Palliative stenting of the digestive tract: a case series of a single centre
Introduction
Obstruction of the gastrointestinal tract in patients with cancer occurs frequently and may be mechanical or functional, partial or complete, and may occur at one or at many sites (1,2). Tumours can impair bowel function in several ways: occlusion of the lumen, impairment of peristalsis due to tumour ingrowth, masses in the mesentery or omentum or adhesions creating an extra-luminal obstruction, and finally infiltration of the enteric nervous system causing dysmotility (3). Obstruction due to intra- or extra-luminal obstruction can be treated by endoscopic placement of metallic self-expandable stents.
Cancer in the oesophagus is frequently a late diagnosis with local and systemic metastases precluding resection. Most patients suffer from dysphagia, and palliative care is the only option. Colorectal cancer is occurring increasingly (4). Due to the use of swift diagnostic colonoscopy in case of complaints and screening many patients can be cured by surgical resection. However, there are still a certain number of patients presenting with metastases and incurable disease at the initial presentation. In these patients palliative therapy is the only option. Sometimes it is impossible to do a surgical resection of the primary tumour, mostly due to low Karnovski index and co-morbidity. In cases of bowel obstruction palliative stent placing can be an alternative for a deviating stoma.
Finally patients with distal gastric cancer, duodenal cancer or ingrowing pancreatic cancer presenting with obstruction, who are not fit for surgery can be helped with stenting.
The aim of the present study was to review the local experience in a single centre with endoscopic stenting of malignancies in the gastrointestinal tract.
Patients and methods
All patients treated with endoscopic stenting in a ten years period from 2001-2010 were studied.
In the first eight years self-expandable nitinol stents from Boston Scientific Nederland BV, Nieuwegein the Netherlands, were used. The final two years stents from Fujinon Endoscopy BV Veenendaal the Netherlands were used (Hanaro MI tech Ltd Seoul Korea).
In case of oesophageal stenting the partially covered Ultraflex™ nitinol stent with sutured loop ends was placed. This stent has a proximal flare of 23 mm to ensure fixation at the proximal edge of the tumour. The applied length varies according to the length of the obstruction (10-15 cm with a covered length of 7-12 cm). All patients received a stent with proximal release. In case of stenosis due to ingrowth of bronchial cancer uncovered stents with the same specifications were used. For duodenal and gastric stenting Wallflex™ stents were used. These nitinol stents are uncovered, have a body of 22 mm and a length of 9-12 cm, with a stent flare of 27 mm. These stents are placed through the working channel of the endoscope. In the case of colonic stenting Wallflex™ colonic stents were applied. The specifications are: body diameter 22-25 mm, flare of 27-30 mm and a length of 9-12 cm. These stents have a distal release.
The Hanaro™ stents for oesophageal stenting are fully covered with silicone. The stent length is 8-14 cm, diameter 20 mm, and the flare has a length of 10 mm. The enteral stents are uncovered with a diameter for duodenal stents of 18-24 mm with a length of 11 cm, while this is 22-28 mm and 8-11 cm for colonic stents respectively.
Endoscopy was done with endoscopes (gastroscopes and colonoscopes) of Olympus Zoetermeer The Netherlands (EVIS 100, EXERA 160 and 180).
All procedures were done with conscious sedation with midazolam 5 mg.
All stents were placed via guide-wires through the endoscope (in case of stomach, duodenal, or colon obstruction) or via guide-wires placed besides the endoscope through the tumour stenosis (oesophagus and rectum). Placement of the stent was done under fluoroscopic and endoscopic control. In case of oesophageal stent placement the proximal border of the tumour was marked with radio-opaque contrast via needle injection.
The patient preparation for oesophageal stent placement was acetaminophen 500 mg, for colon stenting a laxative enema.
Statistical analysis was done with chi-square test for contingency tables or t-test. A value below 0.05 was considered statistical significant.
Results
All patients receiving a self-expandable stent suffered from metastasised malignancies located in oesophagus, stomach, duodenum, or colon and rectum. All patients were or had been treated with palliative therapy in the form of chemotherapy.
Fifty one patients (37 men, 14 women, mean age 72 years, range, 48-91 years) received 57 stents because of oesophageal cancer. Mean survival after stent placement was 141 days, range, 1-589 days. All patients died due to their disease, with the exception of one. This patient received an oesophageal stent because of a perforation in the diagnostic work-up. He was treated with chemo-radiation and surgery and is currently still alive. One patient received 5 covered stents which dislocated four times due to a very short stenotic tract and the effect of palliative chemotherapy with tumour necrosis. One other patient had a dislocation of an uncovered stent in the proximal oesophagus and needed a new one. No case of perforation was seen. In nine cases (17%) (twice in one patient) clogging of the stent with food occurred. This was successfully solved by endoscopy. Tumour overgrowth was noted in four cases. No additional treatment was initiated in three cases because no important obstruction was noted; one patient needed a second stent.
Twenty four patients (13 men, 11 women, mean age 68 years, range, 42-86 years) received 28 stents in their colon or rectum. One patient had a very long stenotic segment (due to ovarian cancer) and received two stent placed longitudinally in one procedure. The stents were placed in the rectum (n=6), the sigmoid (n=14), the descending colon (n=1), and the transverse colon (n=3). All patients had a dominant stenosis with obstruction. Mean survival after stent placement was 276 days (range, 3-1,131 days). Perforation occurred in zero cases. Tumour in-growth occurred in two patients. One patient received a second stent; in the other patient this was not possible anymore. This patient was treated with a surgical stoma. Dislocation occurred in two cases during placement. The stent was repositioned in the same procedure. There were two cases of clogging (8%) by stool. This was solved by endoscopic rinsing of the stool.
Fourteen patients (5 men, 9 women, mean age 76 years, range, 37-92 years) received 18 stents because of obstructing stomach cancer. This was because of nine distal cancers and four cancer located in the gastric cardia. The latter received covered expandable stents, the remainder uncovered stents. There was one case of cancer in a Billroth II resection stomach. Mean survival after stent placement was 121 days (range, 30-335 days). There was no perforation, one case of clogging, and four cases of tumour ingrowth. Two patients got three stents each because of ingrowth. Two of them received no additional treatment. Their survival was 189 and 332 days respectively after placement of the first stent.
Eight patients (4 men, 4 women, mean age 63 years, range, 40-83 years) had stent placement in their duodenum. This was because of ingrowing pancreatic cancer in two cases, cancer of the distal bile duct in two, and obstructing duodenal cancer in four patients. Mean survival after stent placement was 84 days (range, 9-223 days). No perforation or clogging occurred. Three cases of tumour ingrowth were seen. The tumour ingrowth did not lead to significant new obstruction.
In addition, five patients got an oesophageal stent because of stenosis due to ingrowing bronchial cancer; one patient had stenosis in the course of breast cancer (3 men, 3 women, mean age 71 years, range, 57-86 years). These patients received an uncovered stent in order to prevent dislocation. One patient with bronchial cancer and treated with chemotherapy received three consecutive stents, each time due to tumour ingrowth. No further complications occurred. Mean survival after stent placement was 166 days, range, 6-430 days.
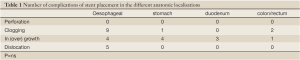
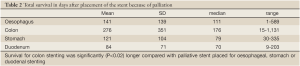
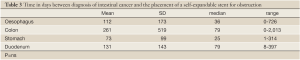
Table 1 shows the complications. There was no difference in occurrence of complication in different stents. Table 2 shows the survival of patients after stent placement. Patients with stenting because of colorectal cancer had a significantly longer survival. Table 3 shows the time between diagnosis and placement of a stent. There were no differences between the different types of cancer.
Full table
Full table
Full table
Discussion
Stent placing in the digestive tract can offer good palliation in patients with obstructing tumours unfit for surgery or in cases where surgery is not feasible anymore. The clinician must make individualised treatment choices in difficult clinical circumstances. There are many reports confirming efficacy. Covered and uncovered stents have different functional characteristics and the type of stent must be selected on an individual basis (5). In most cases technical and clinical success of oesophageal or gastroduodenal stenting is above 90% (6-8).
Modern self-expandable metal stents are easy to introduce and the complications of placement are very limited. The present series is the experience of stent placement in normal daily practice. Obviously all patient with cancer needed palliative therapy. By the placement of stents restoring passage of food or stool adequate palliation was given for the time being.
For cost benefit purposes stent placement should be considered if the life expectance of the patient is at least two months. Sometimes it is difficult to make a true estimate of life expectancy. This is illustrated by the range of survival after stent placement in the present group of patients. Some patients died within a very short time after stent placement. This was not procedure related, but due to the course of their complicated underlying disease. However, survival was more than two month in the majority of patients.
Self-expanding metal stent for the treatment of dysphagia is accepted and evidence based (9). With the exception of a few cases partially covered stents were used in case of oesophageal or cardia cancer. Hanaro stents are fully covered, including the proximal and distal flare and dislocation was observed using the stents (7,8). Reported complications after stent deployment include chest pain and heartburn. Upper gastrointestinal bleeding is very rare. Dysphagia scores improved significantly during follow-up after six months. Stent migration occurs with fully covered stents (10). The self-expandable stents may take about two to three days to reach their maximum diameter. This process can be painful. Patients were treated with effective painkillers before and four days after stent placement.
In one study 36 patients (43.4%) had recurrent dysphagia after stent placement, caused by tumour overgrowth in 32 cases (11). In the present study, tumour overgrowth only occurred in 8% of cases of oesophageal cancer. This low percentage possibly can be explained by the length of the used stent.
Song et al. did a study in order to evaluate predictive factors of food impaction in oesophageal stents. Food impaction occurred in 41 of 1,360 patients (3.0%). Multivariate analysis showed that stent length was an independent predictor of food impaction (12). Clogging due to food occurred in 17% in the present study, mostly in the first period of the study. This was the reason to adjust the dietary advices. Patients were advised to pureeing their food, also risotto rice and larger pieces of meat had to be omitted. This advice was followed very thoroughly by the patients thereafter. Food impaction can be managed by endoscopic or fluoroscopically guided removal or placement of a second stent.
Placing a stent across the obstructing tumour permits unrestricted access of stomach contents to the oesophagus. This iatrogenic reflux has to be treated with proton pump inhibitors. Overall, all patients had good palliation for their remaining life span.
Placement of stents in the oesophagus is an easy procedure. However, there are some differences in placement technique between the available stents. The endoscopist should be aware of these differences. The Ultraflex™ has a both a proximal or distal release system. In the present study only stents with a proximal release were placed. During release the stent should be pushed inwards into the oesophagus in order to prevent dislocation. The Hanaro™ stent only has a distal release; hence during release of the endoprosthesis the stent has to be pulled in order to prevent dislocation into the stomach. One major lesson learnt is that a fully covered Hanaro™ stent is not the best option for placement over a short tight stenosis. In one patient this stent dislocated four times. Whether this was due to tumour necrosis as a result of chemotherapy or because of the fact that the stent did not adhere tightly anymore to the oesophageal mucosa is unsure. In cases where the Ultraflex™ stent was placed this did not happen.
Mean survival in the literature after stent placement was 146.3±143.6 days (range, 13-680 days) (10). The mean survival in the presented patients, 141 days, is in accordance with this report.
Patients with ingrowing bronchial cancer in the oesophagus received an uncovered stent because the common belief is that a covered stent can dislocate easily in these cases. The price to pay is tumour ingrowth, as was the case in one patient. However, new stents could be placed without major problems.
The aim in palliating patients with malignant gastric outlet obstruction is to re-establish an oral intake by restoring gastrointestinal continuity. This ultimately improves the quality of life in the advanced stages of cancer. Endoscopic stenting is preferable to operative gastrojejunostomy in terms of faster return to fluids and solids, and reduced morbidity for patients with a limited life span. The main drawback to operative bypass is the high incidence of delayed gastric emptying, particularly in this group of patients with symptomatic obstruction (13). Malignant gastric outlet obstruction represents often the terminal stage in pancreatic cancer. Between 5% and 25% of patients with pancreatic cancer ultimately experience malignant gastric outlet obstruction. In the present study 22 patients received gastric or duodenal stents. Uncovered stents are used because they adhere better to the mucosa. Unfortunately common duodenal stent-related complications are a recurrence of symptoms due to stent clogging (tissue ingrowth/overgrowth and food impaction) and stent migration. Stent dysfunction is reported in up to 25% of patients (14). Complications are ingrowth or overgrowth of tumours in 12%, bleeding in 3%, stent migration in 1.5%, and perforation in 0.5% (15). In the present study only tumour ingrowth and/or overgrowth was seen in 7 patients. These complications can be usually managed endoscopically, thereby restoring food passage (16).
In a paper by Lee et al. it was reported that there was no difference in major complications between stent placement versus surgery in cases of palliation for colon cancer. The patients treated with stenting had fewer early complications which is understandable since laparotomy is not required (17). Stent placement in the colon has its complications, perforation in 9%, migration in 5%, and occlusion in 9% (18). Placement of a stent in the colon gives good and adequate palliation given the fact that all patients in the present study had passage of stool and were treated effectively for the obstruction. Clogging due to faecal impaction only occurred in two cases. This low percentage can be explained by the standard use of stool softeners and laxatives. No single case of perforation occurred. This is in contradiction with the literature. Especially in cases of colon stent placement perforations are reported (19). Of course this complication is a worst case scenario because the patient was already unfit for surgery. Happily this never occurred. The possible explanation for the perforations in the literature are the fact that stent placement was used as a bridge to surgery in patients presenting with acute bowel obstruction with pre-stenotic dilatation. In the present series all patient receiving a colon stent did not have an acute bowel obstruction. Their presentation was more chronic intermittent obstruction without pre-stenotic dilatation. In addition, the majority also suffered from malignant peritonitis. The through the scope application for enteral stents makes the procedure easier and faster (20).
The survival of patients after stenting of the colon is relatively long. This is probably not the result of the stent, but the result of palliative treatment with chemotherapy in all cases. Especially in colorectal cancer with metastases chemotherapy significantly prolonged life. Placement of colon stents contributes to this survival. Stent placement is less costly and has fewer complications on the long-term compared with a colostomy (21).
From the present series it can be concluded that placement of expandable stents in the digestive tract in normal daily practice is feasible, safe, with a low number of complications, and provides adequate palliation in the majority of patients for the given life span.
Acknowledgements
Disclosure : The authors declare no conflict of interest.
References
- Pameijer CR, Mahvi DM, Stewart JA, et al. Bowel obstruction in patients with metastatic cancer: does intervention influence outcome? Int J Gastrointest Cancer 2005;35:127-33.
- Laval G, Arvieux C, Stefani L, et al. Protocol for the treatment of malignant inoperable bowel obstruction: a prospective study of 80 cases at Grenoble University Hospital Center. J Pain Symptom Manage 2006;31:502-12.
- Rousseau P. Management of malignant bowel obstruction in advanced cancer: a brief review. J Palliat Med 1998;1:65-72.
- Dutch Cancer registration. Available online: www.cijfersoverkanker.nl
- Vlavianos P, Zabron A. Clinical outcomes, quality of life, advantages and disadvantages of metal stent placement in the upper gastrointestinal tract. Curr Opin Support Palliat Care 2012;6:27-32.
- Sgourakis G, Gockel I, Radtke A, et al. The use of self-expanding stents in esophageal and gastroesophageal junction cancer palliation: a meta-analysis and meta-regression analysis of outcomes. Dig Dis Sci 2010;55:3018-30.
- Hirdes MM, Siersema PD, Vleggaar FP. A new fully covered metal stent for the treatment of benign and malignant dysphagia: a prospective follow-up study. Gastrointest Endosc 2012;75:712-8.
- van Heel NC, Haringsma J, Boot H, et al. Comparison of 2 expandable stents for malignant esophageal disease: a randomized controlled trial. Gastrointest Endosc 2012;76:52-8.
- Baron TH. Expandable metal stents for the treatment of cancerous obstruction of the gastrointestinal tract. N Engl J Med 2001;344:1681-7.
- Talreja JP, Eloubeidi MA, Sauer BG, et al. Fully covered removable nitinol self-expandable metal stents (SEMS) in malignant strictures of the esophagus: a multicenter analysis. Surg Endosc 2012;26:1664-9.
- Lazaraki G, Katsinelos P, Nakos A, et al. Malignant esophageal dysphagia palliation using insertion of a covered Ultraflex stent without fluoroscopy: a prospective observational study. Surg Endosc 2011;25:628-35.
- Song M, Song HY, Kim JH, et al. Food impaction after expandable metal stent placement: experience in 1,360 patients with esophageal and upper gastrointestinal tract obstruction. J Vasc Interv Radiol 2011;22:1293-9.
- Chandrasegaram MD, Eslick GD, Mansfield CO, et al. Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction. Surg Endosc 2012;26:323-9.
- van Hooft JE, van Montfoort ML, Jeurnink SM, et al. Safety and efficacy of a new non-foreshortening nitinol stent in malignant gastric outlet obstruction (DUONITI study): a prospective, multicenter study. Endoscopy 2011;43:671-5.
- Costamagna G, Tringali A, Spicak J, et al. Treatment of malignant gastroduodenal obstruction with a nitinol self-expanding metal stent: an international prospective multicentre registry. Dig Liver Dis 2012;44:37-43.
- Boškoski I, Tringali A, Familiari P, et al. Self-expandable metallic stents for malignant gastric outlet obstruction. Adv Ther 2010;27:691-703.
- Lee HJ, Hong SP, Cheon JH, et al. Long-term outcome of palliative therapy for malignant colorectal obstruction in patients with unresectable metastatic colorectal cancers: endoscopic stenting versus surgery. Gastrointest Endosc 2011;73:535-42.
- Small AJ, Coelho-Prabhu N, Baron TH. Endoscopic placement of self-expandable metal stents for malignant colonic obstruction: long-term outcomes and complication factors. Gastrointest Endosc 2010;71:560-72.
- van Hooft JE, Fockens P, Marinelli AW, et al. Early closure of a multicentre randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy 2008;40:184-91.
- Feo L, Schaffzin DM. Colonic stents: the modern treatment of colonic obstruction. Adv Ther 2011;28:73-86.
- Varadarajulu S, Roy A, Lopes T, et al. Endoscopic stenting versus surgical colostomy for the management of malignant colonic obstruction: comparison of hospital costs and clinical outcomes. Surg Endosc 2011;25:2203-9.


