
Surgical considerations for the “perfect” colorectal anastomosis
Introduction
Anastomotic leak is one of the most discussed and dreaded complication in colorectal surgery. It is of utmost importance to prevent a leak as it may lead to prolonged hospital stay, repeated operations, stoma formation, anastomotic stricture formation and even mortality in patients (1-3).
Numerous clinical risk factors have been analysed to be associated with anastomotic leakage. Many of these patient factors [e.g., body mass index (BMI) and American Society of Anaesthesiology (ASA) score] and disease factors (e.g., tumour size and location) are not readily modifiable, and their identification merely serves as a form of risk stratification for anastomotic complications. In contrast, it is essential that surgeons are aware of the technical factors that affect the outcome of a colorectal anastomosis, because these are largely controllable (4,5).
The hallmark of a “perfect” colorectal anastomosis is one that is well-perfused, free of tension, and mechanically secure (6). The myriad of techniques and technologies that have been proposed to achieve this reflect the substantial heterogeneity in practice. The ideal anastomotic technique should not only be evidence-based, but also reproducible in routine practice. This review is meant to critically appraisal the practices described in the literature, and how we have applied them in our institution.
Discussion
Enhanced recovery after surgery (ERAS) is widely discussed in colorectal surgery since its implementation in 2012 (7). With the implementation of ERAS, traditional mechanical bowel preparation has been out of favour except in low rectal anastomosis with defunctioning ileostomy. A new concept of microbiome has been introduced whereby anastomotic contamination by digestive flora may result in anastomotic leak (8). In the last decade, studies show that the use of oral antibiotics preoperatively reduces the rate of anastomotic leak (9). A recent meta-analysis by Woodfield et al. with 35 randomised controlled trials (RCTs) comparing intravenous (IV) antibiotics with or without enema, IV antibiotic with oral antibiotics, mechanical bowel preparation, mechanical bowel preparation with IV and oral antibiotics, mechanical bowel preparation with oral antibiotics and oral antibiotics alone showed no difference in anastomotic leak rate among these groups (10). In our centre, only patients with low colorectal anastomosis with defunctioning ileostomy will have mechanical bowel preparation.
High ligation of the inferior mesenteric artery (IMA) was proposed by Miles, Moynihan, and Dukes in the early days of rectal cancer surgery to achieve adequate clearance of lymph nodes around the origin of the IMA (11-13). Dissection beyond that level, with excision of the periaortic lymph nodes, would likely not contribute to an improved survival given that a malignant node at this level would represent systemic spread of the disease. One of the most debated variations in technique would be the preservation of the left colic artery (LCA)—a low ligation of the IMA—as a means to improve the perfusion to a colorectal anastomosis. The proponents of a low ligation contend that marginal arteries may not be routinely sufficient to perfuse a colorectal anastomosis after a high ligation, and that the risk of malperfusion outweighs the oncological benefits of the latter (14).
While there have been several review articles published on this controversy, there have been relatively fewer prospective trials studying it. One RCT by Fujii et al. comparing high versus low IMA ligation in 331 patients undergoing anterior resection did not demonstrate any difference in anastomotic leak rate (15). Given the paucity of well-designed studies investigating the differences in IMA ligation, together with the heterogeneity of data and selection bias, meta-analyses on this topic have arrived at conflicting conclusions (16-20).
Some authors have proposed a more tailored approach to IMA ligation, only performing a high ligation for patients at risk of IMA nodal involvement (20,21). This is necessarily flawed given the limited accuracy with which nodal involvement can be predicted preoperatively. Other authors have attempted to preserve the blood supply of the LCA while achieving lymphatic clearance by combining a low ligation with lymphadenectomy around the IMA origin, at the expense of a slightly longer operative time. A meta-analysis by Yin et al. showed a reduced anastomotic leak rate in the low tie high dissection group (P<0.001), at the expense of a slightly longer operative time (P=0.06) and a lower yield of total lymph nodes (P=0.03). However, low ligation with IMA lymphadenectomy did not result in poorer 5-year oncological outcomes (22).
The authors routinely perform high ligation of the IMA for oncological resections involving the sigmoid and rectum. Firstly, this ensures complete lymphadenectomy based on a consistent anatomical landmark, using an easily reproducible method of dissection. Secondly, high ligation of the IMA ensures sufficient mobility of the proximal bowel to achieve a tension-free anastomosis. The length of viable bowel is less likely than its accompanying mesentery to limit its reach. By preserving the LCA, the mesentery of the proximal bowel is tethered by the remnant IMA, limiting its mobility especially in a low colorectal anastomosis.
Instead of potentially compromising oncological outcomes, or unnecessarily complicating an otherwise straightforward IMA ligation, the authors propose two practices that they have implemented as routine—splenic flexure mobilisation (SFM) and perfusion assessment using indocyanine green (ICG). SFM has been shown to significantly increase the length of the proximal colonic conduit, particularly when combined with high ligation of the IMA/inferior mesenteric vein (IMV) (23,24). Common reservations concerning routine SFM include added complexity of operation, prolonged operative time, and an increased risk of injury to vascular structures and adjacent organs (25,26). We routinely perform SFM as we feel that the advantage of minimising anastomotic tension outweighs the small penalty in operative time.
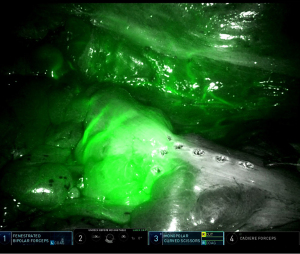
Adequate vascularity and tissue perfusion is no doubt another cornerstone of a successful anastomosis. Direct evaluation of this can be performed by visual inspection of cut bowel ends for healthy bleeding—this is rudimentary and arguably subjective. A more rigorous assessment is provided by the use of ICG to assess bowel perfusion. It has been established as safe and cost-effective without substantially increasing to the duration of surgery. There are differing results on ICG in prevention of anastomotic leaks. A meta-analysis by Blanco-Colino et al. comprising five non-randomized studies showed reduction of anastomotic leak in the ICG group (27). On the other hand, two randomized controlled studies did not show superiority of ICG in prevention of anastomotic leak (28,29). However, one of them had an inherent type 2 error due to inadequate sample size (29). One criticism is the varying results based on dosing, image acquisition device and observational biases (30). We advocate the use of ICG as an intravenous bolus of 0.1 mg/kg and visually confirm a transition point prior to bowel transection (Figure 1). We find that such a dose is safe, adequate for visualisation, and also allows for repeat dosing should further perfusion evaluation be necessary during later parts of the surgery.
Another practice that the authors have adopted to optimise perfusion is to perform side-to-end anastomoses. By securing the anvil of the circular stapler on the antimesenteric side of the proximal conduit, the authors hypothesise that there is a lower risk of attenuating the marginal blood supply. In patients who have undergone total mesorectal excision, a side-to-end J-pouch coloanal anastomosis potentially mitigates the symptoms of low anterior resection syndrome. While meta-analyses offer conflicting results on functional outcomes (31-33), most support the role of side-to-end anastomoses in reducing the risk of anastomotic leakage (34).
The other aspect of the ‘perfect’ anastomosis is its mechanical construct. While the widespread adoption of staplers in modern day colorectal surgery has brought about convenience and expedience, surgeons need to be mindful of the intricacies in fashioning such anastomoses. The authors make three recommendations with respect to the siting of the circular staple line in a colorectal anastomosis. Firstly, the circular stapler should be introduced towards the anti-mesenteric edge of the rectal stump in order to minimise the number of mesenteric blood vessels that are inadvertently divided by the stapler. Secondly, the circular stapler should also be sited towards one end of the rectal linear staple line (Figure 2) in a bid to incorporate one end of it within the resected ‘donut’ of the circular stapler. Studies have shown an association between anastomotic leaks and the number of staple cartridges used for rectal transection (35,36). One of the reasons for this is the vulnerability of staple line intersections. This second recommendation therefore serves to half the number of intersections between the circular and linear staple lines. For the same reason, in the event that multiple linear cartridges were required to complete the rectal transection, we recommend incorporating these intersections within the tissue that is to be resected by the circular stapler (Figure 3).
The integrity of the staple line is affected by the thickness (and consistency) of tissue across which it is fired, and the shaping of the staples against the anvil (37). When apposing the circular stapler to its anvil, we take care to ensure that extraneous tissue such as pericolic fat are excluded from the staple line. This ensures a uniform thickness of tissue throughout the entire circumference of the staple line, and also reduces the risk staple line bleeding.
A critical phase in a stapled anastomosis is the deployment of the stapler. One of the shortcomings of a manual circular stapler is the inadvertent movement of the stapler-anvil complex during the firing process, particularly in less experienced hands (38). It is postulated that such unwanted movements could result in micro-trauma and compromise the anastomosis (39). The powered circular stapler has been shown to mitigate this problem, and the authors have since incorporated its use to their practice (40).
Just as essential as the care put into the construct of the anastomosis are the secondary checks of orientation, tension, integrity and perfusion following its completion.
The use of ICG, methylene blue injection, sigmoidoscopic evaluation of the anastomosis, and air leak tests are well-described adjuncts for this purpose. A meta-analysis by Kryzauskas et al. reported lower leak rates in patients who had at least one of these tests performed (41). A prospective cohort study evaluating the use of trimodal testing (combining ICG perfusion check, tension testing, air- and methylene blue-leak tests) for left-sided colorectal anastomoses also concluded that such an approach allows for identification of anastomoses with early technical failure; allowing changes in the surgical plan where needed and finally culminating in an acceptable clinical leak rate (42). We routinely perform an on-table flexible sigmoidoscopy post-anastomosis, assessing ‘two sets of two’ items: firstly, anastomotic integrity as determined by the (I) visual confirmation on sigmoidoscopy of a complete and well-formed circular staple line, and (II) the absence of air leak, assessed by submerging the anastomosis under water in the pelvic cavity; secondly, anastomotic perfusion as determined by (I) the absence of mucosal malperfusion or demarcation, and (II) the absence of staple line bleeding.
Some other adjuncts for reinforcing the staple line for better apposition of tissue and added tensile strength have been described in the literature. Options include buttress with sutures, omentum, mesenteric flaps or synthetic materials (43). Fibrin and other associated sealants are purported to form a scaffold resistant to tension and compression while still remaining porous to cytokines and other immune cells essential for healing (44-47). Due to the questionable cost-benefit profile of these adjuncts, we do not utilise them in our routine practice.
This review article lacks quantitative data and analyses but aims to provide the reader with a review of the latest literature and discuss some of the controversies regarding the “perfect” colorectal anastomosis.
Conclusions
In summary, meticulous technique with nuanced refinements based on our understanding of surgical principles, together with the adoption of relevant new technologies, are essential in our strive towards the “perfect” colorectal anastomosis.
Acknowledgments
Funding: None.
Footnote
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-41/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-41/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patients for the publication of this study and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Branagan G, Finnis DWessex Colorectal Cancer Audit Working Group. Prognosis after anastomotic leakage in colorectal surgery. Dis Colon Rectum 2005;48:1021-6. [Crossref] [PubMed]
- Hu X, Guo P, Zhang N, et al. Nomogram for benign anastomotic stricture after surgery for rectal cancer. Asian J Surg 2023;46:111-9. [Crossref] [PubMed]
- Wako G, Teshome H, Abebe E. Colorectal Anastomosis Leak: Rate, Risk Factors and Outcome in a Tertiary Teaching Hospital, Addis Ababa Ethiopia, a Five Year Retrospective Study. Ethiop J Health Sci 2019;29:767-74. [PubMed]
- Kryzauskas M, Bausys A, Degutyte AE, et al. Risk factors for anastomotic leakage and its impact on long-term survival in left-sided colorectal cancer surgery. World J Surg Oncol 2020;18:205. [Crossref] [PubMed]
- Zarnescu EC, Zarnescu NO, Costea R. Updates of Risk Factors for Anastomotic Leakage after Colorectal Surgery. Diagnostics (Basel) 2021;11:2382. [Crossref] [PubMed]
- Goulder F. Bowel anastomoses: The theory, the practice and the evidence base. World J Gastrointest Surg 2012;4:208-13. [Crossref] [PubMed]
- Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for Perioperative Care in Elective Colorectal Surgery: Enhanced Recovery After Surgery (ERAS®) Society Recommendations: 2018. World J Surg 2019;43:659-95. [Crossref] [PubMed]
- Bachmann R, Leonard D, Delzenne N, et al. Novel insight into the role of microbiota in colorectal surgery. Gut 2017;66:738-49. [Crossref] [PubMed]
- Yue Y, Chen X, Wang H, et al. Mechanical bowel preparation combined with oral antibiotics reduces infectious complications and anastomotic leak in elective colorectal surgery: a pooled-analysis with trial sequential analysis. Int J Colorectal Dis 2023;38:5. [Crossref] [PubMed]
- Woodfield JC, Clifford K, Schmidt B, et al. Strategies for Antibiotic Administration for Bowel Preparation Among Patients Undergoing Elective Colorectal Surgery: A Network Meta-analysis. JAMA Surg 2022;157:34-41. [Crossref] [PubMed]
- Miles W. Cancer of the Rectum (The Lettsomian Lectures). London: Harrison and Sons; 1926.
- Moynihan B. The surgical treatment of cancer of the sigmoid flexure and rectum. Surg Gynecol Obstet 1908;6:463-6.
- Dukes CE. Peculiarities in the Pathology of Cancer of the Ano-Rectal Region. Proc R Soc Med 1946;39:763-5. [Crossref] [PubMed]
- Scott-Conner CEH. Chassin’s operative strategy in colon and rectal surgery. New York: Springer New York; 2006.
- Fujii S, Ishibe A, Ota M, et al. Short-term and long-term results of a randomized study comparing high tie and low tie inferior mesenteric artery ligation in laparoscopic rectal anterior resection: subanalysis of the HTLT (High tie vs. low tie) study. Surg Endosc 2019;33:1100-10. [Crossref] [PubMed]
- Nayeri M, Iskander O, Tabchouri N, et al. Low Tie Compared to High Tie Vascular Ligation of the Inferior Mesenteric Artery in Rectal Cancer Surgery Decreases Postoperative Complications Without Affecting Overall Survival. Anticancer Res 2019;39:4363-70. [Crossref] [PubMed]
- Yang Y, Wang G, He J, et al. High tie versus low tie of the inferior mesenteric artery in colorectal cancer: A meta-analysis. Int J Surg 2018;52:20-4. [Crossref] [PubMed]
- AlSuhaimi MA, Yang SY, Kang JH, et al. Operative safety and oncologic outcomes in rectal cancer based on the level of inferior mesenteric artery ligation: a stratified analysis of a large Korean cohort. Ann Surg Treat Res 2019;97:254-60. [Crossref] [PubMed]
- Wang Y, Wang Y, Zou L, et al. Does the level of inferior mesenteric artery ligation affect short-term and long-term outcomes of patients with sigmoid colon cancer or rectal cancer? A single-center retrospective study. World J Surg Oncol 2022;20:274. [Crossref] [PubMed]
- Zheng H, Li F, Xie X, et al. Preservation versus nonpreservation of the left colic artery in anterior resection for rectal cancer: a propensity score-matched analysis. BMC Surg 2022;22:164. [Crossref] [PubMed]
- Tjandra JJ, Kilkenny JW, Buie WD, et al. Practice parameters for the management of rectal cancer (revised). Dis Colon Rectum 2005;48:411-23. [Crossref] [PubMed]
- Yin TC, Chen YC, Su WC, et al. Low Ligation Plus High Dissection Versus High Ligation of the Inferior Mesenteric Artery in Sigmoid Colon and Rectal Cancer Surgery: A Meta-Analysis. Front Oncol 2021;11:774782. [Crossref] [PubMed]
- Kye BH, Kim HJ, Kim HS, et al. How much colonic redundancy could be obtained by splenic flexure mobilization in laparoscopic anterior or low anterior resection? Int J Med Sci 2014;11:857-62. [Crossref] [PubMed]
- Araujo SE, Seid VE, Kim NJ, et al. Assessing the extent of colon lengthening due to splenic flexure mobilization techniques: a cadaver study. Arq Gastroenterol 2012;49:219-22. [Crossref] [PubMed]
- Ferrara F, Di Gioia G, Gentile D, et al. Splenic flexure mobilization in rectal cancer surgery: do we always need it? Updates Surg 2019;71:505-13. [Crossref] [PubMed]
- Nowakowski M, Małczak P, Mizera M, et al. The Safety of Selective Use of Splenic Flexure Mobilization in Sigmoid and Rectal Resections-Systematic Review and Meta-Analysis. J Clin Med 2018;7:392. [Crossref] [PubMed]
- Blanco-Colino R, Espin-Basany E. Intraoperative use of ICG fluorescence imaging to reduce the risk of anastomotic leakage in colorectal surgery: a systematic review and meta-analysis. Tech Coloproctol 2018;22:15-23. [Crossref] [PubMed]
- De Nardi P, Elmore U, Maggi G, et al. Intraoperative angiography with indocyanine green to assess anastomosis perfusion in patients undergoing laparoscopic colorectal resection: results of a multicenter randomized controlled trial. Surg Endosc 2020;34:53-60. [Crossref] [PubMed]
- Jafari MD, Pigazzi A, McLemore EC, et al. Perfusion Assessment in Left-Sided/Low Anterior Resection (PILLAR III): A Randomized, Controlled, Parallel, Multicenter Study Assessing Perfusion Outcomes With PINPOINT Near-Infrared Fluorescence Imaging in Low Anterior Resection. Dis Colon Rectum 2021;64:995-1002. [Crossref] [PubMed]
- Guo J, Sim SK, Teo NZ, et al. Pitfalls of indocyanine green perfusional assessment in colorectal anastomosis. ANZ J Surg 2022;92:1602-5. [Crossref] [PubMed]
- McKechnie T, Sharma S, Daniel R, et al. End-to-end versus end-to-side anastomosis for low anterior resection: A systematic review and meta-analysis of randomized controlled trials. Surgery 2021;170:397-404. [Crossref] [PubMed]
- Fazio VW, Zutshi M, Remzi FH, et al. A randomized multicenter trial to compare long-term functional outcome, quality of life, and complications of surgical procedures for low rectal cancers. Ann Surg 2007;246:481-8; discussion 488-90. [Crossref] [PubMed]
- Rubin F, Douard R, Wind P. The functional outcomes of coloanal and low colorectal anastomoses with reservoirs after low rectal cancer resections. Am Surg 2014;80:1222-9. [Crossref] [PubMed]
- Hou S, Wang Q, Zhao S, et al. Safety and efficacy of side-to-end anastomosis versus colonic J-pouch anastomosis in sphincter-preserving resections: an updated meta-analysis of randomized controlled trials. World J Surg Oncol 2021;19:130. [Crossref] [PubMed]
- Park JS, Choi GS, Kim SH, et al. Multicenter analysis of risk factors for anastomotic leakage after laparoscopic rectal cancer excision: the Korean laparoscopic colorectal surgery study group. Ann Surg 2013;257:665-71. [Crossref] [PubMed]
- Balciscueta Z, Uribe N, Caubet L, et al. Impact of the number of stapler firings on anastomotic leakage in laparoscopic rectal surgery: a systematic review and meta-analysis. Tech Coloproctol 2020;24:919-25. [Crossref] [PubMed]
- Naoi D, Horie H, Sadatomo A, et al. The effect of staple height and rectal-wall thickness on anastomotic leakage after laparoscopic low anterior resection. Asian J Surg 2023;46:1577-82. [Crossref] [PubMed]
- Ethicon. PSB004770 Tissue Displacement and Deformation of Ethicon RENO (RENO) and Medtronic DST (DST) Circular Staplers on Harvested Porcine Colon. 2018. Available online: https://www.jnjmedtech.com/de-DE/product/ethicon-circular-stapler
- Pla-Martí V, Martín-Arévalo J, Moro-Valdezate D, et al. Impact of the novel powered circular stapler on risk of anastomotic leakage in colorectal anastomosis: a propensity score-matched study. Tech Coloproctol 2021;25:279-84. [Crossref] [PubMed]
- Teo NZ, Ngu JC. Clinical outcomes with a powered circular stapler for colorectal anastomoses: An initial experience with 25 consecutive cases. ANZ J Surg 2021;91:1949-50. [Crossref] [PubMed]
- Kryzauskas M, Bausys A, Jakubauskas M, et al. Intraoperative testing of colorectal anastomosis and the incidence of anastomotic leak: A meta-analysis. Medicine (Baltimore) 2020;99:e23135. [Crossref] [PubMed]
- Kryzauskas M, Bausys A, Dulskas A, et al. Comprehensive testing of colorectal anastomosis: results of prospective observational cohort study. Surg Endosc 2022;36:6194-204. [Crossref] [PubMed]
- Betzold R, Laryea JA. Staple line/anastomotic reinforcement and other adjuncts: do they make a difference? Clin Colon Rectal Surg 2014;27:156-61. [Crossref] [PubMed]
- Vakalopoulos KA, Daams F, Wu Z, et al. Tissue adhesives in gastrointestinal anastomosis: a systematic review. J Surg Res 2013;180:290-300. [Crossref] [PubMed]
- Huh JW, Kim HR, Kim YJ. Anastomotic leakage after laparoscopic resection of rectal cancer: the impact of fibrin glue. Am J Surg 2010;199:435-41. [Crossref] [PubMed]
- Tomori K, Eto K, Haruki K, et al. Comparison of Strength of Anastomosis Between Four Different Techniques for Colorectal Surgery. Anticancer Res 2020;40:1891-6. [Crossref] [PubMed]
- Paral J, Odlozilova S, Sirovy M, et al. Perioperative intrapelvic hyaluronate application as prophylaxis against complications following rectal anastomotic dehiscence: An experimental study. Asian J Surg 2022;45:1246-52. [Crossref] [PubMed]




