Outcome of young patients with rectal adenocarcinoma
Introduction
Recent epidemiological studies have emphasized an increase in the incidence of rectal adenocarcinoma in young patients, especially in Asian countries like India (1). Series published in rectal carcinoma (RC) showed proportions of affection in young patients between 3% and 31% (2). There is not until now a consensus in the literature on the definition of age to consider a patient with RC as a young, but published cut points vary between 35 and 50 years old. There are conflicting studies about survival of young patients with RC in western countries, with some studies suggesting a worse prognosis for young patients, while other studies show no differences in cancer outcomes among young patients and older patients with RC (3,4). In our country there is no information about the incidence of carcinoma in young people. In this study we analyzed the histopathologic features and oncological outcomes of patients with rectal adenocarcinoma in patients younger than 40 years compared with those over 40 years. The main objective of the study was determine if the 5-year overall survival is different according the age of the patients, our hypothesis is that young patients with rectal cancer (≤40 years) have similar (statistically insignificant difference) 5-year overall survival respect older patients (>40 years).
Methods
We analyzed the histopathologic features of 175 patients diagnosed with rectal adenocarcinoma (24 patients with less than or equal to 40 years old and 151 patients older than 40 years 1 day) at our institution, between January 2009 and December 2013. All patients were discussed in an interdisciplinary collegial group and those with tumors clinically T3, T4 and/or positive lymph nodes (LNs) received preoperative chemoradiotherapy (pCRT) followed by surgery, while the remaining patients underwent surgery directly. The pCRT scheme was 45 Gy to the pelvis more overprinting of 5.4 Gy given in 5 weeks plus the chemotherapy schema with 3–5 cycles of 5-fluorouracil (5-FU) before surgery. The decision on the surgical approach was based on tumor characteristics, economic preferences of the patient and hospital needs. The surgical specimen was assessed by systematically recommended by Quirke (5) and validated in our institution (6). After surgery, patients were followed with the start of pCRT as starting point and with the date of their last visit or death as stop of the follow up. Recurrences were categorized as loco regional if they were in the anastomosis site or in the pelvis and distant if they were located in para-aortic LNs, liver, lung or other distant organs. For purposes of our study, we define as rectal adenocarcinoma in young the cases that occurred in patients aged 40 years or below. Statistical analysis was performed using the statistical package SPSS Statistics® (SPSS Inc., version 22, Armonk, New York, IL, USA). Survival analysis was performed using the Kaplan-Meier method. Chi-square test or Fisher’s exact test were used to compare means of variables when it was the case with a P value of <0.05 for statistical significance.
The study was approved by the ethics committee/research committee of our institution.
Results
Demographic and histopathologic features
The characteristics evaluated and compared between groups are summarized in Table 1. Of the 175 patients, 24 (13.7%) were under 40 years old. The group of young patients showed higher prevalence of tumors in advanced stage (clinical stage III and IV 54.2% vs. 44.4%, P=0.054), more poorly differentiated tumors (grade 3 in 25% vs. 13.2%, P=0.038) and increased frequency of tumors with luminal obstruction requiring a derivative colostomy (9% vs. 3.2%, P=0.001); compared with tumors in patients older than 40 years. The vast majority of tumors in the series were of conventional type (intestinal without another specification) in 135 (77.1%) cases, 23 (13.1%) cases were mucinous, 11 (6.3%) cases showed cribriform pattern and 6 cases showed signet ring cell morphology. An interesting observation is that five of the six cases with signet ring cells were present in patients younger than 40 years. The proportion of patients who received pCRT was similar between the two groups (83.3% vs. 82.1%).
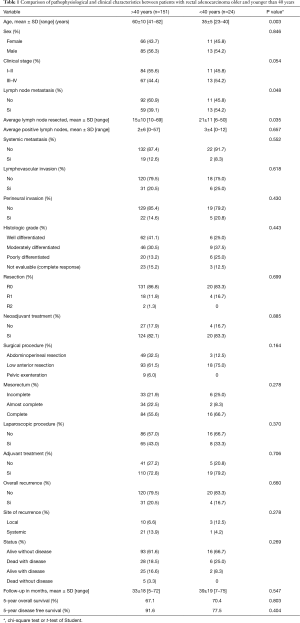
Full table
Pathologic complete response was observed in 3 (12.5%) of patients younger than 40 years and in 23 (15.2%) of patients older than 40 years. There were no statistical differences between the rates of pathologic response to pCRT between the two groups of patients. The type of surgical treatment in the group of >40 years patients showed abdominoperineal resections (32.5% vs. 12.5%) and pelvic exenterations (6% vs. 0%) in more cases compared to patients younger than 40 years. The use of laparoscopic surgery was higher in the group of patients >40 years (43% vs. 33.3%). The mesorectum was adequately resected (complete and almost complete mesorectum) in 78.1% of patients over 40 years and in 75% of patients younger than 40 years. Complete resection R0 was obtained in 86.8% of patients in the group >40 years and was slightly lower in the group of patients younger than 40 years (83.3%). Patients undergoing surgery without pCRT had a higher pT stage in patients younger than 40 years, also the number of patients with LN metastasis was higher in this group (54.2% vs. 39.1%, P=0.048) and the nodal stage was higher. The average number of dissected LNs in patients younger than 40 and older than 40 years was 21 (range, 6–50) and 15 (range, 10–69), respectively (P=0.035). The average of positive nodes in the pathological examination was 3 (range, 0–12) in the age group under 40 years old and 2 (range, 0–57) in the group over 40 years.
Oncologic results
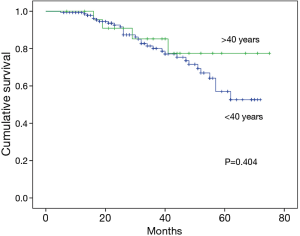
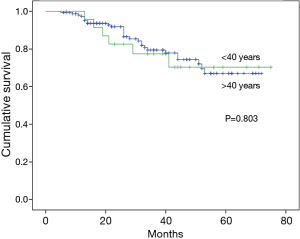
The overall recurrence rate was 16.7% in less than 40 years, and 20.5% in the group increased to 40 years group; however, the type of recurrence was different between the two groups. Local recurrence was higher in the group of <40 years (12.5% vs. 6.6%), whereas systemic recurrence was higher in the group of patients older than 40 years (13.9% vs. 4.2%). The recurrence-free survival at 5 years was 91.6% for patients over 40 years, compared with 77.5% for patients younger than 40 years, however, this difference was not statistically significant (P=0.404) (Figure 1). Overall survival at 5 years was similar in both study groups, with 67.1% for patients over 40 years and 70.4% for those under 40 years (P=0.803), with a mean follow up of 33.5±18 months (Figure 2). In multivariate analysis of the total study population (n=175) factors demonstrated independently affect the survival of patients are shown in Table 2, of which the only ones who showed association with decreased survival were incomplete resection (P=0.004) and absence of pCRT (0.036). The presence of recurrence overall trend also demonstrated statistical correlation with worse survival (P=0.058). The rest of the factors analyzed, including age showed no independent prognostic value.
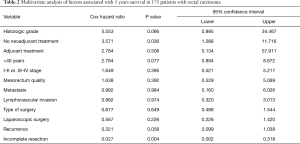
Full table
Discussion
The proportion of young patients with rectal adenocarcinoma in our population is 13%, intermediate between Asian series where around 30% (1) and greater than European populations (3%) (2), but similar to that observed in the United States (20%) (4). Our analysis of the characteristics of tumors young patients vary significantly in the number of dissected lymph largest and most pN stage, compared with the group of elderly patients. Also young patients in our series show a higher incidence of grade 3 tumors, a fact that has been previously reported in the literature (1,3). The incidence of histological subtype of signet ring cells in our study was markedly lower than Japanese studies (7), but five of six cases with this morphology in our series occurred in the group of patients younger than 40 years. In epidemiological studies in the literature has been postulated that young patients are more likely to receive pCRT when compared to its counterparts >40 years, however, in our study this difference was not found, although the younger patients are presented in advanced stage in a larger proportion. The highest rates of recurrence during treatment in our study in young patients may reflect aggressive tumor biology in these patients. Interestingly, the local recurrence rate was higher in the group of young patients, a fact that may be explained by the higher number of incomplete and more likely to mesorectal incompletely resected found in the group of patients younger than 40 years in our series resections. It should be noted that the presence of R1 and R2 resections in our population is due to involucre of circumferential margin in 100% of cases, a characteristic that is determined by both intrinsic characteristics of the tumor and the incomplete mesorectal excision (8). Our findings of increased LNs and increased number of positive nodes in young patients is similar to what has previously been found in a study by the SEER base of the United States of colon cancer (9). Although a high proportion of the patients presented with advanced disease, disease-free survival and overall survival at 5 years between young people and the elderly population they were not statistically different. An analysis of the SEER database showed no statistically significant difference in overall and disease-free survival at 5 years between a cohort of young and elderly patients (63.2% vs. 62%, respectively) (3). You and colleagues reported that there were no statistically significant differences in survival stage by stage between younger and older patients (overall 5-year survival for stage III of 69% vs. 74%, respectively) (4). Data of the aforementioned studies are according to our findings.
Conclusions
We found no statistically significant difference in overall 5-year survival and recurrence rates between patients younger than 40 years and older than this age, although the patients younger than 40 years showed higher clinical stage, higher nodal stage, high proportion of grade 3 tumors, high frequency of positive margins and recurrence. The pessimism associated with rectal cancer in young patients should be avoided and they should be treated the same way as older patients according to the clinical stage.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The study was approved by the ethics committee/research committee of our Institution/Instituto Nacional de Cancerología (No. 15/129) and written informed consent was not necessary because the retrospective/observational nature of the study and data does not contain identifying information of the patients.
References
- Nath J, Wigley C, Keighley MR, et al. Rectal cancer in young adults: a series of 102 patients at a tertiary care centre in India. Colorectal Dis 2009;11:475-9. [Crossref] [PubMed]
- Orsini RG, Verhoeven RH, Lemmens VE, et al. Comparable survival for young rectal cancer patients, despite unfavourable morphology and more advanced-stage disease. Eur J Cancer 2015;51:1675-82. [Crossref] [PubMed]
- O'Connell JB, Maggard MA, Liu JH, et al. Are survival rates different for young and older patients with rectal cancer? Dis Colon Rectum 2004;47:2064-9. [Crossref] [PubMed]
- You YN, Dozois EJ, Boardman LA, et al. Young-onset rectal cancer: presentation, pattern of care and long-term oncologic outcomes compared to a matched older-onset cohort. Ann Surg Oncol 2011;18:2469-76. [Crossref] [PubMed]
- Quirke P, Steele R, Monson J, et al. Effect of the plane of surgery achieved on local recurrence in patients with operable rectal cancer: a prospective study using data from the MRC CR07 and NCIC-CTG CO16 randomised clinical trial. Lancet 2009;373:821-8. [Crossref] [PubMed]
- Lino-Silva LS, Molina-Frías E, Salcedo-Hernández RA, et al. Relevance of an adequate pathologic evaluation of radical rectal resection specimens. Acta Gastroenterol Latinoam 2013;43:198-205. [PubMed]
- Sasaki S, Masaki T, Umetani N, et al. Characteristics in primary signet-ring cell carcinoma of the colorectum, from clinicopathological observations. Jpn J Clin Oncol 1998;28:202-6. [Crossref] [PubMed]
- Baik SH, Kim NK, Lee KY, et al. Factors influencing pathologic results after total mesorectal excision for rectal cancer: analysis of consecutive 100 cases. Ann Surg Oncol 2008;15:721-8. [Crossref] [PubMed]
- Wang L, Hollenbeak CS, Stewart DB. Node yield and node involvement in young colon cancer patients: is there a difference in cancer survival based on age? J Gastrointest Surg 2010;14:1355-61. [Crossref] [PubMed]


