Outcome of rectal cancer after radiotherapy with a long or short waiting period before surgery, a descriptive clinical study
Introduction
Rectal cancer is one of the most prevalent cancers in the gastrointestinal tract (1). The only curative treatment option is surgery. In the past, local recurrence was a major problem. (Neo)-adjuvant radiotherapy in combination with conventional surgery, has shown to improve local control and survival. The Dutch Total Mesorectal Excision (TME) trial investigated the value of radiotherapy in combination with surgery. The local recurrence risk almost halved after six years of follow-up. However, an effect on overall survival could not be demonstrated (2-4).
There are two frequently applied schedules of neo-adjuvant (chemo)radiation. The first one is radiotherapy 5 times 5 Gy followed by immediate surgery, the second one is radiotherapy in combination with chemotherapy followed by a longer waiting period before the actual surgical resection. According to the literature there is no difference in outcome with respect to overall survival, recurrence free survival and local recurrences between both schedules (5,6).
However, patients reported in the literature are not representative of the population seen in daily practice. In trials strict inclusion and exclusion criteria are used. In the studies by Peeters and Sebag-Montefiore median ages were comparable to the one in a cohort in our clinic (7). However, 99% of patients in the study by Sebag-Montefiore had a WHO performance score of 1 or higher indicating that a group of patients with more co-morbidity has been excluded. Unfortunately functional status of patients in this cohort has not been documented (3,4).
In daily practice doctors are confronted with patients fulfilling many or all exclusion criteria applied in clinical trials. Hence, data from the literature cannot always be extrapolated to daily practice.
For this reason, a study was done in usual daily practice in a group of consecutive patients with rectal cancer in order to gather data on survival and recurrences and to correlate these to the kind of radiotherapy that was given.
Methods
All consecutive patients diagnosed with rectal cancer in the period 2002-2008 were included in the present study. This period was chosen in order to obtain adequate follow-up data of all patients. An extensive search was done of clinical records in order to evaluate the clinical course of the patients.
For all patients, treatment was determined, in addition, data were gathered on survival, stage of the tumour, co-morbidity according to the well-known Charlson score, and cause of death.
It was determined whether death was the result of the rectal cancer itself, the complication of the treatment, or not related to rectal cancer at all (death due to co-morbidity, this is non-cancer related causes).
Evaluation was done in January 2014. Hence, follow-up was longer than 5 years in all patients.
The patients were divided in three groups: group 1 patients undergoing surgery without neo-adjuvant radiotherapy; group 2 patients undergoing 5×5 Gy radiotherapy followed by immediate surgery (short course, within 4 weeks after radiation); and group 3 patients treated with (chemo) radiotherapy followed by a longer waiting period (long course) before actual surgery. The decision to choose for the short or the long course was made in a multi-disciplinary meeting and was based on clinical judgment and imaging of tumour extension, N-stage and the intention to downsize the tumour in the long course. Patients who did not undergo surgery, obviously, were excluded
Statistical analysis was done with chi-square test for contingency tables and t-test. A value below 0.05 was considered significant.
Results
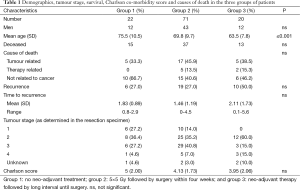
In the period of 7 years a total of 143 patients was diagnosed and treated for rectal cancer. Of these, 113 underwent surgery. This is the group analysed in this study. Twenty two patients (12 men, 10 women) underwent surgery without neo-adjuvant radiotherapy (group 1). Ninety one patients (55 men, 36 women) were treated with neo-adjuvant radiotherapy; 71 patients in the short course (group 2), and 20 in the long course schedule (group 3).
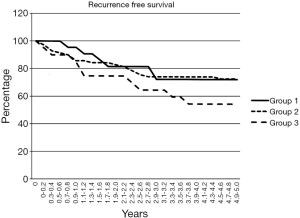
Table 1 shows the results in the three groups of patients. There was no difference in gender. Mean age in patients of group 3 was significantly lower than in groups 1 and 2 (P=0.02). There was no significant difference in cause of death between the three groups. Recurrence of disease occurred in all three groups without any difference. Figure 1 shows the recurrence free period graphically. There was no significant difference in time to recurrence. There was a trend towards a lower tumour stage in the patients of group 3, implying successful down-staging of the tumour. There was no difference in co-morbidity score.
Full table
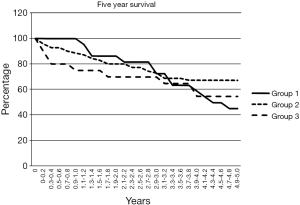
Figure 2 shows the five year survival. There was no significant difference between the three groups. Overall five year survival was 32% in group 1, 48% in group 2, and 35% in group 3.
Discussion
Treatment decisions have to be made by clinicians relying on data from the literature that cannot always be strictly applied to their patients. Hence, in daily practice, sometimes decisions have to be made that contradict the guidelines from the literature. So, our study population represents daily practice and the outcome data are comparable to those of selected patients included in randomised controlled trials. All patients treated for rectal cancer, in the time period of this study, were discussed in a multi-disciplinary meeting with oncologists, gastroenterologists, radiologists, radiotherapists and surgeons. On the basis of the clinical and radiological presentation, and data from the literature, a therapeutic regimen was chosen. In the study period neo-adjuvant radiotherapy was applied in all patients with a T3 stage and judged fit enough to undergo the treatment. In the final years of the study period chemo-radiation was also applied in some patients on basis of the N-stage. In that aspect this study presents unique data, since there is also a group of patients not been treated with neo-adjuvant therapy. The five year survival was much lower than reported in the literature. Presence of co-morbidity is an important factor in mortality. These patients usually do not participate in clinical trials, simply because of their co-morbidity. There was no difference in the three groups with respect to overall survival. Also there was no difference with respect to recurrent disease. An important observation is the fact that many patients do not die because of cancer but because of non-cancer related causes. This reduces the effect of treatment on overall survival. This is important when discussing survival after treatment of cancer. The majority of the patients in our study were older with a limited life expectancy. The patients in the three groups are comparable with respect to gender and co-morbidity score.
At a first glance, there is no benefit between surgery with or without neo-adjuvant radiotherapy. Indeed, survival and recurrence rate was the same for all three groups. However, these results can also be interpreted differently. Patients receiving neo-adjuvant radiotherapy had a higher clinical stage at presentation. Despite this the results of treatment were the same as in patients with a low stage of disease, possibly because of the effect of radiotherapy. It could be speculated that if the patients in groups 2 and 3 did not undergo neo-adjuvant therapy the survival would have been worse.
Short-term 5×5 Gy radiotherapy has become a popular preoperative treatment for patients with resectable rectal cancer in the Netherlands. An older study clearly demonstrated improved overall survival with radiotherapy. This study used radiotherapy followed by surgery within one week. The overall five-year survival rate was 58 percent in the radiotherapy-plus-surgery group and 48 percent in the surgery-alone group (P=0.004) (8,9).
The intention to down stage the tumour was the argument for a longer waiting period after radiation. According to a meta-analysis, short course radiotherapy with immediate surgery is as effective as long-course chemo-radiotherapy with delayed surgery for the treatment of rectal cancer in terms of overall survival, disease free survival, local recurrence rate, and distant metastases (5,6). Down-staging the tumour is the purpose of radiotherapy. Foster et al. did a literature review. They found limited evidence to support decisions regarding when to resect rectal cancer following chemo-radiotherapy. There may be benefits in prolonging the interval between chemo-radiotherapy and surgery beyond the 6 to 8 weeks that is commonly practiced (10). However, there are also data which do not show any down-staging. Sirohi et al. did a retrospective analysis in 110 patients and concluded that timing of surgery, a longer time interval, did not influence pathological response (11). In a study by Perez et al. it was shown that increased uptake of FDG during PET-scan was a sign of absence of down-staging (12). In the present study there was a trend towards successful down-staging after a longer waiting period. This did not reach statistical significance probably due to the low number of patients in this group.
The final conclusion of the present study is that neo-adjuvant radiotherapy seems to be of benefit in daily practice in selected patients with rectal cancer. Co-morbidity score is not of influence on the outcome. A longer waiting period after radiation therapy results in successful down-staging as expressed by the lower Dukes stage of the resected specimen. In addition, clinicians have to be aware that many patients will die due to other causes than those related to the rectal cancer itself, irrespective of the outcome of rectal cancer treatment.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Integraal kanker centrum Nederland. 2014. Available online: www.cijfersoverkanker.nl
- Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 2001;358:1291-304. [Crossref] [PubMed]
- Peeters KC, Marijnen CA, Nagtegaal ID, et al. The TME trial after a median follow-up of 6 years: increased local control but no survival benefit in irradiated patients with resectable rectal carcinoma. Ann Surg 2007;246:693-701. [Crossref] [PubMed]
- Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 2009;373:821-8. [Crossref] [PubMed]
- Zhou ZR, Liu SX, Zhang TS, et al. Short-course preoperative radiotherapy with immediate surgery versus long-course chemoradiation with delayed surgery in the treatment of rectal cancer: a systematic review and meta-analysis. Surg Oncol 2014;23:211-21. [Crossref] [PubMed]
- Sajid MS, Siddiqui MR, Kianifard B, et al. Short-course versus long-course neoadjuvant radiotherapy for lower rectal cancer: a systematic review. Ir J Med Sci 2010;179:165-71. [Crossref] [PubMed]
- van Eeghen EE, Bakker SD, van Bochove A, et al. Impact of age and comorbidity on survival in colorectal cancer. J Gastrointest Oncol 2015;6:605-12. [PubMed]
- Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med 1997;336:980-7. [Crossref] [PubMed]
- Folkesson J, Birgisson H, Pahlman L, et al. Swedish Rectal Cancer Trial: long lasting benefits from radiotherapy on survival and local recurrence rate. J Clin Oncol 2005;23:5644-50. [Crossref] [PubMed]
- Foster JD, Jones EL, Falk S, et al. Timing of surgery after long-course neoadjuvant chemoradiotherapy for rectal cancer: a systematic review of the literature. Dis Colon Rectum 2013;56:921-30. [Crossref] [PubMed]
- Sirohi B, Barreto SG, Patkar S, et al. Down-staging following neoadjuvant chemo-radiotherapy for locally advanced rectal cancer: Does timing of surgery really matter? Indian J Med Paediatr Oncol 2014;35:263-6. [Crossref] [PubMed]
- Perez RO, Habr-Gama A, São Julião GP, et al. Optimal timing for assessment of tumor response to neoadjuvant chemoradiation in patients with rectal cancer: do all patients benefit from waiting longer than 6 weeks? Int J Radiat Oncol Biol Phys 2012;84:1159-65. [Crossref] [PubMed]