
Comparing laparoscopic and open resection in elderly hepatocellular carcinoma: a systematic review and meta-analysis
Highlight box
Key findings
• The key findings indicate that laparoscopic liver resection (LLR) is associated with significantly fewer complications, both major and minor, as well as a reduced incidence of postoperative ascites, and shorter length of hospital stay compared to open liver resection (OLR). No significant difference was found in long-term survival rates (overall survival and disease-free survival) between LLR and OLR.
What is known and what is new?
• Surgical resection, including LLR and OLR, is a primary curative strategy for hepatocellular carcinoma (HCC). The effectiveness and safety of these procedures in elderly patients, however, had not been comprehensively analyzed.
• This study provides new insights by specifically comparing LLR and OLR in elderly patients with HCC, highlighting the advantages of LLR in terms of lower complication rates and shorter hospital stays.
What is the implication, and what should change now?
• The findings suggest that LLR may be a safer and more suitable alternative to OLR for elderly patients with HCC. Given the reduced complications and shorter recovery time, clinicians and surgical teams should consider LLR as the preferred surgical approach in this demographic, enhancing patient care and potentially improving outcomes.
Introduction
Hepatocellular carcinoma (HCC) poses a significant global health challenge, ranking as the sixth most common malignancy worldwide and serving as a major contributor to cancer-related morbidity and mortality (1). Moreover, the global aging population has contributed to a rising number of elderly individuals diagnosed with HCC, highlighting the importance of this demographic group in disease management (2,3).
The therapeutic approach to HCC varies significantly, encompassing a spectrum of treatments, including transplantation, locoregional therapies, and surgical resection. The choice of treatment depends on factors such as the disease stage, extent, and the patient’s overall health (4,5). Among these options, surgical resection has emerged as a primary curative strategy for HCC, offering the potential for long-term survival and disease control (6-9). In the context of an aging population, a critical question arises: “What is the most effective and safest surgical approach for hepatocellular carcinoma in elderly patients?”
Two prominent surgical techniques for HCC resection are laparoscopic liver resection (LLR) and open liver resection (OLR). LLR, a minimally invasive surgery, has gained popularity over the last two decades due to its potential advantages, including reduced postoperative pain, shorter hospital stays, and faster recovery (9-11). In contrast, OLR represents the conventional surgical approach, affording the surgeon a direct and tactile perception of the liver, which allows for better control of bleeding and potential complications (12). The decision-making process regarding the choice of surgical approach is particularly complex in elderly patients who commonly have a unique set of challenges like comorbidities, compromised physiological reserves, and altered responses to surgical stressors (13). As the elderly population continues to grow, optimizing the management of HCC in this demographic becomes increasingly important.
This systematic review and meta-analysis aimed to fill the knowledge gap by systematically comparing the efficacy and safety of LLR and OLR for HCC in elderly patients (≥65 years). Through a comprehensive review and synthesis of existing evidence, we aimed to offer valuable insights that can assist clinicians and surgical teams in making informed decisions regarding the surgical approach for this specific patient population. We present this article in accordance with the PRISMA reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-67/rc).
Methods
The methods for selecting articles, conducting data analysis, and reporting the results of the meta-analysis were predetermined in the protocol. The protocol was registered on the PROSPERO (registration number CRD42022301691). Ethics approval for this study was waived from the IRB of National Evidence-based Healthcare Collaborating Agency (NECA).
Search strategy
We conducted a comprehensive search for studies comparing LLR with OLR in the treatment of elderly patients with HCC up until March 2022. We utilized the Ovid-Medline, Ovid-EMBASE, and Cochrane Library databases, with no restrictions on publication year or language. Our search strategy combined Medical Subject Headings (MESH) terms such as “hepatocellular carcinoma”, “aged”, and “hepatectomy” as well as related terms. To efficiently identify randomized controlled trials and observational studies, we applied the search filter recommended by the Scottish Intercollegiate Guidelines Network. Furthermore, we scrutinized the bibliographies of relevant articles to identify any additional publications. For a detailed breakdown of our search strategy and results for each database, please refer to the Tables S1-S3.
Inclusion and exclusion criteria
In our study, we focused exclusively on patients undergoing primary surgical treatment for HCC and did not include cases of re-hepatectomy. Two independent reviewers (J.J.Y. and S.R.) conducted an initial screening of titles and abstracts to exclude irrelevant studies. Subsequently, a thorough full-text review of potentially relevant articles was performed. The inclusion criteria were defined as follows: (I) studies focusing on elderly patients (≥65 years) with primary HCC; (II) comparative studies between LLR (laparoscopic or robotic) and OLR for elective surgical procedures; (III) studies reporting at least one of our predetermined outcomes of interest; and (IV) original, peer-reviewed articles that had been published. The exclusion criteria encompassed: (I) studies involving inappropriate populations, such as those with stage IV HCC, recurrent HCC or re-hepatectomy, liver metastasis, or specific situations like human immunodeficiency virus (HIV) infection; (II) studies related to emergency surgery or palliative treatment; (III) non-original articles, including reviews, editorials, letters, etc.; (IV) publications consisting solely of abstracts; (V) studies published in languages other than English or Korean; and (VI) duplicate publications. Any discrepancies in the review process were resolved through discussion and consensus, with the involvement of additional reviewers when necessary.
Data extraction and quality assessment
We employed the Methodological Index for Non-randomized Studies (MINORS) (14) to evaluate the quality of non-randomized surgical studies. Quality assessments were conducted independently by two researchers (D.A.P. and S.R.). Any discrepancies in assessment were resolved through consensus among all the authors. The data extraction encompassed the following categories: (I) study characteristics, including study design, country, study center, etc.; (II) participant characteristics, such as the disease, age cutoff point, stage, and proportion of males; (III) intervention details, including the type and scope of surgery; (IV) outcomes, which comprised survival outcomes at 3- and 5-year intervals, encompassing overall survival (OS) and disease-free survival (DFS), as well as post-operative mortality at 30 days, 90 days, and in-hospital, liver failure-related mortality, overall complication rate, major/minor post-operative complication rate, individual post-operative complications, including liver failure, heart failure, respiratory failure, renal failure, ascites, hemorrhage, wound infection, intra-abdominal abscess, re-operation rate, recurrence rate, re-hospitalization rate, and patient-reported outcomes. Major complications were defined as Clavien-Dindo grade III or higher, while minor complications were defined as Clavien-Dindo grades I–II. Additionally, we considered the descriptions provided by the authors of the primary research papers. Two independent reviewers extracted the variables listed above using a predefined data extraction form, and a double-check was performed to ensure accuracy. In cases where the primary research paper did not provide relevant data, we extracted survival rates and median survival times using the “Ungraph” program. To mitigate selection bias, we gave preference to extracting and utilizing matching data from matched studies.
Statistical analysis
Survival results were presented using descriptive statistics, relying on median survival time and 5-year survival rate data extracted from the literature. When applicable, we conducted meta-analyses employing a random-effects model, utilizing either the generic inverse variance method or the Mantel-Haenszel method to convey the impact of a variable on survival in terms of hazard ratios (HRs) or odds ratios (ORs) with accompanying 95% confidence intervals (CIs). To assess statistical heterogeneity, we employed Cochran and I2 statistics. Statistical heterogeneity was analyzed through a chi-squared test, with a significance threshold set at a P value <0.10 in the I2 test (15). An I2 value exceeding 50% was considered substantial evidence of statistical heterogeneity (16). Subgroup and sensitivity analyses were conducted to elucidate any heterogeneity among studies, when statistically significant, or to explore treatment effects based on specific study characteristics. Variables considered in the subgroup or sensitivity analysis included patient characteristics (age cutoff, tumor stage), intervention details [proportion of minor liver resection (LR)], general study characteristics (country, study design, number of adjusted variables), and methodological factors. Subgroup analyses were performed when there were five or more articles, as a small number of studies can yield misleading results. Sensitivity analysis was executed exclusively on matched studies and those with median MINORS scores. Unfortunately, a sensitivity analysis involving studies exclusively on super-elderly patients (>80 years) was infeasible due to a lack of relevant studies. For analyses involving more than 10 studies, we planned to assess publication bias and utilized the contour-enhanced funnel plot and Egger’s test. For conducting the meta-analysis, we utilized RevMan version 5.4 (The Cochrane Collaboration, Oxford, UK). The threshold for statistical significance was set at 5%.
Results
Study characteristics
We initially identified 2,736 potentially relevant studies from electronic databases and meticulously screened them, resulting in the selection of 222 studies for full-text review (Figure 1). Of these, 213 were excluded, leaving 9 studies included in this review. Table 1 offers an overview of these 9 studies, encompassing a total of 1,599 patients (17-25). All included studies were retrospective observational cohort studies. Notably, 8 of these studies employed propensity score matching analysis to compare LLR and OLR outcomes. Seven of the studies were conducted in Asian countries. Age criteria for defining elderly patients varied, with five papers (55.6%) using a cutoff of 70 years, while two papers (22.2%) used criteria of 75 and 65 years of age.
Table 1
| Author, year | Country/region | Study design | Study center | Enroll period | Study populations | Elderly criteria (years) | N (LLR/OLR) | Proportion of minor LR† | MINORS score | Robotic surgery | Hybrid approach | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| LLR | OLR | |||||||||||
| Monden, 2022 (17) | Japan | RC, PSM | Single center | 2010–2021 | Aged ≥70 years newly diagnosed with HCC who underwent LLR and OLR | 70 | 75/75 | 90.7% | 92.0% | 21 | Not mentioned | Excluded |
| Delvecchio, 2021 (18) | Europe | RC, PSM | Multi-center (n=8) | 2009–2019 | Elderly patients with HCC | 70 | 219/219 | 81.7% | 80.8% | 21 | Not mentioned | Not mentioned |
| Wen, 2021 (19) | China | RC, PSM | Single center | 2015–2018 | Patients over 65 years old who underwent liver resection | 65 | 71/71 | 94.4% | 91.5% | 21 | Not mentioned | Not mentioned |
| Chen, 2020 (20) | China | RC, PSM | Single center | 2013–2018 | Patients with primary HCC aged 70 years or older who underwent radical hepatectomy | 70 | 64/64 | 100% | 100% | 20 | Not mentioned | Not mentioned |
| Dumronggittigule, 2020 (21) | Korea | RC, PSM | Single center | 2003–2018 | HCC patients aged ≥70 years after hepatectomy | 70 | 41/41 | 53.7% | 56.1% | 21 | Excluded | Not mentioned |
| Kim, 2020 (22) | Korea | RC, PSM | Single center | 2013–2017 | Elderly patients with solitary treatment-naive HCC underwent liver resection | 65 | 96/160 | 51.1% | 56.0% | 21 | Excluded | Not mentioned |
| Nomi, 2020 (23) | Japan | RC, PSM | Multi-center (n=9) | 2010–2017 | Elderly patients who underwent liver resection for HCC | 75 | 155/155 | Mixed | Mixed | 21 | Not mentioned | Not mentioned |
| Goh, 2018 (24) | Singapore | RC, PSM | Single center | 2005–2016 | Consecutive patients who underwent LMH for HCC | 70 | 32/32 | 100% | 100% | 21 | Not mentioned | Not mentioned |
| Amato, 2017 (25) | Italy | RC | Single center | 2010–2014 | Elderly patients underwent hepatic resections for HCC | 75 | 11/18 | 100% | 88.9% | 19 | Not mentioned | Excluded |
†, minor LR: <3 adjacent segment resection. LLR, laparoscopic liver resection; OLR, open liver resection; LR, liver resection; MINORS, Methodological Index for Non-randomized Studies; RC, retrospective cohort; PSM, propensity score match; HCC, hepatocellular carcinoma; LMH, laparoscopic major hepatectomy.
Quality assessment
In the quality assessment of the included cohort studies, most of the 12 items received a rating of two points, with the exception of consecutive population sampling and prospective data collection (Figure S1). The median MINORS score for the assessed values in the 9 studies was 21 points.
OS
OS data were available in 5 papers, with median survival times identified in four of them, although the 50% survival rate reference point was not reached. In one study, the survival range was reported as 41.1 months in the LLR group and 39.1 months in the OLR group. Four papers provided data on the 3-year survival rates, ranging from 66.9% to 91.0% in the LLR group and 60.5% to 94.6% in the OLR group. For the 5-year survival rate, it ranged from 62.0% to 86.7% in the LLR group and 59.0% to 87.0% in the OLR group. Pooled analyses showed no significant difference between the two groups for both 3-year (HR =1.01; 95% CI: 0.99–1.02; I2=36%) and 5-year survival rates (HR =1.02; 95% CI: 0.99–1.06; I2=0) (Figure 2).
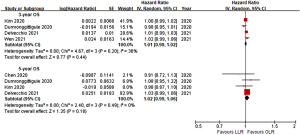
DFS
DFS data were available in five papers, and we extracted the 3- and 5-year DFS rates from papers. The 3-year DFS rate ranged from 48.1% to 71.5% in the LLR group and 49.3% to 58.1% in the OLR group. For the 5-year DFS rate, it varied from 43.4% to 66.0% in the LLR group and 30.8% to 57.0% in the OLR group. Pooled analyses indicated no significant difference between the two groups for both 3-year DFS (HR =1.00; 95% CI: 0.98–1.02; I2=0%) and 5-year DFS (HR =1.02; 95% CI: 0.99–1.05; I2=0%) (Figure 3).

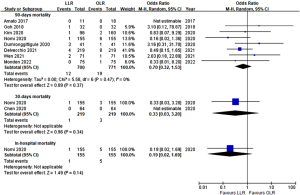
Post-operative short-term mortality
Eight studies provided data on the 90-day post-operative mortality rate, while two studies reported 30-day mortality, and one study reported in-hospital mortality. No significant differences were observed between the two groups in terms of 90-day post-operative mortality (OR =0.70; 95% CI: 0.32–1.53; I2=0%), 30-day mortality [OR =0.33; 95% CI: 0.03–3.20; I2= not available (NA)], and in-hospital mortality (OR =0.19; 95% CI: 0.02–1.69; I2= NA) (Figure 4). Subgroup analysis results for 90-day mortality across all subgroups based on cutoff age and LR type were consistent with the main findings (Table S4).
Post-operative complication rate
The overall complication rate was significantly lower in the LLR group compared to the OLR group (OR =0.53; 95% CI: 0.41–0.67; I2=0%, Figure 5A). Also, incidence of major complication was significantly lower in LLR group (OR =0.51; 95% CI: 0.35–0.74; I2=0%, Figure 5B). Subgroup analysis based on age cutoff, type of LR, and countries also showed consistent results (Table S5). Additionally, the post-operative minor complication rate was significantly lower in the LLR group than in the OLR group (OR =0.72; 95% CI: 0.54–0.94; I2=0%, Figure 5C).
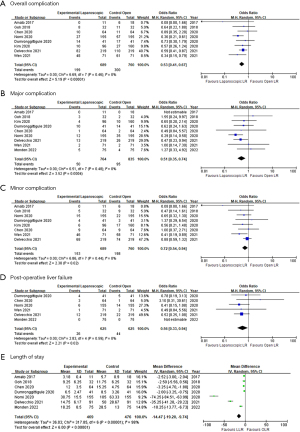
Post-operative individual complication rate
When considering specific complications, the incidence of post-operative liver failure was significantly lower in the LLR group compared to the OLR group (OR =0.56; 95% CI: 0.33–0.94; I2=0%, Figure 5D). In addition, it was possible to analyze the occurrence of ascites, wound infection, respiratory complication, bile leak, and bleeding (Table S6). The occurrence of ascites (OR =0.63), wound infection (OR =0.47), respiratory complication (OR =0.31), bile leak (OR =0.45), and bleeding (OR =0.65) all tended to be lower in the LLR group compared to the OLR group. Among these, the incidence of respiratory complications was statistically significantly lower in the LLR group (OR =0.31; 95% CI: 0.16–0.59; I2=0%).
Length of hospital stay
Regarding the length of stay (LOS), we identified 8 papers; however, a meta-analysis was not feasible due to most of them reporting median and range data. Nevertheless, all the studies consistently reported a significantly shorter hospitalization duration in the LLR group. Specifically, the median hospitalization periods for the LLR and OLR groups were 7 (range, 1–97) and 10 (range, 4–386) days, respectively. In an exploratory integrated analysis following data conversion, the LLR group exhibited a significantly shorter hospitalization period compared to the OLR group, although there was a high degree of heterogeneity among the studies (mean difference: −14.47 days; 95% CI: −19.20 to −9.74 days; I2=98%, Figure 5E).
Re-operation rate and re-hospitalization rate
Re-operation rates were reported in three studies. The meta-analysis showed no significant difference between the two groups, and there was moderate heterogeneity among the studies (OR =1.52; 95% CI: 0.12–18.96; I2=62%). Re-hospitalization rates were reported in one study, and no significant difference was observed between the two groups (OR =0.66; 95% CI: 0.11–4.02).
Sensitivity analyses
Sensitivity analysis limited to super-aged patients could not be conducted due to the absence of relevant studies. However, we proceeded with planned sensitivity analyses, which excluded two studies, resulting in outcomes similar to those observed in the main analysis (Figure S2). Notably, in these matched studies, the LLR group exhibited a significantly lower incidence of post-operative ascites compared to the OLR group (n=4 studies; OR =0.51; 95% CI: 0.34–0.76; I2=3%) (Figure S2). Finally, sensitivity analyses using studies with MINORS scores above the median (21 points), yielded results consistent with the findings of the overall analysis (Figure S3).
Discussion
This systematic review and meta-analysis aimed to assess the long-term prognosis and short-term post-operative outcomes of LLR in comparison to OLR in elderly patients with HCC. While previous meta-analyses have addressed HCC in elderly populations, our study specifically focused on patients aged ≥65 years, as defined by the World Health Organization, with primary HCC. We excluded studies with mixed populations, encompassing patients under 65 years of age or those with other liver malignancies like intrahepatic cholangiocarcinoma, liver metastases, or recurrent liver cancer. Previously, Jiang et al. (10) conducted a review and meta-analysis encompassing 14 studies comparing laparoscopic hepatectomy to open hepatectomy, while Wang et al. (9) performed meta-analyses using 12 propensity score-matched studies. Brolese et al. (11) reviewed eight studies comparing minimally invasive LRs (laparoscopic or robotic) to OLR. However, these previous systematic reviews included studies involving both adults and patients with primary or metastatic liver malignancies, potentially introducing variations in effectiveness and prognosis following surgical resection. Consequently, they do not offer precise insights into the clinical benefits of LLR compared to OLR in elderly HCC patients. Our study comprehensively assessed surgical safety, perioperative outcomes, long-term prognosis, and patient-reported outcomes associated with LLR versus OLR specifically for elderly HCC patients. We achieved this by selecting comparative studies, including recently published articles comparing LLR to OLR. As a result, our study incorporated the most up-to-date comparative surgical data, potentially providing valuable insights for surgical decision-making.
Our primary outcome of interest in this surgical treatment analysis was the OS rate among elderly patients with primary HCC. We aimed to gather comprehensive data by extracting results from survival curve plots for both the OS rate and DFS rates at the 3-year and 5-year points. Subsequently, we conducted descriptive statistics and an exploratory meta-analysis. Our analysis indicated that there was no significant difference in long-term survival between the two surgical approaches. These findings align with those of previous studies (9-11). However, it is important to note that further research is necessary to provide more detailed survival data and adjusted HR as time-to-event data, which can enhance the precision and depth of our understanding in this context.
In terms of overall and post-operative major complications, our meta-analysis indicated a decreasing trend in complications associated with LLR, which aligns with the findings of previous systematic reviews (9,10). Additionally, our analysis revealed that LLR was significantly linked to a lower rate of postoperative minor complications, a result consistent with the findings of Wang et al. (9). The smaller abdominal incision used in LLR can help maintain pulmonary function, facilitate early resumption of diet and ambulation, potentially contributing to reduced wound and pulmonary complications (26). In the realm of postoperative individual complications, our meta-analysis notably reported that LLR was associated with a lower rate of liver failure and ascites compared to OLR. These findings were further emphasized in sensitivity analysis, specifically when considering matching-design studies exclusively. During LLR, there is typically no need for complete mobilization of the liver, except in major LRs. This approach preserves collateral vessels and lymphatic channels around the liver. Additionally, LLR requires less manipulation, traction, and compression of the liver than OLR. All these factors contribute to the preservation of liver integrity and likely account for the lower rate of liver failure associated with LLR when compared to OLR (27).
This study found that the incidences of readmission and re-operation have been reported in very few studies. Specifically, regarding the re-operation rate, one out of the three results was contradictory, possibly attributed to the complexity of cases in the open surgery group and limitations in research design after matching. Thus, it is crucial to minimize the impact of selection bias on the outcome variable in future research. Furthermore, we observed that LLR was associated with significantly shorter hospitalization periods compared to OLR, with a difference of approximately 7 and 10 days, respectively. While this finding aligns with reports from previous meta-analyses, it is important to highlight that there was considerable heterogeneity in the exploratory meta-analysis that involved data conversion based on median and interquartile range, revealing an approximate difference of 14.5 days and an I2 statistic of 98%.
This systematic review and meta-analysis have several limitations that warrant acknowledgment. First, the inclusion of only non-randomized studies in the evaluation and pooled analysis posed challenges in obtaining results of optimal clinical relevance. Although many of the studies were matched retrospective cohort studies, it is important to recognize that this approach may not completely mitigate the inherent limitations and risk of selection bias associated with observational studies. Second, we encountered difficulty in clearly defining the age cutoff for elderly patients with HCC. While our intention was to conduct subgroup and sensitivity analyses with a cutoff age of >80 years, as defined in the primary studies, the scarcity of relevant literature limited our ability to explore age-specific effects thoroughly. Third, the majority of the included studies were single-center studies (80%) or conducted in Asian countries (70%). This imbalance in study settings and geographical locations can pose challenges to the generalizability of findings to broader populations. Fourth, our analysis faced limitations due to the lack of inclusion of non-elderly groups in many of the studies we reviewed. Consequently, a direct comparison between these two demographics was not feasible within the scope of our research. Regarding this topic, we are planning to publish a paper based on the results of additional meta-analysis research. Lastly, although we had intended to assess the impact of surgeon bias and operative variability in detail, most studies did not provide comprehensive details or standardized data in this regard. Consequently, it is advisable to interpret the findings of our study with caution, considering these limitations and potential drawbacks in the review process.
Conclusions
In conclusion, this study suggests that LLR may offer a safer and more suitable alternative to open surgery for elderly patients with HCC. LLR is associated with significantly fewer complications, both major and minor, as well as a reduced incidence of postoperative ascites, along with a shorter LOS compared to OLR. To establish the definitive advantages and risks of LLR over OLR in the treatment of elderly patients with HCC, future research should encompass long-term prospective controlled studies and randomized controlled trials that comprehensively assess clinical, oncological, and patient-reported outcomes.
Acknowledgments
Funding: This study was funded by
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-67/rc
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-67/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-67/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Ethics approval for this study was waived from the IRB of National Evidence-based Healthcare Collaborating Agency (NECA).
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Siegel RL, Miller KD, Fuchs HE, et al. Cancer statistics, 2022. CA Cancer J Clin 2022;72:7-33. [Crossref] [PubMed]
- Sung H, Ferlay J, Siegel RL, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 2021;71:209-49. [Crossref] [PubMed]
- Jang W, Lee HW, Lee JS, et al. Clinical characteristics and prognosis of Korean patients with hepatocellular carcinoma with respect to etiology. J Liver Cancer 2022;22:158-66. [Crossref] [PubMed]
- Korean Liver Cancer Association (KLCA) and National Cancer Center. (NCC) Korea. 2022 KLCA-NCC Korea practice guidelines for the management of hepatocellular carcinoma. J Liver Cancer 2023;23:1-120. [Crossref] [PubMed]
- Renne SL, Di Tommaso L. A clinical and pathological update on hepatocellular carcinoma. J Liver Cancer 2022;22:14-22. [Crossref] [PubMed]
- Cucchetti A, Sposito C, Pinna AD, et al. Effect of age on survival in patients undergoing resection of hepatocellular carcinoma. Br J Surg 2016;103:e93-9. [Crossref] [PubMed]
- Faber W, Stockmann M, Schirmer C, et al. Significant impact of patient age on outcome after liver resection for HCC in cirrhosis. Eur J Surg Oncol 2014;40:208-13. [Crossref] [PubMed]
- Kim JM, Cho BI, Kwon CH, et al. Hepatectomy is a reasonable option for older patients with hepatocellular carcinoma. Am J Surg 2015;209:391-7. [Crossref] [PubMed]
- Wang S, Ye G, Wang J, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in elderly patients: A systematic review and meta-analysis of propensity score-matched studies. Front Oncol 2022;12:939877. [Crossref] [PubMed]
- Jiang S, Yu D, He H, et al. Short- and Long-Term Outcomes in Laparoscopic Versus Open Hepatectomy for Hepatocellular Carcinoma in Elderly Patients: A Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A 2023;33:321-34. [Crossref] [PubMed]
- Brolese A, Rigoni M, Vitale A, et al. Role of laparoscopic and robotic liver resection compared to open surgery in elderly hepatocellular carcinoma patients: a systematic review and meta-analysis. Hepatoma Research 2020;6:34. [Crossref]
- Jo SJ, Rhu J, Kim JM, et al. Indications for open hepatectomy in the era of laparoscopic liver resection: a high volume single institutional study. J Liver Cancer 2022;22:146-57. [Crossref] [PubMed]
- Jang JY, Jung J, Lee D, et al. Stereotactic body radiation therapy for elderly patients with small hepatocellular carcinoma: a retrospective observational study. J Liver Cancer 2022;22:136-45. [Crossref] [PubMed]
- Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712-6. [Crossref] [PubMed]
- Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev 2019;10:ED000142. [Crossref] [PubMed]
- Higgins JP, Thompson SG, Deeks JJ, et al. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [Crossref] [PubMed]
- Monden K, Sadamori H, Hioki M, et al. Short-term outcomes of laparoscopic versus open liver resection for hepatocellular carcinoma in older patients: a propensity score matching analysis. BMC Surg 2022;22:63. [Crossref] [PubMed]
- Delvecchio A, Conticchio M, Ratti F, et al. Laparoscopic major hepatectomy for hepatocellular carcinoma in elderly patients: a multicentric propensity score based analysis. Surg Endosc 2021;35:3642-52. [Crossref] [PubMed]
- Wen N, Liu F, Zhang H, et al. Laparoscopic liver resection for hepatocellular carcinoma presents less respiratory complications compared with open procedure: A propensity score analysis in the elderly. Eur J Surg Oncol 2021;47:2675-81. [Crossref] [PubMed]
- Chen Y, Yu L, Quan C. Laparoscopic versus open hepatectomy for elderly patients with hepatocellular carcinoma. J BUON 2020;25:1404-12. [PubMed]
- Dumronggittigule W, Han HS, Ahn S, et al. Laparoscopic versus Open Hepatectomy for Hepatocellular Carcinoma in Elderly Patients: A Single-Institutional Propensity Score Matching Comparison. Dig Surg 2020;37:495-504. [Crossref] [PubMed]
- Kim JM, Kim S, Rhu J, et al. Elderly Hepatocellular Carcinoma Patients: Open or Laparoscopic Approach? Cancers (Basel) 2020;12:2281. [Crossref] [PubMed]
- Nomi T, Hirokawa F, Kaibori M, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in elderly patients: a multi-centre propensity score-based analysis. Surg Endosc 2020;34:658-66. [Crossref] [PubMed]
- Goh BKP, Chua D, Syn N, et al. Perioperative Outcomes of Laparoscopic Minor Hepatectomy for Hepatocellular Carcinoma in the Elderly. World J Surg 2018;42:4063-9. [Crossref] [PubMed]
- Amato B, Aprea G, De Rosa D, et al. Laparoscopic hepatectomy for HCC in elderly patients: risks and feasibility. Aging Clin Exp Res 2017;29:179-83. [Crossref] [PubMed]
- Han DH, Choi SH, Park EJ, et al. Surgical outcomes after laparoscopic or robotic liver resection in hepatocellular carcinoma: a propensity-score matched analysis with conventional open liver resection. Int J Med Robot 2016;12:735-42. [Crossref] [PubMed]
- Belli A, Cioffi L, Russo G, et al. Liver resection for hepatocellular carcinoma in patients with portal hypertension: the role of laparoscopy. Hepatobiliary Surg Nutr 2015;4:417-21. [PubMed]



