Single centre outcomes from definitive chemo-radiotherapy and single modality radiotherapy for locally advanced oesophageal cancer
Introduction
Oesophageal cancer (OC) is the 13th most common cancer in the UK, accounting for 3% of new cases of cancer diagnosed in 2011 (1). The management of loco-regional OC has undergone significant evolution over the past 20 years.
Low cure rates after local treatment alone prompted the inclusion of systemic chemotherapy into multi-modality regimens. For patients with adenocarcinoma (ACA) optimal treatment in the UK is still considered to be neo-adjuvant chemotherapy followed by surgery as demonstrated in the MAGIC and OEO-2 trials (2). Several UK cases series have demonstrated than only 30-40% of OCs are resectable at presentation. Operative mortality rates remain in the region of 4.5-10.1% with 2-year survival rates of 34-43% and overall 5-year survival of 17-23% in addition surgery has been demonstrated to have a detrimental effect on health-related quality of life (3,4).
Single modality radical radiotherapy has been shown in historical case series to have 5-year survival rates of between 5-20% (5). Later single-institution studies have demonstrated 3- and 5-year survival rates of 27% and 21% respectively using modern disease staging and radiotherapy protocols (6-8). Disappointing outcomes from single modality radiotherapy led to the introduction of concurrent cytotoxic chemotherapy first described in 1968. This approach led to superior outcomes for patients when compared to radiotherapy alone (9,10).
Definitive chemo-radiotherapy (dCRT) has been demonstrated to result in long-term survival in patients with oesophageal carcinoma. Three randomised control trials have compared dCRT with either surgery alone or neo-adjuvant chemo-radiotherapy (CRT) followed by surgery for squamous cell carcinoma (SCC). None of these trials have demonstrated a significant difference in overall survival (OS) but were underpowered to detect non-inferiority of dCRT in comparison to surgery (11-13). There has not yet been a randomised trial conducted to compare dCRT with surgical treatment for oesophageal ACA and the role of dCRT in treating such tumours remains less well defined. The seminal RTOG 85-01 trial demonstrated a survival benefit in patients with the addition of cisplatin-based chemotherapy to radiation therapy (14). More recently the SCOPE 1 trial looked at the introduction of cetuximab to combination chemotherapy. This showed increased toxicity in the patients treated with the addition of cetuximab, with OS 22 months in patients treated with cetuximab and 25 months for those treated with concurrent chemo-radiotherapy alone (15).
The aim of this retrospective study was to determine factors affecting disease-free survival (DFS) and OS in patients undergoing dCRT and single modality radical radiotherapy for the treatment of OC with curative intent.
Materials and methods
Study design
This retrospective study included 235 consecutive patients diagnosed with potentially curable oesophageal carcinoma of any cell type who underwent definitive CRT or single modality radical radiotherapy between 1st January 2009 and 31st December 2012 inclusive. No patients underwent neo-adjuvant CRT. All patients were assessed by a regional multi-disciplinary team serving a population of 3.4 million and received treatment within Beatson West of Scotland Cancer Centre. All patients were treated by a clinical oncologist with special interest in upper GI malignancy.
Pre-operative staging involved computed tomography (CT), endoscopic ultrasound (EUS), positron emission tomography (PET) and laparoscopy where appropriate. All staging was in accordance with UICC tumour nodes metastases (TNM) 6th edition.
Data collected included patient age, gender, histological diagnosis, site of tumour, length of tumour on EUS, radiological stage, EUS stage, chemotherapy and radiotherapy toxicity, recurrence rates and OS. Primary endpoints were OS and DFS.
Definitive chemo-radiotherapy (dCRT)
A total of 190 patients were treated with dCRT and included those deemed unsuitable for surgical resection on the grounds of co-morbidity and/or performance status, locoregional disease considered inoperable or individual patient choice to have dCRT. Patients received up to four cycles of either cisplatin (75-80 mg/m2) and a fluoropyrimidine or mitomycin (12 mg/m2) and a fluoropyrimidine at the discretion of the treating clinician, with 1-2 cycles of induction chemotherapy followed by a further two cycles given concurrently with external beam radiotherapy. Concurrent radiotherapy regimes involved conformal or intensity modulated radiotherapy delivered in a single phase with three different dose-fractionations; 50 Gy in 25 fractions (n=137), 50.4 Gy in 28 fractions (n=46) and 54 Gy in 27 fractions (n=7). All patients without distant disease and adequate performance status (as assessed by MDT) were considered for dCRT. The radiotherapy planning target volume was defined using information for EUS, CT and PET imaging. This included all gross tumour volume plus a minimum of 1.5 cm circumferentially and 3 cm craniocaudally at the discretion of the treating clinical oncologist. Toxicity to oncological therapy was collated using the National Cancer Institute common criteria for adverse events (CTCAE v4.0). All patients receiving radiotherapy underwent CT planning and treated by either 3D conformal or intensity-modulated radiotherapy.
Single modality radical radiotherapy
Patients who were deemed either unsuitable for systemic chemotherapy on the grounds of medical co-morbidity, performance status or patient selection were considered for radical-dose single modality radiotherapy (n=45). Patients were staged in the same way as for dCRT and two different dose-fractionations were utilised; 55 Gy in 20 (n=38) fractions or 50 Gy in 25 fractions (n=7).
Follow-up and disease assessment
After completion of dCRT and single modality radical radiotherapy, planned follow-up included repeat endoscopy between 2-4 months. A total of 182 patients received endoscopy within this time frame, three patients underwent endoscopy at 6 months and 56 patients did not have further endoscopy either due to other evidence of metastatic disease before then or patient preference. Patients then had repeat endoscopy every 6 months for the first 3 years and then annually until 5 years. Patients underwent repeat CT 3 months following completion of treatment. A total of 217 patients underwent repeat CT imaging, 24 patients did not have further CT after treatment either due to co-morbidity of patient preference.
A total of 232 patients underwent clinical assessment between 6-12 weeks after dCRT and single modality radiotherapy, followed by every 3 months for the first 2 years then every 6 months thereafter until 5 years or death. The three patients who did not receive clinical assessment had died within 30 days of competing treatment.
Disease recurrence patterns were determined as loco-regional, distant metastatic or both. The time to recurrence was taken from the time of the confirmatory investigation. The patient cohort was analysed in May 2014, at which time median follow-up was 35.1 months (interquartile range, 29.5-40.6 months). Death certification was obtained from the Office for National Statistics.
Statistical analysis
Analysis was based on intention to treat. The primary end-point data were DFS and OS. Estimates of survival rates were expressed as percentages using the life-table Kaplan-Meier method with differences between groups analysed using Log Rank testing. Grouped data were expressed as a median and non-parametric testing was used. Disease-free and OS was measured from the date of completion of treatment to the date of recurrence. Final multivariate analysis included age, performance status, gender, tumour staging and histological subtype to correct for baseline differences between the groups.
All statistical analysis was done using IBM SPSS version 22.0.
Results
Patient characteristics
A total of 235 patients were included in the study (130 males and 105 females) and their details related to treatment modality are shown in Table 1. Of these patients, 91% were ECOG performance status 0-1 and 9% were ECOG performance status 2. A total of 190 patients were treated with dCRT and the remaining 45 patients were treated with single modality radiotherapy.
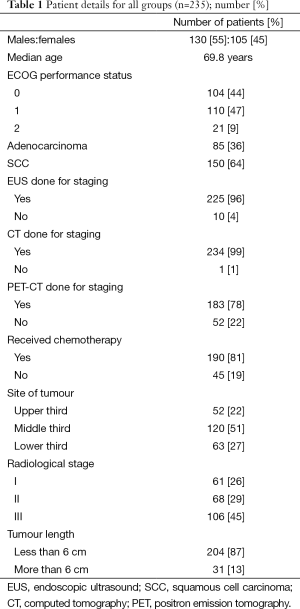
Full table
Compliance
The planned number of chemotherapy cycles for the dCRT group (n=190) was 4. A total of 138 patients (73%) completed four cycles with no chemotherapy dose alterations, 32 patients (17%) required dose reductions but completed four cycles of chemotherapy and 20 patients (10%) received three or less cycles of chemotherapy. A total of 233 patients completed planned radiotherapy treatment. One treatment was stopped early due to discovery of metastatic disease during treatment and one death during radiotherapy treatment. Both patients were in the radiotherapy only group.
Treatment-related morbidity
The overall rate of grade III or IV toxicity in the dCRT group (n=190) was 34% (64 patients) and 3.6% (7 patients) respectively. The rates of grade III or IV toxicity in the single modality radiotherapy group (n=45) were 29% (13 patients) and 7% (3 patients). The rates of nasogastric of PEG feeding in the whole population were 4% (9 patients); of which seven patients received dCRT and two patients received single modality radiotherapy.
There was one death during single modality radiotherapy group during therapy due to aspiration pneumonia. There were two deaths within 30 days of treatment, one in either group and both secondary to cerebro-vascular event.
DFS and OS
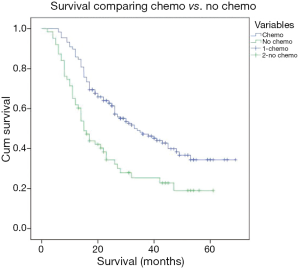
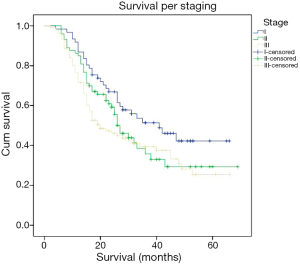
Patients who underwent dCRT had a significant improvement in median and DFS (31 vs. 16 months, P=0.02) and OS (37 vs. 25 months, P=0.01) compared to those undergoing single modality radiotherapy, demonstrated in Kaplan-Meier curve in Figure 1. The median stage for stage DFS for dCRT versus single modality radiotherapy were: stage I (40 vs. 30 months, P=0.09), stage II (36 vs. 22 months, P=0.06) and stage III (32 vs. 11 months, P=0.11), demonstrated in Kaplan-Meier curve in Figure 2. Patients with stage I/II disease had a significantly improved DFS (28 vs. 11 months) and OS (38.2 vs. 32 months) compared to those with stage III disease (P=0.013).
Subgroup analysis for histological subtype
All patients were further analysed for histological subtype irrespective of treatment received. A total of 150 patients (64%) had SCC and 85 patients (36%) had ACA as histological diagnosis. Stage for stage comparison of median OS for SCC was 37.9 and 32.8 months for ACA, P value 0.061. DFS was similar between both groups (28.6 months for SCC and 26.2 months for ACA, P value 0.057). There was a greater proportion of local recurrence in patients with SCC compared to ACA (54% vs. 49%, P=0.045), but a greater proportion of distant relapse in patients with ACA when compared to SCC (68% vs. 51%, P=0.039).
Subgroup analysis for completion of chemotherapy
Of the 190 patients treated with concurrent chemotherapy, there were 138 (73%) patients who completed all planned chemotherapy treatments, 32 (17%) patients who completed chemotherapy but required dose reductions and 20 (10%) patients who received three or less chemotherapy treatments. Stage for stage median OS was significantly improved for patients who completed chemotherapy versus those that did not (38 vs. 25 months, P=0.008).
Univariate and multivariate analysis
Univariate and multivariate statistical analysis revealed the factors adversely affecting DFS and OS were higher radiological staging in patients with stage III disease versus those with stage I/II disease (P=0.013) and patients who did not receive or complete chemotherapy (P=0.024 and P=0.008 respectively). Age, gender and tumour location were not significant factors. Histological subtype and EUS tumour length did not reach statistical significance.
Discussion
dCRT has emerged as an alternative treatment modality to surgery for locally advanced OC. Historical studies have demonstrated that advanced disease stage is an adverse prognostic factor. Recent advances in both local and distant staging with the increasing use of EUS and PET-CT have improved sensitivity for detection of occult nodal and distant metastatic disease as well as more precise definition of local tumour staging. This has enabled improved patient selection for curative treatment. In this study 78% of patients underwent CT-PET and 96% of patients had EUS performed.
This study demonstrates that dCRT was associated with improved rates of DFS (31 vs. 16 months respectively) and OS (27 vs. 25 months respectively) when compared to single modality radical radiotherapy, which concurs with historical clinical trial data (16-22). DFS (11 vs. 28 months respectively) and OS (32 vs. 38.2 months respectively) were also demonstrably improved in patients with stage I and II when compared to those with stage III disease. This again concurs with historical literature (Table 2), that patients with advanced stage disease have a poorer prognosis.
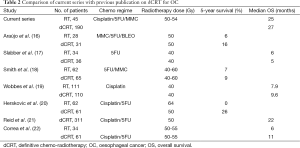
Full table
This study again reinforces the role of concurrent chemotherapy in addition to radical radiotherapy with demonstrable improvement in DFS and OS in patients who both had and completed concurrent chemotherapy with dCRT. The study showed a median OS for dCRT of 27 months which is similar to recently published studies although higher than historical case series. This may well reflect that there is an improvement in patient selection with the advent of modern staging modalities including CT-PET as well as technological advances in radiotherapy planning and delivery.
The rate of grade III and IV acute treatment-related toxicities were 34% and 3.6% respectively for dCRT compared to 29% and 7% respectively for single modality radiotherapy. The rates of NG/PEG feeding were low at 4% across the whole patient cohort. There were three deaths between starting and within 30 days of completion of treatment but none of these were attributed to be treatment-related toxicity
This study has several potential limitations. It was conducted as a non-randomised retrospective comparative analysis and is therefore potentially vulnerable to selection bias. There are, however many strengths to this study in that it represents a large series of consecutive patients over an abbreviated time frame assessed by an experienced multi-disciplinary team with the benefits of accurate modern radiological and clinical staging, particularly the increasing use of PET-CT and EUS. Patients were also treated using modern radiotherapy techniques, with CT planning and use of both conformal and intensity modulated radiotherapy planning techniques. There was good follow-up for patients within a well-defined geographical distribution and there were high rates of clinical, endoscopic and radiological follow-up to assess response.
Conclusions
This retrospective study again reinforces that dCRT is an effective and well-tolerated radical treatment for OC. Both DFS and OS rates were significantly improved when compared to previous data from this centre as well as historical case series. This may well reflect improved patient selection with modern clinical and radiological staging modalities. The rates of EUS were comparable with previous historical series, although the rates of CT-PET were higher than previous series which were conducted before CT-PET became standard of care for staging of oesophageal caner within the United Kingdom.
The study does highlight the importance of combined modality treatment in the form of concurrent chemo-radiotherapy. Patients treated with concurrent chemotherapy and who completed the planned treatment had a significantly improved overall and DFS when compared to those treated with single modality radiotherapy or in whom concurrent chemotherapy had to be stopped prematurely. This benefit clearly has to be balanced against clinical toxicity, but data from this study reflects a currently acceptable acute toxicity profile for patients undergoing dCRT. It is limited, however, by lack of long-term toxicity data.
This retrospective study adds further weight to current treatment paradigms emphasising the importance and safety of concurrent CRT in maximising curative potential for patients undergoing non-surgical treatment of OC. This study does demonstrate an acceptable acute toxicity profile throughout treatment but would benefit from further long-term follow-up data on late toxicities from dCRT.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cancer Research UK. Available online: http://www.cancerresearchuk.org/cancer-info/cancerstats/types/oesophagus/incidence/, accessed 13/12/2014.
- Cunningham D, Allum WH, Stenning SP, et al. Perioperative chemotherapy versus surgery alone for resectable gastroesophageal cancer. N Engl J Med 2006;355:11-20. [PubMed]
- Medical Research Council Oesophageal Cancer Working Group. Surgical resection with or without preoperative chemotherapy in oesophageal cancer: a randomised controlled trial. Lancet 2002;359:1727-33. [PubMed]
- National oesophago-gastric cancer audit 2014. NHS information Centre. Available online: http://www.hscic.gov.uk/catalogue/PUB16020/clin-audi-supp-prog-oeso-gast-2014-rep.pdf
- Sykes AJ, Burt PA, Slevin NJ, et al. Radical radiotherapy for carcinoma of the oesophagus: an effective alternative to surgery. Radiother Oncol 1998;48:15-21. [PubMed]
- Choi NC. Carcinoma of the oesophagus. In: Wang CC, editor. Clinical radiation oncology: indications, results. New York: Wiley-Liss, 2000:333.
- Earlam R, Cunha-Melo JR. Oesophogeal squamous cell carcinoms: II. A critical view of radiotherapy. Br J Surg 1980;67:457-61. [PubMed]
- Sun XD, Yu JM, Fan XL, et al. Randomized clinical study of surgery versus radiotherapy alone in the treatment of resectable esophageal cancer in the chest. Zhonghua Zhong Liu Za Zhi 2006;28:784-7. [PubMed]
- Walsh TN, Noonan N, Hollywood D, et al. A comparison of multimodal therapy and surgery for esophageal adenocarcinoma. N Engl J Med 1996;335:462-7. [PubMed]
- Tepper J, Krasna MJ, Niedzwiecki D, et al. Phase III trial of trimodality therapy with cisplatin, fluorouracil, radiotherapy, and surgery compared with surgery alone for esophageal cancer: CALGB 9781. J Clin Oncol 2008;26:1086-92. [PubMed]
- Chiu PW, Chan AC, Leung SF, et al. Multicenter prospective randomized trial comparing standard esophagectomy with chemoradiotherapy for treatment of squamous esophageal cancer: early results from the Chinese University Research Group for Esophageal Cancer (CURE). J Gastrointest Surg 2005;9:794-802. [PubMed]
- Bedenne L, Michel P, Bouché O, et al. Chemoradiation followed by surgery compared with chemoradiation alone in squamous cancer of the esophagus: FFCD 9102. J Clin Oncol 2007;25:1160-8. [PubMed]
- Stahl M, Stuschke M, Lehmann N, et al. Chemoradiation with and without surgery in patients with locally advanced squamous cell carcinoma of the esophagus. J Clin Oncol 2005;23:2310-7. [PubMed]
- Cooper JS, Guo MD, Herskovic A, et al. Chemoradiotherapy of locally advanced esophageal cancer: long-term follow-up of a prospective randomized trial (RTOG 85-01). Radiation Therapy Oncology Group. JAMA 1999;281:1623-7. [PubMed]
- Crosby T, Hurt CN, Falk S, et al. Chemoradiotherapy with or without cetuximab in patients with oesophageal cancer (SCOPE1): a multicentre, phase 2/3 randomised trial. Lancet Oncol 2013;14:627-37. [PubMed]
- Araújo CM, Souhami L, Gil RA, et al. A randomized trial comparing radiation therapy versus concomitant radiation therapy and chemotherapy in carcinoma of the thoracic esophagus. Cancer 1991;67:2258-61. [PubMed]
- Slabber CF, Nel JS, Schoeman L, et al. A randomized study of radiotherapy alone versus radiotherapy plus 5-fluorouracil and platinum in patients with inoperable, locally advanced squamous cancer of the esophagus. Am J Clin Oncol 1998;21:462-5. [PubMed]
- Smith TJ, Ryan LM, Douglass HO Jr, et al. Combined chemoradiotherapy vs. radiotherapy alone for early stage squamous cell carcinoma of the esophagus: a study of the Eastern Cooperative Oncology Group. Int J Radiat Oncol Biol Phys 1998;42:269-76. [PubMed]
- Wobbes T, Baron B, Paillot B, et al. Prospective randomised study of split-course radiotherapy versus cisplatin plus split-course radiotherapy in inoperable squamous cell carcinoma of the oesophagus. Eur J Cancer 2001;37:470-7. [PubMed]
- Herskovic A, Martz K, al-Sarraf M, et al. Combined chemotherapy and radiotherapy compared with radiotherapy alone in patients with cancer of the esophagus. N Engl J Med 1992;326:1593-8. [PubMed]
- Reid TD, Davies IL, Mason J, et al. Stage for stage comparison of recurrence patterns after definitive chemoradiotherapy or surgery for oesophageal carcinoma. Clin Oncol (R Coll Radiol) 2012;24:617-24. [PubMed]
- Correa PD. Chemoradiation for inoperable oesophageal cancer. Clin Oncol (R Coll Radiol) 2009;21:264.