Clinical outcomes of pancreaticoduodenectomy in octogenarians: a surgeon’s experience from 2007 to 2015
Introduction
Pancreaticoduodenectomy (PD) is a complex procedure used to resect the duodenum and head of the pancreas. An early version of this procedure was first successfully performed by Dr. Walther Kausch in 1909, and the procedure was popularized by Dr. Allen Whipple in the 1930s (1-3). Prior to the 1980s, PD was performed infrequently due to high hospital mortality up to 25%. As high-volume centers were developed and advances in perioperative care were made, hospital mortality dramatically decreased (1,2). Currently, PD is performed for malignant diseases of the periampullary region and for nonmalignant indications such as chronic pancreatitis.
The number of elderly people in the United States population continues to increase each year. Over next two decades, the population aged 85 and older will double, and by the year 2049, the number is projected to triple (4). Given that the incidence of periampullary malignancies increases with age, it is expected that a greater number of elderly patients will be referred for PD, the only curative option for periampullary malignancies (5). Moreover, while mortality rates associated with other cancers (e.g., breast, colorectal, and prostate cancers) are projected to decrease, deaths from pancreatic cancer are projected to dramatically increase. Pancreatic cancer is expected to become second in causes of cancer-related deaths by 2030 (6).
Previously, a large population-based study and a meta-analysis have shown that PD in octogenarians may be associated with increased morbidity and mortality rates (7,8). However, in our experience, many octogenarians have successfully undergone PD without significantly increased mortality or morbidity. The objective of this study is to evaluate mortality and morbidity of PD in octogenarians, as performed by a single surgeon at a high-volume tertiary referral hospital, compared to that of younger patients and to discuss the importance of pre-operative and post-operative management for successful PD.
Methods
Patients
Institutional internal review board approval was obtained, and the study was conducted in accordance with its guidelines. Medical records of patients who underwent PD performed by a single surgeon were retrospectively reviewed to identify pre-operative medical comorbidities, estimated blood loss, operative time, histopathology of surgical specimens, peri-operative mortality, post-operative complications, and length of stay.
Pre-operative comorbidities of patients included in this study were ASA Physical Status Score, myocardial infarction, coronary artery disease, congestive heart failure, hypertension, diabetes, chronic obstructive pulmonary disease, chronic kidney disease, cerebral vascular accident, and hyperlipidemia. Post-operative complications reviewed were in-hospital mortality, re-operation, myocardial infarction, cardiac arrest, re-intubation, ventilator dependence for more than 48 hours, pulmonary embolism, acute renal failure, wound infection, intra-abdominal abscess, biliary leak, and pancreatic fistula.
Statistical analysis
A two-sided Fisher’s exact statistical analysis was used for comparative analysis between a group of patients 79 years old or younger (non-octogenarian) and a group of patients 80 years old or older (octogenarians). P value less than 0.05 was considered statistically significant.
Results
Patient demographics
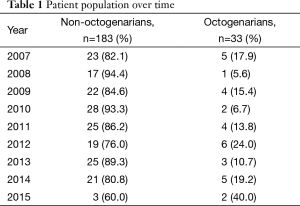
From January 2007 to April 2015, 216 patients underwent PD by a single surgeon at a tertiary hospital. There were 183 non-octogenarians and 33 octogenarians. Table 1 shows the change over time in the age of the patients who underwent PD. About 11.8% of patients from 2007 to 2010 were octogenarians. 17.7% of patients from 2010 to 2015 were octogenarians.
Full table
Pre-operative comorbidities
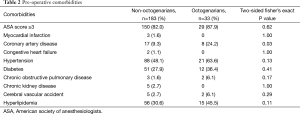
As shown in Table 2, 82.0% of non-octogenarians and 87.9% of octogenarians had ASA score 3 or greater (P=0.62). Although 3 non-octogenarians and no octogenarians had a history of myocardial infarction, octogenarians were significantly more likely to have coronary artery disease (P=0.03). In this study, octogenarians were more likely to have hypertension, diabetes, chronic obstructive pulmonary disease, cerebral vascular accident, and hyperlipidemia. (P=0.13, 0.41, 0.17, 0.29, 0.11, respectively). With a larger sample size, there may be statistical significance in these factors. Our data suggests that octogenarians may have more medical comorbidities that can affect clinical outcomes after PD.
Full table
Intra-operative factors
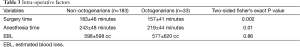
Table 3 summarizes intra-operative factors that may contribute to postoperative course after PD. Surgery time (157±41 minutes) and anesthesia time (219±44 minutes) in octogenarians were significantly shorter when compared to the younger cohort (P=0.002, 0.01, respectively). Although our average surgery time was significantly shorter than previously reported, a similar trend of shorter surgery time in octogenarians has been reported (7). Estimated blood loss was similar in the two cohorts (P=0.86).
Full table
Surgical pathologies
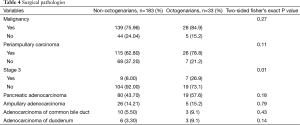
Table 4 shows surgical specimen pathologies. The majority of our patients underwent PD as a curative option for a malignant disease process. 76.0% of non-octogenarians and 84.9% of octogenarians had a malignancy (P=0.27). Of those with malignancies, 62.8% of non-octogenarians and 78.8% of octogenarians had periampullary carcinoma (P=0.11). Although the proportion of patients undergoing PD for periampullary carcinoma was not statistically different between the two age groups, octogenarians were significantly more like to present with stage 3 disease, 26.9% compared to 8% (P=0.01). Our data demonstrates a higher tumor burden and a more advanced disease state in octogenarians, compared to the younger cohort.
Full table
Surgical margin was assessed in 139 non-octogenarians and 28 octogenarians with malignancy (Table 5). R0 resection was achieved in 71.2% of non-octogenarians and 78.6% of octogenarians (P=0.63).

Full table
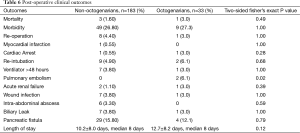
Post-operative clinical outcome
As shown in Table 6, there was not a statistically significant difference in the mortality rate, overall morbidity rate, and rate of repeat operations between two age groups (P=0.49, 1.00, 1.00, respectively). One complication found to be statistically higher in the octogenarians was pulmonary embolism, 6.1% vs. 0% (P=0.02). There were two octogenarians who developed pulmonary embolism. However, these were non-fatal events. One patient was discharged home with an inferior vena cava filter in place, and the other patient was discharged on therapeutic anticoagulation.
Full table
Discussion
As the elderly population in the United States continues to grow, an increasing number of elderly patients are projected to develop periampullary malignancies (1,4,5). As PD remains the only potentially curative therapy for these malignancies (3), more elderly patients will present to surgeons for surgical intervention. Elderly patients will likely have more pre-operative comorbidities affecting peri-operative morbidity and mortality, and surgeons will be required to determine which elderly patients will be reasonable surgical candidates.
Previous studies have shown varied clinical outcomes of elderly patients undergoing PD (7-14). While there are studies that suggest advanced age to be a risk factor associated with increased postoperative complications and mortality after PD (7,8), others have shown no increased risk with advanced age (9-12,14). Another study, however, demonstrated that while elderly patients can undergo pancreatic resection safely, they have poorer long-term survival (13). As such, while PD remains the only curative therapy available for patients of all ages, performing PD in octogenarians remains controversial.
Although this study has limitations due to small sample size, absence of long-term follow-up, and the inherent nature of the retrospective analysis, our experience is that octogenarians can undergo PD with outcomes similar to younger age groups. Although pulmonary embolism was more common in octogenarians after PD, development of pulmonary embolism was non-fatal and did not result in long-term disability. In these patients, as in all of our other patients without contraindications for anticoagulation, medical venous thromboembolism (VTE) prophylaxis was initiated on postoperative day 1. One of the patients developed gastrointestinal bleeding and VTE prophylaxis had to be discontinued. Earlier studies have suggested a higher risk of VTE in cancer patients with a higher grade tumor or more advanced cancer stage (15,16). Higher rates of PE seen in our octogenarians group may also be associated with greater tumor burden.
To optimize clinical outcome after PD, pre-operative decisions should be preceded by individualized evaluations. Our practice is to consult with each patient’s cardiologist and/or pulmonologist for those with a medical history of cardiac or pulmonary disease, respectively. Patients with significant coronary artery disease typically undergo either cardiac stenting or bypass surgery prior to PD. Pre-operatively, hypertension and diabetes are medically optimized. Ultimately, the decision to offer surgery is made by the attending surgeon after reviewing subspecialist evaluations and preoperative testing results, and by assessing each patient’s functional status via evaluation of an individual’s capacity to perform activities of daily living independently.
Following PD, patients at our institution are routinely admitted to the surgical intensive care unit, staffed by surgical critical care physicians. The majority of patients are extubated at the end of the surgery, and patients’ hemodynamics and respiratory status are carefully monitored. On post-operative day one patients are encouraged to be out of bed, in a chair, and ambulating, if possible. Patients are transferred out of the intensive care unit on postoperative day 1, if deemed appropriate by the surgeon. Patients’ pain control regimen is also optimized in order facilitate early ambulation and mobilization. For those patients with less mobility, physical therapists are readily available to assist in passive exercise with the aim of progressively increasing mobility.
Early enteral feeding is also advocated at our institution. All patients have nasogastric tubes placed at the time of surgery and erythromycin, a promotility agent, is given post-operatively to improve gastric emptying. After return of bowel function, the nasogastric tube is removed, and patients are started on a liquid diet. At that time, an amylase level is measured from the output of the surgical drain in the area of the pancreatic resection. If the amylase level is appropriate, the patient’s diet is advanced to a post-gastrectomy diet consisting of small meals every few hours. If a pancreatic fistula is diagnosed, patients are discharged with drain in place with close follow-up in clinic, and drains are removed when the output becomes minimal. This practice has allowed us to keep our median length of hospital stay after surgery to 8 days.
Although other studies have demonstrated higher rates of mortality and morbidity in the elderly patient population when compared to younger patient population (7,8,17), our experience shows that with careful pre-operative planning and post-operative care, PD can be performed safely in patients 80 years and older. In a study that shows similar overall morbidity and mortality between elderly and younger patient groups, there was a statistically significant increase in mortality when elderly patients had chronic obstructive pulmonary disease (18). However, in our experience, patients with pulmonary comorbidities including chronic obstructive pulmonary disease had no life-threatening complications or mortalities during their post-operative course.
With improvement in operative technique, anesthesia, and perioperative care along with increasing volume of PD cases, overall complications after PD have declined over time (19-21). Furthermore, our conclusion that advanced age alone should not be a contraindication to PD is supported by other studies. Although exact age groups differ, another group has shown that elderly patients can undergo PD safely with similar long-term survival rates as the younger cohorts (22). Furthermore, in a study showing poorer ASA status and higher complication rates in octogenarians, age alone was not an independent marker of prognosis (23).
Conclusions
With thorough pre-operative evaluation of patients and careful peri-operative care, patients 80 years and older can undergo PD by a high-volume, experienced surgeon with outcomes similar to that of the overall or younger population. Thus, patients should not be denied a curative surgical option for periampullary disease based on advanced age alone. Future studies using a larger prospective database are warranted to better inform our patients and surgeons regarding risks and benefits of PD in elderly patients.
Acknowledgements
This work was supported by the Department of Surgery at the Houston Methodist Hospital.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the Houston Methodist Institutional Review Board (No. Pro00012880).
References
- Are C, Dhir M, Ravipati L. History of pancreaticoduodenectomy: early misconceptions, initial milestones and the pioneers. HPB (Oxford) 2011;13:377-84. [Crossref] [PubMed]
- Cameron JL, Riall TS, Coleman J, et al. One thousand consecutive pancreaticoduodenectomies. Ann Surg 2006;244:10-5. [Crossref] [PubMed]
- Berberat PO, Friess H, Kleeff J, et al. Prevention and treatment of complications in pancreatic cancer surgery. Dig Surg 1999;16:327-36. [Crossref] [PubMed]
- Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States 2014;25-1140.
- Yeo TP. Demographics, epidemiology, and inheritance of pancreatic ductal adenocarcinoma. Semin Oncol 2015;42:8-18. [Crossref] [PubMed]
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913-21. [Crossref] [PubMed]
- de la Fuente SG, Bennett KM, Pappas TN, et al. Pre- and intraoperative variables affecting early outcomes in elderly patients undergoing pancreaticoduodenectomy. HPB (Oxford) 2011;13:887-92. [Crossref] [PubMed]
- Sukharamwala P, Thoens J, Szuchmacher M, et al. Advanced age is a risk factor for post-operative complications and mortality after a pancreaticoduodenectomy: a meta-analysis and systematic review. HPB (Oxford) 2012;14:649-57. [Crossref] [PubMed]
- Hannoun L, Christophe M, Ribeiro J, et al. A report of forty-four instances of pancreaticoduodenal resection in patients more than seventy years of age. Surg Gynecol Obstet 1993;177:556-60. [PubMed]
- Delcore R, Thomas JH, Hermreck AS. Pancreaticoduodenectomy for malignant pancreatic and periampullary neoplasms in elderly patients. Am J Surg 1991;162:532-5; discussion 535-6. [Crossref] [PubMed]
- Sohn TA, Yeo CJ, Cameron JL, et al. Should pancreaticoduodenectomy be performed in octogenarians? J Gastrointest Surg 1998;2:207-16. [Crossref] [PubMed]
- Chijiiwa K, Yamaguchi K, Yamashita H, et al. ASA physical status and age are not factors predicting morbidity, mortality, and survival after pancreatoduodenectomy. Am Surg 1996;62:701-5. [PubMed]
- Oliveira-Cunha M, Malde DJ, Aldouri A, et al. Results of pancreatic surgery in the elderly: is age a barrier? HPB (Oxford) 2013;15:24-30. [Crossref] [PubMed]
- Scurtu R, Bachellier P, Oussoultzoglou E, et al. Outcome after pancreaticoduodenectomy for cancer in elderly patients. J Gastrointest Surg 2006;10:813-22. [Crossref] [PubMed]
- Abu Saadeh F, Norris L, O'Toole S, et al. Venous thromboembolism in ovarian cancer: incidence, risk factors and impact on survival. Eur J Obstet Gynecol Reprod Biol 2013;170:214-8. [Crossref] [PubMed]
- Abdel-Razeq HN, Mansour AH, Ismael YM. Incidental pulmonary embolism in cancer patients: clinical characteristics and outcome--a comprehensive cancer center experience. Vasc Health Risk Manag 2011;7:153-8. [Crossref] [PubMed]
- Faraj W, Alameddine R, Mukherji D, et al. Postoperative outcomes following pancreaticoduodenectomy: how should age affect clinical practice? World J Surg Oncol 2013;11:131. [Crossref] [PubMed]
- Casadei R, Zanini N, Morselli-Labate AM, et al. Prognostic factors in periampullary and pancreatic tumor resection in elderly patients. World J Surg 2006;30:1992-2001; discussion 2002-3.
- Fernández-del Castillo C, Morales-Oyarvide V, McGrath D, et al. Evolution of the Whipple procedure at the Massachusetts General Hospital. Surgery 2012;152:S56-63. [Crossref] [PubMed]
- Yeo CJ, Cameron JL, Sohn TA, et al. Six hundred fifty consecutive pancreaticoduodenectomies in the 1990s: pathology, complications, and outcomes. Ann Surg 1997;226:248-57; discussion 257-60. [Crossref] [PubMed]
- Matsuoka L, Selby R, Genyk Y. The surgical management of pancreatic cancer. Gastroenterol Clin North Am 2012;41:211-21. [Crossref] [PubMed]
- Ito Y, Kenmochi T, Irino T, et al. The impact of surgical outcome after pancreaticoduodenectomy in elderly patients. World J Surg Oncol 2011;9:102. [Crossref] [PubMed]
- Khan S, Sclabas G, Lombardo KR, et al. Pancreatoduodenectomy for ductal adenocarcinoma in the very elderly; is it safe and justified? J Gastrointest Surg 2010;14:1826-31. [Crossref] [PubMed]


