
Significant response from fruquintinib plus anti-PD-1 immunotherapy for microsatellite stable metastatic colorectal cancer with liver and lung metastasis in the third line: case report
Highlight box
Key findings
• A mismatch repair proficient/microsatellite stable (pMMR/MSS) metastatic colorectal cancer (mCRC) patient with lung and live metastases achieved PR and the longest progression-free survival of 28 months currently reported from fruquintinib plus anti-programmed cell death protein 1 immunotherapy.
What is known and what is new?
• Checkpoint inhibitor monotherapy is virtually inactive in MSS mCRC.
• Fruquintinib combined with immunotherapy could exert good therapeutic effects and safety in MSS mCRC patients.
What is the implication, and what should change now?
• This case demonstrated that patients with MSS mCRC could also benefit from immunotherapy combined with fruquintinib, providing a new and promising treatment option for some MSS mCRC patients.
Introduction
Colorectal cancer (CRC) is one of the most common malignant tumors with new cases reaching 940,000 worldwide every year. About 80% of CRC patients have developed distant metastasis at the time of diagnosis, and about 50% of patients that had objective responses still have postoperative recurrence and metastasis. Although metastatic CRC (mCRC) patients receiving systemic chemotherapy in first- and second-line settings generally have good response, geriatric and patients with decreased functional status are often not good candidates for chemotherapy and later-line treatment options are limited. Although the latest studies have reported that programmed cell death protein 1 (PD-1) antibodies (pembrolizumab, nivolumab, etc.) as first-line treatment in patients with mismatch repair gene deficiency (dMMR) mCRC were more effective than standard first-line chemotherapy combined with targeted therapy, and associated with significantly prolonged progression-free survival (PFS) (keynote-177) (1), mismatch repair proficient/microsatellite stable (pMMR/MSS) CRC patients did not benefit from PD-1 antibody therapy (2). Therefore, establishment of immunotherapy in pMMR remains a great importance.
In recent years, the exploration of various targeted drugs [such as epidermal growth factor receptor (EGFR) inhibitors, vascular endothelial growth factor (VEGF) inhibitors, B-Raf proto-oncogene (BRAF) inhibitors, etc.], and further combination with immunotherapy has become a popular and clinically important direction for exploring subsequent-line treatments for mCRC. Fruquintinib is a potent, highly selective small-molecule inhibitor of a vascular endothelial growth factor receptor (VEGFR)-1/2/3 that blocks the angiogenesis associated with tumor proliferation (3). Compared with placebo, fruquintinib has been shown to result in a statistically significant increase in overall survival (OS) for third and later line mCRC patients (9.3 vs. 6.6 months, P<0.001) (FRESCO trial) (4). In the phase 1b/2 trial, however, fruquintinib plus PD-1 inhibitor (FP) (sintilimab) for patients with MSS mCRC showed a remarkably longer survival with median PFS of 6.9 months and median OS of 14.8 months, compared to the phase Ib study of fruquintinib monotherapy with median PFS of 5.8 months and median OS of 8.8 months (5,6). Furthermore, preclinical studies in an MSS mouse model found that fruquintinib combined with immunotherapy could synergistically reduce angiogenesis and enhance the anti-tumor immune response (7,8). Thus, the combination of fruquintinib and PD-1 inhibitors may break the deadlock in MSS CRC patients with virtually no response to immunotherapy. This report shows that a patient with MSS mCRC achieved a significant response from fruquintinib plus anti-PD-1 immunotherapy as the third treatment line. We present this article in accordance with the CARE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-862/rc).
Case presentation
A 65-year-old male was admitted to Renji Hospital on August 10, 2018, due to recurrent hematochezia. Colonoscopy showed a 5 cm × 4 cm neoplasia of the rectum 3 cm from the anal verge, invading nearly 80% of the circumference. Pathology identified adenocarcinoma of the rectum. The patient immediately underwent Miles’ resection that is the optimal surgical operation for cancer involving the lowermost third of the rectum on August 16, 2018 (Figure 1). The postoperative pathology showed rectal mucinous adenocarcinoma, invading the outside of the plasma membrane and involving 9/14 lymph nodes, with no clear choroidal aneurysm embolus or nerve invasion. A diagnosis of stage IIIc (pT4aN2bM0) adenocarcinoma was suggested in this patient. Genetic testing suggested that RAS genes had no mutations. No single-nucleotide variants (SNVs) were detected in PMS2, MSH2, MSH6, or MLH1, suggesting pMMR, and the MSI status was stable (MSS). Immunohistochemistry (IHC) for several makers showed the following: (PD-L1) (0% positive), PD-1 (0% positive), ki-67 (70% positive), and p53 (++).
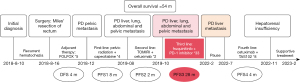
On September 19, 2018, the patient started postoperative treatment with the FOLFOX regimen (folinic acid, fluorouracil, and oxaliplatin) for 5 cycles. However, a computed tomography (CT) scan suggested diffuse thickening of pelvic mesangium with multiple lymph node metastases around bilateral iliac vessels. Disease-free survival (DFS) after surgery was 4 months. Then, the patient received first-line treatment with pelvic radiation therapy (2Gy/Fx, planned TD50Gy/25Fx), combined with oral chemotherapy with capecitabine (1 g bid d1–5, qw) from December 2018 to January 2019. The disease was stable until August 2019 with the first PFS (PFS1) of 8 months. The next CT scan found multiple metastasis including abdominal-pelvic, liver (maximum lesion diameter of 15 mm), lung (maximum lesion diameter of 31 mm), and small hilar mediastinal lymph nodes. The patient received second-line treatment with TOMIRI regimen (irinotecan and raltitrexed) plus cetuximab, just lasting for 2 cycles. A CT scan uncovered lesion progression again in October 2019 with the second PFS (PFS2) of 2 months.
At that time, the lesions in both lungs had increased in number and some had enlarged with a maximum diameter of 31 mm in inferior lobe of right lung (first image of Figure 2A). Multiple pathologic lymph nodes in the mediastinum and both lung hila had increased in number and size, with the longest diameter of around 41 mm (first image of Figure 2B). The largest lesion in the right lobe of the liver had also increased to 30 mm in size (Figure 3). Subsequently, starting from October 2019, patient received fruquintinib (3 mg d1–14 q21d) plus PD-1 inhibitor (sintilimab, 200 mg d1 q21d) (FP regimen) as third-line treatment, lasting for 33 cycles. After 3 cycles of treatment, the patient achieved a partial response (PR) in January 2020 (Figure 2). There was a partial reduction in the size of the lesions in both lungs and the enlarged lymph nodes in the mediastinum and both lung hila observed in a CT scan in January 2020, with the diameter of the largest lesions being reduced to 24 and 25 mm, respectively. The largest lesion of the liver was stable with a size of 33 mm (Figure 3A-3D). Then, the patient continued FP regimen and maintained PR. The lesions in the lung or the enlarged lymph nodes decreased continuously (Figure 2). Additionally, the tumor markers and related inflammatory factors also rapidly decreased and remained at normal levels after the third or fifth cycle of FP regimen (Figure 4). However, the maximum lesion of the liver with 33 mm in size started increasing from December 2021 (Figure 3E). Finally, the largest lesion of liver expanded to 60 mm in February 2022 and the patient was assessed with a progressive disease (PD) (Figure 3F). Despite all this, the patient achieved PR and had a significantly long PFS of 28 months from fruquintinib plus anti-PD-1 immunotherapy.



In addition, the patient tolerated the combined treatment of the FP regimen well. The patient never experienced bone marrow suppression, liver damage, hypothyroidism, myocardial damage, or immunotherapy-related pneumonia (Figure 5), and there were no grade 3 or higher other events. In January 2020, the patient had a urine protein level of 2+ and a 24-hour urine protein level of 1.0 g/24 h. This improved after starting losartan potassium tablets (1# Qd). Furthermore, the patient didn’t experience hypertension during the treatment of the combined regimen, so we couldn’t assume that the proteinuria was related to hypertension. Of note, there was renal impairment present prior to starting the third-line treatment and not to deteriorate. As fourth line treatment, the patient received 8 courses of TAS102 plus cetuximab until November 2022. Due to liver damage, the chemotherapy was suspended. Currently, the patient is under conservative supportive treatment. As of February 2023, the patient’s OS has reached 54 months from the initial diagnosis of rectal cancer.

All procedures performed in this study were in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Ethics Committee of Renji Hospital Affiliated to Shanghai Jiao Tong University School of Medicine (Shanghai, China) (No. CR2023-004). Written informed consent was provided by the patient and his family for publication of this report and any accompanying images. A copy of the written consent is available for review by the editorial office of this journal
International Multidisciplinary Team (iMDT) discussion
Discussion among physicians from Shanghai Renji Hospital
The pMMR/MSS subtype represents approximately 95% of mCRC. In recent years, a variety of anti-vascular targeting drugs (such as regorafenib, fruquintinib, etc.) have emerged to cover the treatment gap for advanced CRC at later-line settings. Currently, approved drugs include regorafenib, fruquintinib, and TAS-102, as guideline standard third-line treatment for MSS CRC (9,10). Additionally, a network meta-analysis (NMA) presented at the European Society for Medical Oncology (ESMO) 2022 may provide a reference for clinical applications (4,11-15). This analysis identified randomized controlled trials (RCT) of NMA through a systematic literature review conducted in February 2022, including 3 global or US-only RCTs (REDOs, RECOURSE, and CORRECT) and 4 Asia-only RCTs (FRESCO, TERRA, Yoshino 2012, and CONCUR) (4,11-15). The median PFS of different third-line treatments including fruquintinib, regorafenib of 80 mg, regorafenib of 160 mg, trifluridine-tipiracil (TAS-102), and the best supportive-care group for mCRC, was 3.9, 2.8, 2.1, 2.0, and 1.9 months, respectively. This meta-analysis revealed that fruquintinib had the longest median PFS and dominantly reduced the risk of disease progression or death, making it the preferred third-line option for advanced CRC in clinical practice.
Department of Oncology
However, the options for later-line treatment of mCRC are still limited. It is well known that immune checkpoint blockade therapy has achieved promising results in the treatment of dMMR/microsatellite instability-high (MSI-H) CRC, but checkpoint inhibitor monotherapy is virtually inactive in MSS mCRC (16-18). Therefore, there is an urgent need to explore more effective treatment options for MSS mCRC patients and find out the specific biomarkers. Several experimental studies have demonstrated that FP combination therapy decreased angiogenesis, enhanced normalization of vascular structure, increased infiltration and activation of CD8+ T cells, promoted pro-inflammatory subtype (M1)/anti-inflammatory alternatively activated subtype (M2) ratio of macrophages, decreased the ratio of myeloid-derived suppressor cells (MDSCs) and regulatory T cells in mice, and reprogrammed the immune microenvironment, thereby enhancing the antitumor effect (7,8). Thus, the efficacy of the new regimen (fruquintinib combined with immunotherapy) for MSS mCRC was further explored in more and more clinical practices.
In a phase 1b/2 trial, fruquintinib combined with a PD-1 inhibitor (sintilimab) for patients with MSS mCRC achieved a median PFS of 6.9 months [95% confidence interval (CI): 5.4–8.3] and a median OS of 14.8 months (95% CI: 8.8–not reached) (5). Also, the previous real-world studies of fruquintinib combined with PD-1 inhibitor for MSS mCRC with or without liver metastases showed that the median PFS (3.8, 95% CI: 2.8–4.8; 5.4, 95% CI: 4.0–6.8; or 5.5 months, 95% CI:3.5–7.5) and median OS (14.9, 95% CI: 7.6–21.7; or 10.5 months, 95% CI: not reached) were better than those achieved with the standard regimen of fruquintinib monotherapy to an extent (19-21). According to a recent study involving 8 cases of MSS colorectal extrahepatic metastases, a combination of immunotherapy and anti-vascular tyrosine kinase inhibitors (TKIs) targeting multiple sites can provide significant clinical advantages for patients with MSS CRC (22). All lung lesions in this observation study achieved PR, and the PFS ranged from 7 to 21 months. It was very similar to our case in which both lung lesions and mediastinal lymph nodes decreased significantly, and even the largest lesion in the lung decreased from 31 to 10 mm during treatment. Although this patient also had concurrent liver metastasis, the liver lesion under the treatment regimen remained stable for at least 26 months. We are pleased to report that they achieved the longest PFS of 28 months and the longest OS of 40 months among patients with MSS mCRC who have received fruquintinib plus sintilimab thus far.
Here, we also observed that interleukin-10 (IL-10) decreased after 3 cycles of fruquintinib treatment and the lung lesions shrank obviously in this case. M2 macrophages are the main inhibitory cells in the tumor microenvironment and regulate the response to anti-tumor therapy (23). and IL-10 is mainly secreted by the tumor and activates M2 through the IL-10 receptor of macrophages (24). The decrease of IL-10 may indicate the weakening of immune suppression and suggest that immunotherapy can exert anti-tumor effects. Together, some MSS CRC patients become the advantageous population for this combined regimen. Hence, we recommend fruquintinib combination immunotherapy for patients with MSS mCRC, especially with lung metastases, and patients with liver metastases are also recommended to this treatment if their economic status and physical strength are conducive. The local therapy to the liver may be indicated given the immune sink nature of liver metastases in colorectal cancer.
Department of nephrology
It is important to note that the recommended dosage for fruquintinib monotherapy is 5 mg, and a phase 1b/II study has confirmed the combination dosage of fruquintinib with PD-1 inhibitor. However, there is currently no available data regarding the use of fruquintinib in patients with renal impairment. Considering that this patient had renal dysfunction, we finally decided to administer a low dosage. During the treatment period, the patient had no other obvious side effects except for transient minor urinary protein, from which he quickly and fully recovered after receiving symptomatic treatment. Even the kidney dysfunction was not aggravated, and virtually remained at the original level. Despite being treated with the low dose, the patient achieved an excellent response and was very sensitive to the combination of fruquintinib and PD-1 inhibitor, which revealed that the patient was obviously the dominant candidate type for this regimen. Unfortunately, the patient did not receive treatment on time in January 2022 due to the COVID-19 outbreak, and the liver metastases had progressed significantly by the time of the review in February 2022.
Several issues on the treatment of this patient were further discussed as follows
Q1. What are the more promising individuals of the fruquintinib plus anti-PD-1 immunotherapy combination regimen for the treatment of MSS mCRC apart from patients with lung metastasis, such as other clinical or genetic features?
Expert opinion 1: Matteo Donadon
To date, fruquintinib plus anti-PD-1 in MSS mCRC patients should be considered in the context of clinical trials for those patients non-responders to the conventional regimens. It would be of great interest to consider basic and translational studies on in vivo and in vitro tumor models (for instances of colorectal liver metastases) to further understand the basic mechanisms behind their action.
Expert opinion 2: Francesco Mannavola
A paucity of prospective data exists to give a valid answer to this question, however it is plausible that combinations of fruquintinib and anti-PD1 inhibitors may be more useful in pre-treated MSS mCRC patients with RAS wild type and left sided tumors, especially in those with no liver metastases.
Q2. What are the current clinical indications or consensus for the option of fruquintinib plus anti-PD-1 immunotherapy exploration regimen or fruquintinib monotherapy for MSS mCRC patients?
Expert opinion 1: Matteo Donadon
Currently, there is no consensus on fruquintinib plus anti-PD-1 immunotherapy for MSS mCRC patients. More attention should be given and, as said before, clinical trials and basic studies should be planned. Potential candidates are those MSS mCRC patients non responders to others more standard treatments.
Expert opinion 2: Francesco Mannavola
Fruquintinib is a new generation TKI with high affinity to VEGFR-1/2/3 and significant clinical activity in patients with pretreated mCRC. Studies have shown that combination of fruquintinib and PD-1 inhibitors can synergistically inhibit the progression of colorectal cancer cells, change the tumor microenvironment, and promote immune antitumor activity (7,8). Patients with MSS mCRC failing previous line of therapies, including those who progressed under other antiangiogenic agents, otherwise not eligible to ICIs, are the ideal candidates for fruquintinib and immunotherapy combination in clinical trials. Although this regimen appears to be more effective in patients with lung metastases, those with liver disease should not be excluded from trials at this time.
Q3. Is there further guidance on the dose and course of the fruquintinib plus anti-PD-1 immunotherapy combination regimen, especially in patients with hepatic and renal impairment?
Expert opinion 1: Matteo Donadon
The experience on anti-PD1 immunotherapy in patients with liver and renal insufficiency is limited. While it is reasonable to modulate and reduce the dose in such patients, more experiences and more studies should be performed to answer that question.
Expert opinion 2: Francesco Mannavola
There are still no data on the safety of fruquintinib in case of impaired hepatic or renal function, while both hepatotoxicity and renal toxicity appear negligible. Pharmacokinetic studies have shown that fruquintinib is mostly metabolised in the liver, with subsequent biliary and renal-predominant excretion (25,26). While ICIs use is safe in case of impaired hepatic or renal function, fruquintinib should still be used with caution in these cases while awaiting data from ongoing trials.
Conclusions
The TKI targeting the VEGFR family, fruquintinib, combined with a PD-1 inhibitor (sintilimab) brought significant clinical benefits to this MSS mCRC patient, especially for the lung metastasis, which may be a breakthrough of immune unresponsiveness for the beneficiary individual with MSS CRC. The combination regimen was found to be well tolerated.
Acknowledgments
Funding: This project was supported by
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-862/rc
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-862/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-862/coif). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Diaz LA Jr, Shiu KK, Kim TW, et al. Pembrolizumab versus chemotherapy for microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer (KEYNOTE-177): final analysis of a randomised, open-label, phase 3 study. Lancet Oncol 2022;23:659-70. [Crossref] [PubMed]
- Zhou C, Cheng X, Tu S. Current status and future perspective of immune checkpoint inhibitors in colorectal cancer. Cancer Lett 2021; Epub ahead of print. [Crossref] [PubMed]
- Sun Q, Zhou J, Zhang Z, et al. Discovery of fruquintinib, a potent and highly selective small molecule inhibitor of VEGFR 1, 2, 3 tyrosine kinases for cancer therapy. Cancer Biol Ther 2014;15:1635-45. [Crossref] [PubMed]
- Li J, Qin S, Xu RH, et al. Effect of Fruquintinib vs Placebo on Overall Survival in Patients With Previously Treated Metastatic Colorectal Cancer: The FRESCO Randomized Clinical Trial. JAMA 2018;319:2486-96. [Crossref] [PubMed]
- Guo Y, Zhang W, Ying J, et al. Phase 1b/2 trial of fruquintinib plus sintilimab in treating advanced solid tumours: The dose-escalation and metastatic colorectal cancer cohort in the dose-expansion phases. Eur J Cancer 2023;181:26-37. [Crossref] [PubMed]
- Xu RH, Li J, Bai Y, et al. Safety and efficacy of fruquintinib in patients with previously treated metastatic colorectal cancer: a phase Ib study and a randomized double-blind phase II study. J Hematol Oncol 2017;10:22. [Crossref] [PubMed]
- Wang Y, Wei B, Gao J, et al. Combination of Fruquintinib and Anti-PD-1 for the Treatment of Colorectal Cancer. J Immunol 2020;205:2905-15. [Crossref] [PubMed]
- Li Q, Cheng X, Zhou C, et al. Fruquintinib Enhances the Antitumor Immune Responses of Anti-Programmed Death Receptor-1 in Colorectal Cancer. Front Oncol 2022;12:841977. [Crossref] [PubMed]
- Xu X, Yu Y, Liu M, et al. Efficacy and safety of regorafenib and fruquintinib as third-line treatment for colorectal cancer: a narrative review. Transl Cancer Res 2022;11:276-87. [Crossref] [PubMed]
- Dai Y, Sun L, Zhuang L, et al. Efficacy and safety of low-dose apatinib plus S-1 versus regorafenib and fruquintinib for refractory metastatic colorectal cancer: a retrospective cohort study. J Gastrointest Oncol 2022;13:722-31. [Crossref] [PubMed]
- Burnett H, Proskorovsky I, Yoon SS, et al. 400P Impact of regorafenib dose optimization on comparative outcomes in the treatment of relapsed/refractory metastatic colorectal cancer (mCRC)(J). Ann Oncol 2022;33:S719-S720. [Crossref]
- Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet 2013;381:303-12. [Crossref] [PubMed]
- Dasari A, Sobrero A, Yao J, et al. FRESCO-2: a global Phase III study investigating the efficacy and safety of fruquintinib in metastatic colorectal cancer. Future Oncol 2021;17:3151-62. [Crossref] [PubMed]
- Bekaii-Saab TS, Ou FS, Ahn DH, et al. Regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (ReDOS): a randomised, multicentre, open-label, phase 2 study. Lancet Oncol 2019;20:1070-82. [Crossref] [PubMed]
- Longo-Muñoz F, Argiles G, Tabernero J, et al. Efficacy of trifluridine and tipiracil (TAS-102) versus placebo, with supportive care, in a randomized, controlled trial of patients with metastatic colorectal cancer from Spain: results of a subgroup analysis of the phase 3 RECOURSE trial. Clin Transl Oncol 2017;19:227-35. [Crossref] [PubMed]
- Le DT, Kim TW, Van Cutsem E, et al. Phase II OpenLabel Study of Pembrolizumab in Treatment-Refractory, Microsatellite Instability-High/Mismatch Repair-Deficient Metastatic Colorectal Cancer: KEYNOTE-164. J Clin Oncol 2020;38:11-9. [Crossref] [PubMed]
- Andre T, Amonkar M, Norquist JM, et al. Healthrelated quality of life in patients with microsatellite instability-high or mismatch repair deficient metastatic colorectal cancer treated with first-line pembrolizumab versus chemotherapy (KEYNOTE-177): an open-label, randomised, phase 3 trial. Lancet Oncol 2021;22:665-77. [Crossref] [PubMed]
- Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017;18:1182-91. [Crossref] [PubMed]
- Gou M, Qian N, Zhang Y, et al. Fruquintinib in Combination With PD-1 Inhibitors in Patients With Refractory Non-MSI-H/pMMR Metastatic Colorectal Cancer: A Real-World Study in China. Front Oncol 2022;12:851756. [Crossref] [PubMed]
- Nie C, Lv H, Chen B, et al. Microsatellite stable metastatic colorectal cancer without liver metastasis may be preferred population for regorafenib or fruquintinib plus sintilimab as third-line or above therapy:A real-world study. Front Oncol 2022;12:917353. [Crossref] [PubMed]
- Zhang W, Zhang Z, Lou S, et al. Efficacy, safety and predictors of combined fruquintinib with programmed death-1 inhibitors for advanced microsatellite-stable colorectal cancer: A retrospective study. Front Oncol 2022;12:929342. [Crossref] [PubMed]
- Liu J, Li D, Han J, et al. Case Report: MSS colorectal extrahepatic (non-liver) metastases as the dominant population for immunotherapy combined with multi-target tyrosine kinase inhibitors. Front Oncol 2023;13:1091669. [Crossref] [PubMed]
- Mehla K, Singh PK. Metabolic Regulation of Macrophage Polarization in Cancer. Trends Cancer 2019;5:822-34. [Crossref] [PubMed]
- Myers KV, Amend SR, Pienta KJ. Targeting Tyro3, Axl and MerTK (TAM receptors): implications for macrophages in the tumor microenvironment. Mol Cancer 2019;18:94. [Crossref] [PubMed]
- Li K, Li X, Xia S, et al. Pharmacokinetics of fruquintinib in humans Clin Pharmacol Ther 2018;103:S86. [abstract no PII-116 plus poster].
- Zhou S, Shao F, Xu Z, et al. A phase I study to investigate the metabolism, excretion, and pharmacokinetics of [ 14C]fruquintinib, a novel oral selective VEGFR inhibitor, in healthy Chinese male volunteers. Cancer Chemother Pharmacol 2017;80:563-73. [Crossref] [PubMed]


