Adverse health behaviours among colorectal cancer survivors: a case study from Iran
Introduction
Globally, colorectal cancer (CRC) is ranked as the third most common cancer diagnosed in men and the second in women (1). In recent decades, the number of cancer survivors including CRC survivors, has been increased as a result of advances in early detection and curative treatment options (2). Cancer survivors have a higher risk of developing secondary tumours, heart disease, type 2 diabetes, and osteoporosis (3,4). Coronary artery disease becomes the leading cause of death in CRC, breast and endometrial cancer survivors approximately ten years after diagnosis (5-7). A part of this is because they share the similar lifestyle factors [diet, body weight, physical activity (PA), and smoking] (8). There is evidence that cancer-related outcomes such as quality of life, and prognosis are influenced by lifestyle factors. Adverse health behaviours such as smoking, inadequate fruit and vegetable consumption, insufficient PA and obesity have repeatedly been shown to negatively impact outcomes in survivors of different cancer types (9,10).
Results of previous studies showed, despite the lifestyle recommendation, adherence to healthy behaviours is inadequate among cancer survivors, for example, the majority of survivors (80%) in the ACS-SCS II study which examined over 9,000 survivors across six different cancer types, did not meet the 5-A-day dietary recommendation (five serving of fruits and vegetable per day according to current dietary guidelines) (9). Meeting PA recommendation is even much worse among cancer survivors (10,11). Smoking have negative consequences on cancer outcomes, for instance, results of a meta-analysis of different studies of lung cancer survivors showed a lower five year survival rates for smokers in compared to non-smokers or former smokers (33% and 70%, respectively) (12). A history of ever-smoking can also impact outcomes in colon cancer, as a recent study demonstrated a significantly shorter disease-free survival in ever-smokers (12,13). Evidence showed that adherence to lifestyle recommendation in CRC patients may reduce the recurrence, prevent the development of a secondary cancer and improve quality of life (9,14).
CRC is one of the most common cancers in Iran (15), overall, it is the fourth common cancer in Iran and is ranked the third and fifth most common cancer in women and men respectively. The age-standardized incidence rates in men and women were 11.31 and 10.89 in Iran respectively (14). Research examining the adverse health behaviours among CRC survivors in Iran is scarce while this group of patients are more vulnerable to negative health outcomes. The aim of this study was to identify the sociodemographic, and health related predictors of adverse health behaviours among CRC survivors in Babol, North of Iran where CRC is one of the most common cancers and the trend of CRC showed an increase in recent years (16).
Methods
This cross-sectional study was conducted in Babol city located in North of Iran. The Babol cancer registry is the first population-based cancer registry established in 1960s (17). For the purpose of this study the CRC survivors were selected from the registry database. The pathologic information (using ICD-10 code), demographic characteristics and tumor information including topography code (ICD-0-C) and pathology code (ICD-0-M) were collected. Subjects with C18 (colon), C19 (recto-sigmoid junction), C20 (rectum), and C21 (anus and anal canal) codes recorded between 2007–2013 were included in the study (n=332). The inclusion criteria were as follows: (I) having the listed codes; (II) being alive; (III) currently residing in Babol; and (IV) diagnosis during the specified periods. Lacks of cooperation and incorrect address or phone number were the exclusion criteria. After excluding people who no longer resided in Babol (37 cases), deaths (112 cases), migrate (six cases), non-cooperative (four cases) and incorrect phone and home addresses (16 cases); the questionnaires were completed for all the remaining 157 patients.
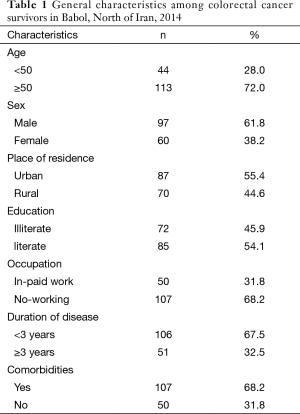
Demographic information was collected via self-report including age, education, employment status, place of residency. Age was categorized into two categories; <50 and ≥50 years, education was classified as illiterate, literate, occupation (in-paid work or no-working) and place of residency urban/rural. Patients were also asked whether they experienced various comorbid conditions (including heart disease, hypertension, chronic back pain, arthritis, stroke, osteoporosis, asthma, chronic obstructive pulmonary disease, stomach and/or intestinal problems, and diabetes).
Insufficient PA, inadequate consumption of fruit and vegetables and smoking habits were considered as adverse health behaviours in this study. PA was measured via the validated Godin Leisure-Time Exercise Questionnaire (18,19) and was classified into two categories: insufficient PA; sufficient PA. Adequate consumption of fruit and vegetable; 5-A-day, was measured by asking survivors the question, “How many times do you eat fruits and vegetables a day?” (19). It was subsequently categorised into two categories: inadequate 5-A-day; adequate 5-A-day. Smoking was measured via this question “Do you currently smoke cigarettes on a regular basis” rated on a yes/no scale. Hookah smoking was measured via this question “Do you smoke hookah on a regular basis” (at least one per week) and a dummy variable created based on these two questions (0 not smoking, 1 smoking). Crude and adjusted odds ratios (ORs) were presented. In multiple logistic regression models, adverse health behaviours (smoking, inadequate PA, inadequate 5-A-day) were considered as dependant variable, and age, sex, place of residency, work status, education, time since diagnosis, and comorbidities were considered as covariates.
This study received Ethics approval from Tabriz University of Medical sciences; Ethics Committee. All patients completed a consent form before the interview.
Results
A total of 157 CRC survivors were included in this study. The majority of them were male, more than 50 years of age, and more than half resided in urban areas. About 46% of them had no education, and about two-third were currently not working. The majority of them (68%) were diagnosed less than 3 years ago and 67% of survivors had at least one comorbid condition (Table 1).
Full table
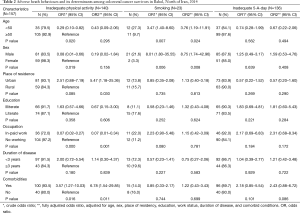
Adverse health behaviours, sociodemographic and clinical characteristics of CRC survivors are presented in Table 2. In general, the majority of people with CRC were not meeting the recommendation for PA (89%), and 5-A-day recommendation (86.6%), in addition only 14.6% of them were smoke either cigarette or hookah.
Full table
Results of multiple logistic regression models showed relative to survivors ≥50 years of age, younger survivors less likely to report insufficient PA, crude OR =0.29 (95% CI: 0.10–0.82, P=0.02), however the effect was attenuated in fully adjustment model. The number of women who were not meeting the PA recommendation was higher than men (about 98% vs. 84%). Crude OR was 0.08 (95% CI: 0.01–0.66) for men relative to women. Urban residents were more likely report insufficient PA (adjusted OR =5.47, 95% CI: 1.18–25.36, P=0.03). Insufficient PA were lower in those who were currently working compared to survivors who were not working (adjusted OR =0.07, 95% CI: 0.01–0.34, P=0.001). Crude OR was 3.57 (95% CI: 1.27–10.03) for survivors with at least one comorbid condition, adjustment for other variables increased the OR to 6.78 (95% CI: 1.54–29.85).
Younger survivors were more likely to be smoker compared to survivors ≥50 years of age (adjusted OR =3.76, 95% CI: 1.19–11.91). The same was true for men survivors compared to women (adjusted OR =8.75, 95% CI: 1.74–42.96).
The majority of survivors were not meeting 5-A-day recommendation, however survivors from urban areas less likely to report inadequate 5-A-day in comparison to those from rural areas (adjusted OR =0.57, 95% CI: 0.20–1.60). Illiterate survivors were more likely to not meeting recommendations (adjusted OR =1.81, 95% CI: 0.60–5.43). The same was true for survivors who were involved in in-paid working and those with comorbidities (adjusted OR =2.31, 95% CI: 0.68–8.34; and 2.43, 95% CI: 0.88–6.72 respectively).
Discussion
The main aim of this study was to assess the prevalence of adverse health behaviours and its determinants among CRC survivors in Babol, North of Iran. Our results showed that the majority of people with CRC were not meeting the recommendation for PA, and for 5-A-day, whereas most of them were not smoking or using hookah. Poor healthy lifestyle behaviours among CRC survivors and other cancer survivors has been reported previously in other studies (9,10,20,21). However Demark-Wahnefried et al. in a study among breast and prostate cancer survivors reported a higher percentage of healthy behaviours; in their study 42% of survivors reported daily consumption of ≥5 fruits & vegetables, but their results might be subject to bias toward reporting healthy behaviours because of low participation rate (22).
The majority of people with CRC were not meeting the recommendation for 5-A-day (86.6%), it was consistent with previous studies that indicated poor adherence to dietary recommendations (5-A-day serving of fruit and vegetables) among people with CRC (9,10,21,23). For instance, Blanchard et al found that only 15.9% colorectal survivors were meeting adequate (5-A-day) fruit and vegetable consumption (9).
The prevalence of sufficient PA was only 11%; women survivors, older patients, not working status, and those with comorbidities had a greater likelihood of not meeting the recommendation. Insufficient PA was much higher than the percentage reporting from other studies; for instance in a study in the US, 35% of colorectal survivors had sufficient PA (9) and based on the results of a study in Korea 26% of cancer survivors were meeting the PA recommendation (24). Evidence from other studies showed that younger cancer survivors (18 to 40 years of age) were more likely to meet the PA recommendations (37.6%) than older survivors (age 40 to 64 years of age and those ≥65 years of age which were 33.0% and 24.9% respectively) (25). It has been shown that male cancer survivors were more likely to meet PA recommendations than female, and those with more than two comorbidities have an increased the odds of being sedentary (25). This percentage is below than those found in the healthy population; based on a nationwide survey where 40% of adults belonged to low and 15% had no PA at all (26). However, percentage of 5-A-day consumption (13.4%) is similar to healthy population (12.5%) (27). In general healthy people also are below the recommendation, this suggest a need for a nationwide campaign in order to increase the consumption of fruit and vegetable to an optimal level.
The prevalence of current smoking was about 15% in this study, it was higher than other studies which reported about 10% (9,24). However, the prevalence of smoking cigarette/hookah among CRC survivors was lower than that in general population (14.6% vs. 22.7% for only cigarette smoking) (28). National data showed the prevalence of 14.2% for current cigarette smoking (29), in our study we combined cigarette and hookah smoking since both were important and it is recommended to be quitted after diagnosis. The prevalence of only smoking was about 10% which is lower than the national average. The findings of this study showed that younger CRC survivors and male patients had a greater likelihood of being current smoker. Similar finding from another study showed that, younger survivors (18 to 40 years) are at greater risk for continued smoking than controls (25).
A link between smoking after diagnosis of CRC and risk of death from CRC is about twice (30), this suggests that recommendation for smoking might be more effective or perhaps is more sensitive in this context since it usually comes forward than PA and fruit and vegetable consumption while these two factors are linked to higher recurrence and mortality and following the recommendations by cancer survivors will provide even a greater benefit.
The strengths of this study were registry-identified cancer diagnosis, lifestyle behaviour assessment comparable to similar studies, there are some limitations; firstly, the self-report assessments of adverse health behaviours rather than objective measurements which subject to recall bias. It is recommended using objective indicators in future research to better evaluation of current pattern in the present study. Secondly, pre-diagnosis lifestyle behaviours were not measured. However, it was more subject to recall bias and would not be feasible to asses in such study. Prospective research studies are recommended to examine time trend of changes in lifestyle behaviours among people with cancer.
Conclusions
This study showed that only the minority of CRC survivors were meeting the PA or 5-A-day recommendations. Female gender, illiteracy, comorbidities, place of residency were the important determinants of having adverse health behaviours, it is important to notify the health policy makers and to develop a comprehensive educational program to enhance the adherence to healthy lifestyle recommendations among CRC survivors.
Acknowledgements
A substantial part of this study was supported by Research Council of Tabriz University of Medical Sciences. We gratefully thank Mr. Habib Zadeh, Mr. Mirzad, Mrs. Mousavi, the staff at the Screening and Counselling Centre of Babol, and all patients and their families who participated in this study.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Ferlay J, Soerjomataram I, Ervik M, et al. GLOBOCAN 2012 v1.0, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 11 [Internet]. Lyon, France: International Agency for Research on Cancer. Available online: http://globocan.iarc.fr
- Vijayvergia N, Denlinger CS. Lifestyle Factors in Cancer Survivorship: Where We Are and Where We Are Headed. J Pers Med 2015;5:243-63. [Crossref] [PubMed]
- Yabroff KR, Lawrence WF, Clauser S, et al. Burden of illness in cancer survivors: findings from a population-based national sample. J Natl Cancer Inst 2004;96:1322-30. [Crossref] [PubMed]
- Søgaard M, Thomsen RW, Bossen KS, et al. The impact of comorbidity on cancer survival: a review. Clin Epidemiol 2013;5:3-29. [Crossref] [PubMed]
- Ward KK, Shah NR, Saenz CC, et al. Cardiovascular disease is the leading cause of death among endometrial cancer patients. Gynecol Oncol 2012;126:176-9. [Crossref] [PubMed]
- van Erning FN, van Steenbergen LN, Lemmens VE, et al. Conditional survival for long-term colorectal cancer survivors in the Netherlands: who do best? Eur J Cancer 2014;50:1731-9. [Crossref] [PubMed]
- Patnaik JL, Byers T, DiGuiseppi C, et al. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res 2011;13:R64. [Crossref] [PubMed]
- Demark-Wahnefried W, Jones LW. Promoting a healthy lifestyle among cancer survivors. Hematol Oncol Clin North Am 2008;22:319-42. [Crossref] [PubMed]
- Blanchard CM, Courneya KS, Stein K, et al. Cancer survivors' adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society's SCS-II. J Clin Oncol 2008;26:2198-204. [Crossref] [PubMed]
- Blanchard CM, Stein KD, Baker F, et al. Association between current lifestyle behaviors and health-related quality of life in breast, colorectal, and prostate cancer survivors. Psychology & Health 2004;19:1-13. [Crossref]
- Nayak P, Holmes HM, Nguyen HT, et al. Self-reported physical activity among middle-aged cancer survivors in the United States: Behavioral Risk Factor Surveillance System Survey, 2009. Prev Chronic Dis 2014;11:E156. [Crossref] [PubMed]
- Parsons A, Daley A, Begh R, et al. Influence of smoking cessation after diagnosis of early stage lung cancer on prognosis: systematic review of observational studies with meta-analysis. BMJ 2010;340:b5569. [Crossref] [PubMed]
- Phipps AI, Shi Q, Newcomb PA, et al. Associations between cigarette smoking status and colon cancer prognosis among participants in North Central Cancer Treatment Group Phase III Trial N0147. J Clin Oncol 2013;31:2016-23. [Crossref] [PubMed]
- American Cancer Society. Cancer treatment and survivorship facts & figures 2012–2013. Atlanta, GA: American Cancer Society, 2012.
- Ministry of Health and Medical Education Cancer office. Introduction. Cancer registration country reports 2009. Iran, 2012.
- Nikbakht H, Aminisani N, Asghari Jafarabadi M, et al. Trends in the Incidence of Colorectal Cancer and Epidemiologic and Clinical Characteristics of Survivors in Babol City in 2007-2012. JBUMS 2015;17:7-14.
- Etemadi A, Sadjadi A, Semnani S, et al. Cancer registry in Iran: a brief overview. Arch Iran Med 2008;11:577-80. [PubMed]
- Jacobs DR Jr, Ainsworth BE, Hartman TJ, et al. A simultaneous evaluation of 10 commonly used physical activity questionnaires. Med Sci Sports Exerc 1993;25:81-91. [Crossref] [PubMed]
- Godin G, Shephard RJ. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci 1985;10:141-6. [PubMed]
- Mulhern RK, Tyc VL, Phipps S, et al. Health-related behaviors of survivors of childhood cancer. Med Pediatr Oncol 1995;25:159-65. [Crossref] [PubMed]
- James AS, Campbell MK, DeVellis B, et al. Health behavior correlates among colon cancer survivors: NC STRIDES baseline results. Am J Health Behav 2006;30:720-30. [Crossref] [PubMed]
- Demark-Wahnefried W, Peterson B, McBride C, et al. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer 2000;88:674-84. [Crossref] [PubMed]
- Doyle C, Kushi LH, Byers T, et al. Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin 2006;56:323-53. [Crossref] [PubMed]
- Oh MG, Han MA, Park J, et al. Health behaviors of cancer survivors: the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV, 2007-09). Jpn J Clin Oncol 2013;43:981-7. [Crossref] [PubMed]
- Bellizzi KM, Rowland JH, Jeffery DD, et al. Health behaviors of cancer survivors: examining opportunities for cancer control intervention.Health behaviors of cancer survivors: examining opportunities for cancer control intervention. J Clin Oncol 2005;23:8884-93. [Crossref] [PubMed]
- Esteghamati A, Khalilzadeh O, Rashidi A, et al. Physical activity in Iran: results of the third national surveillance of risk factors of non-communicable diseases (SuRFNCD-2007). J Phys Act Health 2011;8:27-35. [PubMed]
- Esteghamati A, Noshad S, Nazeri A, et al. Patterns of fruit and vegetable consumption among Iranian adults: a SuRFNCD-2007 study. Br J Nutr 2012;108:177-81. [Crossref] [PubMed]
- Sharifi H, Heydari GR, Emami H, et al. Tobacco smoking pattern: cigarette vs. hookah. Tanaffos 2009;8:62-67.
- Meysamie A, Ghaletaki R, Haghazali M, et al. Pattern of tobacco use among the Iranian adult population: results of the national Survey of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007). Tob Control 2010;19:125-8. [Crossref] [PubMed]
- Yang B, Jacobs EJ, Gapstur SM, et al. Active smoking and mortality among colorectal cancer survivors: the Cancer Prevention Study II nutrition cohort. J Clin Oncol 2015;33:885-93. [Crossref] [PubMed]


