
Suppression effect and safety of acupuncture on colonic spasm during colonoscopy: a randomized controlled trial
Introduction
Colonoscopy is currently the main method for diagnosing colorectal diseases. It is widely used in the diagnosis and treatment of colorectal polyps and other diseases. High-quality colonoscopy is helpful for early detection and increases the detection rate of polyps and other diseases during colonoscopy. Regular inspections can effectively prevent colorectal cancer. At present, the procedure of painless colonoscopy in China is comfortable for patients and the operating environment is good, which has led to the extensive application of colonoscopy. However, many factors continue to interfere with the endoscopic procedure, including anatomical abnormalities, colonic spasms, and contractions, and a lack of experienced endoscopists, and poor cooperation by nurses (1). The question of how to improve the quality of painless colonoscopy operations has become a new focus of attention. In clinical practice, intestinal spasms and hyperperistalsis often occur during endoscopic procedures, which increases the difficulty of inserting the endoscope and tends to impede observation, resulting in an increase in the missed detection rate for colon lesions and delays in inspection times. Strong spasms and contractions of the colon are thought to be due to insufficient anesthesia and lead to increase usage of cannabis drugs (2,3). The premeditation of anesthetic, atropine, scopolamine, and other drugs can suppress intestinal spasms and hypermotility (2,3); however, the use of these antispasmodic agents is limited in long-term examinations and treatments, as their repeated administration can cause side effects, such as dry mouth, flatulence, and abdominal pain after the examination.
Previous studies have confirmed that acupuncture has a significant effect on regulating abnormal gastrointestinal motility and is a cost-effective and safe therapy (4,5). Although an increasing number of randomized controlled trials report the efficacy of acupuncture for gastrointestinal disorders, especially for irritable bowel syndrome (IBS), of which pathophysiology shows gastrointestinal motility dysfunctions (5). There is no study using acupuncture for intestinal spasms in the process of colonoscopy. Our small-scale observations (30 patients) show that acupuncture can prolong the duration of muscle contraction of the bowel wall (before acupuncture vs. after acupuncture: 2.50 vs. 9.77 s), indicating the potentially effective suppression effect of acupuncture. Hence, we sought to objectively evaluate the effect and safety of acupuncture on inhibiting intestinal spasms and contractions in patients undergoing painless colonoscopies to provide a safer and simpler alternative in clinical practice. We present the following article in accordance with the CONSORT reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-407/rc).
Methods
Study design
This prospective, randomized, single-blinded, controlled trial was conducted at the Digestive Endoscopy Center of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine. Eligible patients were randomly assigned to the acupuncture group or sham control group at a 1:1 ratio. The study was reviewed and approved by the Ethics Committee of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine (No. YF2020-150-01). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Participants
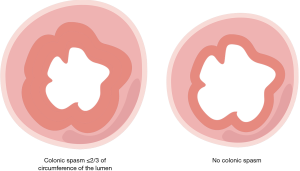
Patients were registered for colonoscopy from August 2020 to January 2021. To be eligible for inclusion in this study, patients had to meet the following inclusion criteria: (I) experience a colonic spasm during colonoscopy. A colonic spasm was defined as an opening to the colonic lumen >2/3 of the maximum diameter of the lumen (3); (II) be aged 18–70 years old; and (III) provide written informed consent before study participation. Patients were excluded from the study if they met any of the following exclusion criteria: (I) were a psychiatric patient, or could not cooperate with treatment; (II) had poor bowel preparation [i.e., a Boston bowel preparation scale (BBPS) score ≤3 points]; (III) experienced shock; (IV) had acute gastrointestinal bleeding, severe anemia (Hb 60 g/L), a bleeding tendency, or coagulation dysfunction; (V) had severe intestinal stenosis, or an obstruction; (VI) had constipation-predominant pattern irritable bowel syndrome, inflammatory bowel disease, or chronic constipation; and/or (VII) had used gastrointestinal antispasmodic drugs before or during the colonoscopy. Patients were withdrawn from the study if they met any of the following withdrawal criteria: (I) had incomplete case data; (II) had an unstable heart rate, blood oxygen saturation, or blood pressure during acupuncture; and/or (III) displayed voluntary actions during acupuncture.
Randomization and masking
Allocation was conducted by researchers using a simple random method with a random number table. Eligible patients were randomly assigned to the acupuncture group (n=27) or sham control group (n=27) using sequentially numbered containers that were implemented by the acupuncturist. Both the endoscopists and patients (who were placed under general anesthesia) were blinded to the acupuncture therapy. The acupuncturist was not masked to the allocation or therapy.
Procedures
Patients strictly followed a low-fire diet, and received standard bowel cleansing and an endoscopy by experienced endoscopists (who had completed >1,000 colonoscopies). No anticholinergic agents were used. Propofol was administrated during the painless colonoscopy. The BBPS was used to evaluate the quality of intestinal preparation. Carbon dioxide was used for insufflation. An endoscopist performed the colonoscopy operation, and an acupuncturist performed the acupuncture operation. Patients’ vital signs were strictly monitored during the procedure and essential measures were taken if these became unstable. When intestinal spasms or contractions occurred during the procedure, the patient undergoing the operation was randomly allocated to the acupuncture group or the sham control group. Colonic spasm was defined as spasm <2/3 of the circumference of the lumen (3) (see Figure 1).
Acupuncture group: In this study, the bilateral Hegu (LI 4) and Neiguan (PC 6) points were chosen as acupoint locations, and the acupuncture depth referred to “Acupuncture and Moxibustion” (6) (see Figure 2). After disinfecting the skin of the acupoint area with Aner’s iodine, a trained acupuncturist held sterile and disposable acupuncture needles [length: 25–40 mm; diameter: 0.25 mm (Hwatuo)], pierced the needles straight at 90°, and inserted the needles at a depth of 0.5–1 cm. To achieve the de qi sensation, the needles were twirled and rotated at each acupoint for about 15 seconds; the needle placement duration lasted until the end of the colonoscopy operation.
Sham control group: The location of the sham acupoints were 1 cm above the proximal end of the bilateral Hegu (LI 4) and Neiguan (PC 6) points, which have no known function (see Figure 3). The manipulation of needling was consistent with that of the experimental group.
When the manipulation to achieve de qi finished, a doctor observed and recorded the latency time to and the duration of colonic spasm suppression. If an intestinal spasm repeated within 5 minutes of the acupuncture, and the degree was greater than that before acupuncture, it was defined as a rebound of intestinal spasm (3,7). Adverse cases were defined as acupuncture-related side effects such as pain, wound redness and swelling, sticking of needle, bending of needle and breaking of inserted needle. Any occasion above would be recorded if occurred during the procedure.
Outcome measures
The primary outcome was the latency time to colonic spasm suppression, which was defined as the latency time between the accomplishment of twirling and rotating at the acupoints and the initiation of colonic spasm suppression. The secondary outcomes were the duration of colonic spasm suppression, and the proportion of patients who experienced rebound spasms, and adverse events.
Sample size calculation
Assuming that the effect of acupuncture of the bilateral Hegu (LI 4) and Neiguan (PC 6) points was close to that of lidocaine in inhibiting intestinal spasms, we estimated the sample size by referring to the article entitled, “Topical Lidocaine Inhibits Spasm During Colonoscopy: A Double-Blind, Randomized Controlled Trial (with video)” (2). In this study, we assumed that the average time spent in suppressing colonic spasm in the acupuncture group was 240 seconds, the standard deviation (SD) was 90 seconds, and the average latency time to colonic spasm suppression in the control group was at least 80 seconds different to that of the treatment group. The α error was 0.05 (2-sided), and β was 0.10. Using SPSS (version 26.0, IBM, Armonk, NY, USA) we calculated the sample size of the 2 groups as N1=N2=27 cases. Thus, 27 cases were included in each of the 2 groups in this study.
Statistical analysis
The continuous variables were measured using the mean and SD () or using the median with the interquartile range (IQR). The categorical variables were measured using frequencies (%). For the normally distributed continuous variables, comparisons were made using 2 independent samples t-tests. For the abnormally distributed continuous variables, comparisons were made using Mann-Whitney U-tests. The categorical data were compared using the chi-square test or Fisher’s exact test as appropriate. A probability (P) value <0.05 was considered statistically significant. SPSS (version 26.0, IBM, Armonk, NY, USA) was used for the data analysis. In this study, the proportion of sex in the 2 groups was tested by a chi-square test, the proportion of age was tested by a t-test, the number of colonoscopies in the past and the reasons for the colonoscopies were tested by a Fisher’s exact test, and BBPS scores were tested by a rank-sum test.
Results
Patients
From August 2020 to January 2021, a total of 54 patients were enrolled and ultimately included in this study (see Figure 4). The patients were randomly allocated to either the acupuncture group (n=27) or the sham control group (n=27). The general baseline data of patients were collected, including data on their age, gender, number of past colonoscopies, reasons for colonoscopies, and the quality of bowel preparation (BBPS). There were no significant differences in the baseline data between the 2 groups (P>0.05), which ensured comparability (see Table 1). All 54 colonoscopies were completed.
Table 1
| Characteristics | Acupuncture group (n=27) | Sham control group (n=27) | P value |
|---|---|---|---|
| Gender (male, %) | 12 (44.44) | 10 (37.04) | 0.580 |
| Age (years, ) | 49.44±10.31 | 48.96±9.98 | 0.862 |
| The number of past colonoscopy examinations (times, %) | 0.267 | ||
| 0 times | 17 (63.0) | 11 (40.7) | |
| 1–2 times | 8 (29.6) | 13 (48.1) | |
| ≥3 times | 2 (7.4) | 3 (11.1) | |
| Reasons for colonoscopy (n, %) | 0.185 | ||
| Abdominal discomfort, such as abdominal pain | 14 (51.9) | 8 (29.6) | |
| Physical examination or re-examination after intestinal polyp treatment | 11 (40.7) | 13 (48.1) | |
| Fecal stool occult blood test (+) or hematochezia | 0 (0.0) | 3 (11.1) | |
| Other reasons | 2 (7.4) | 3 (11.1) | |
| BBPS score [M (P25, P75), points] | 6.00 (4.50, 6.50) | 6.00 (5.00, 7.00) | 0.261 |
BBPS, Boston bowel preparation scale; M, median.
Primary outcome
The latency time to colonic spasm suppression of the acupuncture group was significantly shorter than tha6 of the sham control group (acupuncture: 32.00 s vs. sham: 82.00 s; P<0.001, rank-sum test; see Figure 5).
Secondary outcomes
There was no statistically significant difference in the duration of colonic spasm suppression between the 2 groups; however, the duration was generally longer in the acupuncture group (acupuncture: 300 s vs. sham: 268 s; P=0.142, rank-sum test; see Figure 6). No rebound spasms were observed in the acupuncture group but rebound spasms were observed in 3 patients in the sham control group. However, no statistically significant difference was observed between the 2 groups (acupuncture: 0% vs. sham: 11.1%; P=0.236, Fisher's exact test; see Figure 7).
Adverse events
No adverse events were observed in the acupuncture group or the sham control group during or after the process of the acupuncture operation.
Discussion
In this prospective, single-blinded, randomized controlled trial, we found that the latency time to colonic spasm suppression differed significantly between the acupuncture and sham acupuncture groups (acupuncture: 32.00 s vs. sham: 82.00 s; P<0.001), which indicated that acupuncture had an immediate effect on inhibiting intestinal spasms. In clinical practice, the instantaneous occurrence of colonic spasm narrows the intestinal cavity, which often increases the difficulty for endoscopists, especially beginners. Since the usage of anesthesia is strictly controlled, it is necessary to quickly restore the environment of the intestinal cavity to enable the colonoscope to pass smoothly. In this study, we confirmed that acupuncture had a rapid effect on the relaxation of intestinal spasms during colonoscopy, and saved time and reduced the difficulty of the endoscopic procedure.
Previous studies have confirmed that acupuncture can regulate visceral motor functions (including hypomotility or hyperkinesia) and has a rapid effect in the treatment of functional gastrointestinal diseases (e.g., functional dyspepsia, and irritable bowel syndrome) (8-10). According to traditional Chinese medicine “acupuncture can adjust the balance of yin and yang” (11). Previous studies have found that the effect of acupuncture on regulating gastrointestinal motility is also reflected in a 2-way adjustment effect whereby the direction of the acupuncture effect is mainly determined by the body’s functional state (12-14). As an external stimulation therapy, acupuncture mainly triggers a series of reactions by stimulating the nerve endings under the acupoints and producing short-acting effects. A study showed that electroacupuncture at Zusanli (ST 36) promotes gastric motility in anesthetized animals within 30–120 seconds (15).
After acupuncture at acupoints on the body surface, signals are generated from the peripheral nerves and transmitted to the central nervous system in an orderly and rapid manner. The central system also synthesizes the information of organs, quickly makes adjustments, and feeds back a series of neurotransmitters to the peripheral nerves at all levels, thereby generating a corresponding acupuncture effect (16). Research has shown that acupuncture regulates gastrointestinal motility via a multi-level, multi-system, and has multi-target coordination effects on the nervous system, gastrointestinal peptides, intestinal microbes, gastrointestinal smooth muscle, and signaling pathways, and achieves bidirectional regulation, which is called the "neuro-humoral-immunological modulation" (17,18,19). This may be one of the possible mechanisms by which acupuncture at the Hegu (LI 4) and Neiguan (PC 6) points inhibited intestinal motility in this study.
The function of regulating gastrointestinal motility is related to the specificity of the selected acupoints. According to traditional Chinese medicine, “the meridian goes through, the main treatment is” (i.e., acupoints regulates the meridian qi and have far-reaching effects on the meridian diseases at which the acupoints are located). The effects of stimulating the acupoints on the meridian at which a disease is located is better than stimulating the acupoints that do not belong to the meridian or the non-acupoints on the meridian at which a disease is located. Currently, acupoints are thought to be distinct from non-acupoints or other acupoints in terms of their morphology, biophysics, pathological responses, and stimulus effects, and their acupuncture effects also differ.
Hegu (LI 4) belongs to the original point of the large intestine meridian, which is the mark, and it has the effect of relaxing the tendons of the large intestine (20). Thus, it can overcome the spasm and contraction of the large intestine. Hegu (LI 4) is a sensitive stimulation point, which can adjust the body’s systemic reactions (e.g., by calming the nerves) (21). Lan et al. (22) established an IBS rat model and used the method of electroacupuncture at the Hegu (LI 4) and Zusanli (ST 36) points to compare changes before and after rat colonic motility and confirmed that the treatment can relieve spasms of the large intestinal smooth muscle and peristalsis in IBS type rats. A similar experiment also reached the same conclusion and found that the effect of Hegu (LI 4) in relieving abdominal pain (i.e., resonance sensitivity) is better than Zusanli (ST 36) (23).
The Neiguan (PC 6) point is a collateral point of the pericardial meridian. Early studies have confirmed that acupuncture at Neiguan (PC 6) directly affects the smooth muscle of the intestine (24) and has a good regulatory effect on IBS-D and gastrointestinal spasm abdominal pain (25). A study showed that acupuncture at Neiguan (PC 6) regulates the vagus nerve (26). A multicenter, large-sample, double-blind randomized controlled study found that acupuncture at bilateral Tianshu (ST 25), Shangjuxu (ST 37), Neiguan (PC 6), and Zusanli (ST 36) was effective at relieving symptoms in chronic functional gastrointestinal disorder (27). Based on these previous studies, we chose the Hegu (LI 4) and Neiguan (PC 6) points to explore the efficacy of acupuncture in inhibiting colonic spasm during endoscopy.
To evaluate the persistence and stability of the efficacy of acupuncture in relieving colonic spasm, the duration of the observation of the antispasmodic effect was 5 minutes (3). The duration of colonic spasm suppression of the acupuncture group was 300 seconds, while that of the sham control group was 268 seconds; however, the time did not differ significantly between the 2 groups (P=0.142). In terms of rebound spasms, no rebound spasms were observed in the test group, but rebound spasms were observed in 3 patients in the control group (P>0.05). Thus, acupuncture of the bilateral Hegu (LI 4) and Neiguan (PC 6) points may not be effective in maintaining the relief of intestinal spasms for a long time. The mild differences in the secondary outcomes may be related to the limited administration of acupuncture for which twirling and rotating only occurred for 15 seconds and the limited number of acupuncture points. Patients’ different levels of sensitivity to acupuncture may have also contributed to the unexpected outcomes.
Unqualified bowel preparation directly affects the quality of colonoscopy, and may lead to a missed diagnosis of colon polyps, re-colonoscopy, and a higher incidence of complications, such as bleeding and perforation (28). At present, the commonly used scale for assessing the quality of bowel preparation is the BBPS, which was also applied in this trial.
This study had several limitations. First, the sample size was small, and it was impossible to achieve double-blind testing. Second, the definition of colonic spasm was subjective, and it was judged by endoscopists but not an objective tool. Third, as only 1 acupuncturist performed the acupuncture operations in this study, the generalizability of the results may be limited. Finally, the observation time of the antispasmodic effect was 5 minutes; thus, the effective time of acupuncture for all patients could not be fully and comprehensively evaluated. These limitations need to be addressed in future studies.
Conclusions
This study showed that acupuncture of the bilateral Hegu (LI 4) and Neiguan (PC 6) points suppressed intestinal spasm and peristalsis. The operation was simple, short-acting, effective, and there were no adverse side effects. Further, the use of gastrointestinal antispasmodic drugs that cause side effects was avoided and thus medical costs were reduced. In the future, more high-level randomized controlled trials need to be conducted to further verify our results.
Acknowledgments
The authors would like to thank the Gastroenterology Endoscopy Center, Dade Road General Hospital, The Second Affiliated Hospital of Guangzhou University of Chinese Medicine for its support.
Funding: This work was supported by the clinical research of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine (No. YN10101914), and Guangzhou University of Chinese Medicine “Double First-Class” and High-Level University Discipline Collaborative Innovation Team (No. 2021xk58).
Footnote
Reporting Checklist: The authors have completed the CONSORT reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-407/rc
Trial Protocol: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-407/tp
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-407/dss
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-407/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work, including ensuring that any questions related to the accuracy or integrity of any part of the work have been appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of The Second Affiliated Hospital of Guangzhou University of Chinese Medicine (No. YF2020-150-01). Informed consent was obtained from all individual participants.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Fang Y, Wu J, Liu Q, et al. A prospective control study of painless colonoscopy and conventional colonoscopy. Chinese Journal of Digestive Endoscopy 2014;31:494-8.
- Nemoto D, Utano K, Isohata N, et al. Topical lidocaine inhibits spasm during colonoscopy: a double-blind, randomized controlled trial (with video). Endosc Int Open 2017;5:E402-7. [Crossref] [PubMed]
- Nemoto D, Suzuki S, Mori H, et al. Inhibitory effect of lidocaine on colonic spasm during colonoscopy: A multicenter double-blind, randomized controlled trial. Dig Endosc 2019;31:173-9. [Crossref] [PubMed]
- Yu Z, Zhang N, Lu CX, et al. Electroacupuncture at ST25 inhibits jejunal motility: Role of sympathetic pathways and TRPV1. World J Gastroenterol 2016;22:1834-43. [Crossref] [PubMed]
- Sun JW, Sun ML, Li D, et al. Efficacy of acupuncture based on acupoint combination theory for irritable bowel syndrome: a study protocol for a multicenter randomized controlled trial. Trials 2021;22:719. [Crossref] [PubMed]
- Wang H, Du Y. Acupuncture and Moxibustion. Beijing, China Press of Traditional Chinese Medicine 2012:36+86.
- Fu Y, Xue L, Lu Z, et al. Application of topical lidocaine in colonoscopy. China Practical Medicine 2018;16:7-9.
- Yan C. Discussion on the relationship between the regulation of gastric motility by acupuncture "Zusanli" and SP and MTL. Hunan University of Traditional Chinese Medicine, 2012.
- Qin Q, Wang H, Liu K, et al. The two-way regulating effect of acupuncture Tianshu on the motor function of different intestinal segments in rats with normal, constipation and diarrhea. World Traditional Chinese Medicine 2013;8:245-9.
- Zhou S. Research on the central response mechanism of acupuncture at Tianshu acupoint on the two-way regulation of intestinal function. Chengdu University of Traditional Chinese Medicine, 2014.
- Takahashi T. Mechanism of acupuncture on neuromodulation in the gut-a review. Neuromodulation 2011;14:8-12. [Crossref] [PubMed]
- Ren B, Yu Z, Xu B. Overview of the two-way regulating effect of acupuncture on gastrointestinal motility. Chinese Acupuncture and Moxibustion 2012;32:765-8. [PubMed]
- Wu J, Wu X. Overview of the research on the mechanism of acupuncture and moxibustion in the treatment of digestive system diseases. Chinese Emergency in Traditional Chinese Medicine 2012;21:1115-6.
- Zhu B. The biological significance of the two-way regulating effect of acupuncture and moxibustion. World Traditional Chinese Medicine 2013;8:241-4.
- Lu MJ, Yu Z, He Y, et al. Electroacupuncture at ST36 modulates gastric motility via vagovagal and sympathetic reflexes in rats. World J Gastroenterol 2019;25:2315-26. [Crossref] [PubMed]
- Mao T, Zhou S, Zhao M, et al. Regulatory effect of acupuncture on bowel movement and its neural mechanism. World Chinese Journal of Digestion 2014;22:3780-5. [Crossref]
- Wang W, Liang F, Chen R. Research progress and thinking on the mechanism of acupuncture and moxibustion regulating gastrointestinal motility. Acupuncture Research 2020;45:771-5. [PubMed]
- Yu Z. Neuromechanism of acupuncture regulating gastrointestinal motility. World J Gastroenterol 2020;26:3182-200. [Crossref] [PubMed]
- Long X, Jiang H, Ren X. Research progress on neurohumoral and immune mechanisms of acupoint compatibility. Acupuncture Research 2015;40:314-8. [PubMed]
- He L, Chen S, Wang L. Clinical Acupuncture. Beijing, People's Military Medical Press, 2003:71.
- Wang D. Quick reference to the symptomatic acupoint selection. Beijing, Chemical Industry Press, 2011:30.
- Lan Y, Gao Y, Zhu W, et al. Comparison of the effects of electroacupuncture at "Hegu" and "Zusanli" points on colonic motility and colonic M3 receptor expression in IBS model rats. Journal of Beijing University of Traditional Chinese Medicine 2017;40:1044-9.
- Qin Y, Guo M, Lan Y, et al. The effect of electroacupuncture at different points on the intestinal motility and sensitivity of rats with irritable bowel syndrome. Zhen Ci Yan Jiu 2020;45:293-8. [PubMed]
- Cheng X, Zhang K. Observation on the effect of acupuncture on diarrhea-type irritable bowel syndrome. Shanxi Traditional Chinese Medicine 2017;33:35+45.
- Li L, Wang Z, Yi R, et al. Clinical observation on the eight methods of Linggui to select points for the treatment of diarrheal irritable bowel syndrome. Shanghai Journal of Acupuncture and Moxibustion 2017;36:1181-5.
- Lu M, Chen C, Li W, et al. EA at PC6 Promotes Gastric Motility: Role of Brainstem Vagovagal Neurocircuits. Evid Based Complement Alternat Med 2019;2019:7457485. [Crossref] [PubMed]
- Zhao J, Chen M, Wang X, et al. Efficacy of acupuncture in refractory irritable bowel syndrome: study protocol for a randomised controlled trial. BMJ Open 2021;11:e045655. [Crossref] [PubMed]
- ASGE Standards of Practice Committee. Bowel preparation before colonoscopy. Gastrointest Endosc 2015;81:781-94. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)








