed]
- Kaposi M. Idiopatisches multiples pigmentsarkom der haut. Arch Dermatol Syph 1872;3:265-73.
- Beral V, Peterman TA, Berkelman RL, et al. Kaposi's sarcoma among persons with AIDS: a sexually transmitted infection? Lancet 1990;335:123-8. [PubMed]
- Antman K, Chang Y. Kaposi's sarcoma. N Engl J Med 2000;342:1027-38. [PubMed]
- Aboulafia DM. Kaposi's sarcoma. Clin Dermatol 2001;19:269-83. [PubMed]
- Parente F, Cernuschi M, Orlando G, et al. Kaposi's sarcoma and AIDS: frequency of gastrointestinal involvement and its effect on survival. A prospective study in a heterogeneous population. Scand J Gastroenterol 1991;26:1007-12. [PubMed]
- Barrison IG, Foster S, Harris JW, et al. Upper gastrointestinal Kaposi's sarcoma in patients positive for HIV antibody without cutaneous disease. Br Med J (Clin Res Ed) 1988;296:92-3. [PubMed]
- Chang Y, Cesarman E, Pessin MS, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science 1994;266:1865-9. [PubMed]
- Huang YQ, Li JJ, Kaplan MH, et al. Human herpesvirus-like nucleic acid in various forms of Kaposi's sarcoma. Lancet 1995;345:759-61. [PubMed]
- Sarid R, Sato T, Bohenzky RA, et al. Kaposi's sarcoma-associated herpesvirus encodes a functional bcl-2 homologue. Nat Med 1997;3:293-8. [PubMed]
- Bais C, Santomasso B, Coso O, et al. G-protein-coupled receptor of Kaposi's sarcoma-associated herpesvirus is a viral oncogene and angiogenesis activator. Nature 1998;391:86-9. [PubMed]
- Whelan P, Scadden DT. New developments in the etiopathogenesis and treatment of HIV-related Kaposi's sarcoma. Clin Dermatol 2000;18:469-77. [PubMed]
- Mesri EA. Inflammatory reactivation and angiogenicity of Kaposi's sarcoma-associated herpesvirus/HHV8: a missing link in the pathogenesis of acquired immunodeficiency syndrome-associated Kaposi's sarcoma. Blood 1999;93:4031-3. [PubMed]
- Lin CH, Hsu CW, Chiang YJ, et al. Esophageal and gastric Kaposi's sarcomas presenting as upper gastrointestinal bleeding. Chang Gung Med J 2002;25:329-33. [PubMed]
- Neville CR, Peddada AV, Smith D, et al. Massive gastrointestinal hemorrhage from AIDS-related Kaposi's sarcoma confined to the small bowel managed with radiation. Med Pediatr Oncol 1996;26:135-8. [PubMed]
- Wang NC, Chang FY, Chou YY, et al. Intussusception as the initial manifestation of AIDS associated with primary Kaposi's sarcoma: a case report. J Formos Med Assoc 2002;101:585-7. [PubMed]
- Friedman SL, Wright TL, Altman DF. Gastrointestinal Kaposi's sarcoma in patients with acquired immunodeficiency syndrome. Endoscopic and autopsy findings. Gastroenterology 1985;89:102-8. [PubMed]
- Sakagami J, Sogame Y, Kataoka K, et al. Endoscopic resection for the diagnosis of visceral Kaposi's sarcoma. J Gastroenterol 2005;40:98-103. [PubMed]
- Weprin L, Zollinger R, Clausen K, et al. Kaposi's sarcoma: endoscopic observations of gastric and colon involvement. J Clin Gastroenterol 1982;4:357-60. [PubMed]
- McNutt NS, Fletcher V, Conant MA. Early lesions of Kaposi's sarcoma in homosexual men. An ultrastructural comparison with other vascular proliferations in skin. Am J Pathol 1983;111:62-77. [PubMed]
- Zhang YM, Bachmann S, Hemmer C, et al. Vascular origin of Kaposi's sarcoma. Expression of leukocyte adhesion molecule-1, thrombomodulin, and tissue factor. Am J Pathol 1994;144:51-9. [PubMed]
- Russell Jones R, Orchard G, Zelger B, et al. Immunostaining for CD31 and CD34 in Kaposi sarcoma. J Clin Pathol 1995;48:1011-6. [PubMed]
- Patel RM, Goldblum JR, Hsi ED. Immunohistochemical detection of human herpes virus-8 latent nuclear antigen-1 is useful in the diagnosis of Kaposi sarcoma. Mod Pathol 2004;17:456-60. [PubMed]
- Xu H, Edwards JR, Espinosa O, et al. Expression of a lymphatic endothelial cell marker in benign and malignant vascular tumors. Hum Pathol 2004;35:857-61. [PubMed]
- Sherid M, Sifuentes H, Brasky J, et al. Clinical and endoscopic features of angiosarcoma of the colon: two case reports and a review of the literature. J Gastrointest Cancer 2013;44:12-21. [PubMed]
- Chen J, Zheng Q, Huang XY, et al. Upper gastrointestinal hemorrhage caused by duodenal angiosarcoma. Am Surg 2012;78:E258-9.
- Allison KH, Yoder BJ, Bronner MP, et al. Angiosarcoma involving the gastrointestinal tract: a series of primary and metastatic case. Am J Surg Pathol 2004;28:298-307. [PubMed]
- Chetty R, Sabaratnam RM. Upper gastrointestinal bacillary angiomatosis causing hematemesis: a case report. Int J Surg Pathol 2003;11:241-4. [PubMed]
- Cotell SL, Noskin GA. Bacillary angiomatosis. Clinical and histologic features, diagnosis, and treatment. Arch Intern Med 1994;154:524-8. [PubMed]
- Koehler JE, Cederberg L. Intra-abdominal mass associated with gastrointestinal hemorrhage: a new manifestation of bacillary angiomatosis. Gastroenterology 1995;109:2011-4. [PubMed]
- Yao T, Nagai E, Utsunomiya T, et al. An intestinal counterpart of pyogenic granuloma of the skin. A newly proposed entity. Am J Surg Pathol 1995;19:1054-60. [PubMed]
- van Eeden S, Offerhaus GJ, Morsink FH, et al. Pyogenic granuloma: an unrecognized cause of gastrointestinal bleeding. Virchows Arch 2004;444:590-3. [PubMed]
- Carmen González-Vela M, Fernando Val-Bernal J, Francisca Garijo M, et al. Pyogenic granuloma of the sigmoid colon. Ann Diagn Pathol 2005;9:106-9. [PubMed]


