Less than 12 lymph nodes in the surgical specimen after neoadjuvant chemo-radiotherapy: an indicator of tumor regression in locally advanced rectal cancer?
Introduction
The importance of adequate staging of colorectal cancer for oncological outcomes is highlighted by the management guidelines. Survival impact of lymph node ratio (LNR) (number of metastatic lymph nodes to total number of nodes examined) has been proven to be an independent prognostic indicator in various recent studies, with low LNR shown to have a better survival (1-3). Survival advantage of higher total number of lymph nodes examined in the surgical specimen has been reported (4). The actual lymph node yield shows wide variation as reported in literature (5,6). Presence of at least 12 lymph nodes in surgical specimen is recommended by the American Joint Committee on Cancer (AJCC) and UIAC to ratify the competence of surgery for colorectal cancer, and it has been accepted universally as the standard in the colorectal cancer treatment based on two hypotheses (7-10). First, the accurate staging is an important subset in the treatment protocol in rectal cancer. Second, more precise surgery with higher number of lymph node clearance improves the local control of the disease. This cut-off value is looked as an indicator of quality of surgery and a proxy for adequate surgery, and considered as an important prognostic factor (11-13).
Consequently, fewer than standard recommended lymph nodes have hypothesised to be due to either an inadequate disease removal by the surgeon, or nodes missed from being picked up in the surgical specimen by the pathologist. This might also be due to a reduction in the size and numbers of lymph nodes with chemo radiotherapy (CRT) (14).
The rectal cancer is rather different from colon cancer regarding lymph node metastasis due to its anatomical configuration and circumferential by mesorectum with the fascial inclination. Nevertheless, circumferential radial margin has as much importance as the distal mucosal margin. Higher local recurrence rates in locally advanced rectal cancers have leads to an increased use of pre-operative radiotherapy with or without chemotherapy. Preoperative treatment empirically downstages the primary tumor and the lymph nodes covered in the radiation field as well. Therefore, preoperative CRT followed by routine total mesoractal excision (TME) has become the standard protocol of treatment in locally advanced rectal cancer (15). At our centre, we noticed a paucity of lymph node yield in patients undergoing resection after preoperative CRT in rectal cancer. There are several factors affecting the number of harvested lymph nodes, including radiation technique, radiation dose, tumor responsiveness to radiotherapy and use of additional chemotherapy, etc. High lymph node yield after pre-operative CRT denotes a compromised radiation field and poor response of the tumor.
The standard surgical technique of TME for proximal rectum and partial TME for the lower rectal cancer would have resulted in high variability of the number of lymph nodes in post CRT patients (14,16). This contemplates the presence of the few lymph nodes in the mesorectum due to neoadjuvant treatment. We propose this study as an orientation, which might help to revise the future guidelines regarding the lymph node yield for proper staging of rectal cancer patients who received neoadjuvant CRT. We also investigated that lower total number of lymph nodes in the TME specimen after CRT is a marker of better tumor response.
Methods
Patients
A prospectively sustained, institutional, confidential record of patients with rectal cancer was probed to identify patients undergoing total mesorectal excision after neoadjuvant CRT for the primary rectal adenocarcinoma between January, 2010 and December, 2014. For each patient, demographics, preoperative diagnosis, clinical staging, preoperative chemo-radiotherapy schedule, dose and duration, post neoadjuvant treatment response, operative course, intraoperative events and follow-up assessment were documented. Exclusions included patients who, on presentation had metastatic disease, recurrent cancer, and previous pelvic surgery and radiation. Patients who underwent local excision and who had followed up less than 12 months also excluded. A total of 92 patients were included with full database and retrospectively analysed.
Pre-treatment assessment
At the initial evaluation, clinical and digital rectal examination (DRE), colonoscopy with biopsy, chest radiography and computed tomography (CT) of the abdomen and pelvis to confirm the diagnosis were done. Pathological confirmation was performed on tissue biopsy of the primary lesion. Magnetic resonance imaging (MRI) of the pelvis was performed to stage the local transmural extension and nodal status for all patients. In addition to that, blood cell count, serum biochemistry including liver and renal function tests and serum CEA levels were obtained. Patients with suspected distant metastasis underwent image guided biopsy and positron emission tomography if possible. Clinical stages were recorded according to the AJCC Staging System, seventh edition (7).
Neo-adjuvant treatment
All patients who had clinical or radiological stage T3, T4 with N0 or N+ received whole pelvis radiotherapy with doses 45 to 54 Gy at 1.8 Gy per fraction in prone position. Local tumor boost radiation was given to patients with cT4 category, as a sequential boost on the primary tumor and corresponding mesorectum with a concomitant dose of 10 Gy (twice in a week, total ten fractions immediately after the daily dose), over five weeks. Radiotherapy was delivered for five sessions per week.
During preoperative radiotherapy, patients who had T4 and N+ stage also received chemotherapy concurrently as per institutional protocol. The chemotherapy regimens used were 5-FU and leucovorin (FL) (n=11) and capecitabine (n=14).
Treatment response
All patients underwent CECT abdomen with pelvis after 4 weeks of completion of neoadjuvant treatment. Serum CEA levels were also performed for all patients. The grade of tumor regression was recorded based on abnormal surface area, size or longitudinal extent of lesion and intramural involvement. Radiological TRG is classified as (17):
- Complete: no residual tumor, no surface abnormality, no induration;
- Good: barely perceptible, 75% or greater reduction in surface abnormality and induration;
- Moderate: 25% to 75% reduction in surface abnormality and induration;
- Minimal: less than 25% reduction in surface abnormality and induration;
- No change: no change in surface abnormality and induration.
Surgical treatment
At our institute, the assessment for surgery usually starts at four weeks’ completion of neoadjuvant treatment to decide the timing of surgery. All patients were planned for surgical exploration after 4 weeks of completion of neoadjuvant treatment with anaesthetic fitness under ASA class I–III. Mean interval between completion of neoadjuvant treatment and surgery was 7 weeks (range, 4–11 weeks) in this study. Forty-six patients (50.5%) underwent low anterior resection, 41 patients (45.5%) underwent abdominoperineal resection and 4 patients (4%) had pelvic exenteration. Laparoscopic surgery was done in 8 patients (9%). The technique of resection was standardized and all patients underwent TME or partial TME with preservation of the hypogastric nerves.
Surgical pathological assessment
Pathological examination of the specimen was done by the qualified pathologist with manual dissection of the mesenteric and mesorectal fat of the specimen in whole length. During latter half of this study, in our institution the fat clearing technique and lymph node harvesting immediately after surgery followed by submission of the specimen in formalin to the pathologist was followed. Pathologist performed a second attempt to harvest the lymph nodes from the specimen. Each pathological slide was assessed by the consultant pathologist qualified in onco-histopathology. Pathological staging done according to AJCC 7th edition (7). Pathological parameters included tumor transmural extension, tumor differentiation, depth of tumor penetration, lymph node metastasis, circumferential resection margin (CRM), lymphovascular invasion, and tumor regression grade (TRG) as suggested by Mandard et al. (18). Positive CRM is defined as the presence of tumor microscopically at the outermost margin of the lesion or <1 mm depth of the circumferential surface of the specimen. Patients were categorized into two groups based on the number of total harvested lymph nodes with group 1, having 12 or more nodes harvested, and group 2 including patients who had <12 lymph nodes harvested.
Follow up
Clinical examination was performed at every 3 months for the first year, every 6months for the next 2 years, and then annually. Serum CEA level, liver function test, chest X-ray and liver ultrasound performed at every 3 months for the first year and then 6 monthly. At every 6 months, pelvic CT was obtained for all patients and colonoscopy was performed at 1 and 3 years. The occurrence of recurrent lesion in the pelvis, perineum and at the anastomosis was considered as local recurrence, while any other areas considered as distant metastasis. Recurrence was confirmed cytologically or histologically for all cases. Disease free survival was calculated from the time of surgery to appearance of the recurrence. Overall survival was calculated from the day of diagnosis to death.
Statistical analysis
The analysis was done with SPSS statistical software version 20.0 for Windows. Continuous variable (e.g., age, BMI, distal margin from anal verge, time interval, number of lymph nodes, etc.) groups were compared independent t test and chi-square test performed for the proportions (e.g., gender, TNM stage, neo-adjuvant treatment, TRG, ypTNM stage, LNR, etc.). Quantitative and ordinal variables were compared (e.g., number of lymph nodes) with Mann-Whitney test. The value of P≤0.05 was considered statistically significant.
Results
Patient characteristics
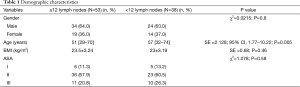
One-hundred-two patients underwent surgery for rectal cancer after preoperative chemo-radiotherapy between the period of January, 2010 and December, 2014 at our institute. Four patients had evidence of systemic metastasis at the time of initial evaluation and seven patients did not come for the follow, and were excluded from the study. Out of them, ninety-one patients with complete information, were enrolled into the study. Based on the total number of lymph nodes retrieved, allocation was done into two groups as described earlier. Among these groups, fifty-three patients (58.2%) had 12 or more lymph nodes retrieved and 38 patients (41.8%) had less than 12 lymph nodes. Gender distribution between both the groups was similar (P=0.8). Patients with fewer lymph nodes (group 2) were older than group 1. Median age was 57 years (range, 32–74) compared with 51 years (range, 29–70), respectively (P=0.005). No significant differences were seen in BMI and ASA grade of the patients between these groups (Table 1).
Full table
Tumor characteristics
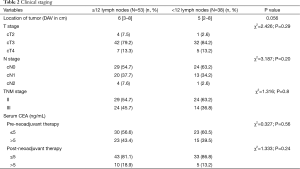
At the time of initial evaluation, the tumor location was more likely to be in the lower rectum in group 1, but the difference was statistically insignificant (P>0.05). Although, preoperative T, N, and TNM stage in relation to lymph node yield was not significantly different (P=0.29, P=0.20 and P=0.80), but patients in group with higher lymph node retrieved had more advance lesions in terms of cT3, node positive and overall TNM stage. Clinical T3 stage was the most commonly seen T stage in both the groups. Approximately, one third of the patients had clinically positive nodes as evident by radiological imaging. The level of serum CEA was found to be more than 5 IU/mL in 58.2% patients in the whole study population with insignificant difference between both the groups (P=0.56) (Table 2).
Full table
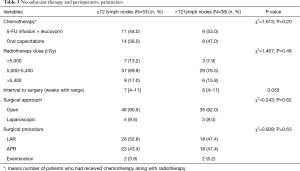
Neoadjuvant treatment
As per institutional protocol, patients with clinical or radiological stage T3, T4 and N positive received neoadjuvant radiotherapy. In addition to that, patients with T4 and node positive also received concurrent chemotherapy either infusion or oral. All ninety-one patients received radiotherapy with dose of 50–54 Gy, only a few patients received boost radiotherapy, the difference between the two groups was not markedly different (P=0.48). Additional concurrent chemotherapy was given to patients with indications to forty-two patients (46.1%) without obvious difference between the two groups (P=0.20) (Table 3).
Full table
Time to surgery
Median time from the completion of the neoadjuvant treatment to surgery was shorter in group 1 than in that with group 2. The median interval was 7 weeks (range, 4–11 weeks) and 8 weeks (range, 4–11), respectively, with no statistically difference (P=0.055) (Table 3).
Type of surgery
Majority of the patients in both groups underwent open surgery, only 10% patients underwent laparoscopic exploration. In both the groups, patients underwent LAR and APR almost equally (P=0.63) (Table 3).
Lymph node retrieval
The number of harvested lymph nodes was significantly different between two groups. Patients in group 2, had a median number of the total lymph nodes 9 (range, 2–11), fewer than the other group, for which the median number of lymph nodes was 16 (range, 12–32) (P<0.001) (Table 4).

Full table
Pathological staging
The pathological characteristics and staging are shown in Table 4. Thirty-eight patients (41.7%) had less than 12 lymph nodes examined in the surgical specimen. There was no significant difference of mean size of the lesion, distance from the anal verge with respect to the total lymph nodes in the surgical specimen. But, patients in the <12 LNs group had smaller tumor size compared to patients in ≥12 LNs (mean size: 3.07±1.59 vs. 3.43±1.97 cm, P=0.35). On pathological evaluation, the proportion of the patients with ypT0 stage was higher in group with fewer lymph nodes 42.1% versus 37.7%, but difference was statistically not significant (P=0.71). Consequently, ypT stage was deviated higher in the group with high lymph node yield as ypT1 was 1.8% vs. 5.2%, ypT2 22.7% vs. 18.4%, ypT3 34% vs. 31.7% and ypT4 was 3.8% vs. 2.6%. The ypN stage was more favourable in the <12 lymph node group (ypN0, 76% vs. 71%; P=0.29). The pCR rate was statistical different between both the groups (39.4% vs. 26.4%, P=0.05). The grade of differentiation of the tumor was more favourable in the patients with fewer lymph nodes, but was statistically insignificant, as well-differentiation was seen in 71.1% patients in group 2 compared to 56.6% in group 1 (P=0.1). The grade of tumor regression was recorded according to Mandard’s criteria, which denoted statistically significant better regression was seen with <12 lymph nodes (TRG 1, 2, 3 was 71.1% vs. 62.3%; P=0.05).
Lymph node status
The median number of total harvested lymph nodes was statistically different between both the groups, as <12 lymph nodes group had 9 lymph nodes (range, 2–11) compared to 16 lymph nodes (range, 12–32) in ≥12 lymph nodes group (P<0.001). The lymph node stage (ypN) was more favourable with <12 lymph node group, 76.4% patients as ypN0 stage versus 71.1% in ≥12 lymph nodes group (P=0.52). Among patients with metastatic lymph nodes, median LNR was lower in <12 lymph nodes group at 0.167 (range, 0.09–0.45) versus 0.187 (range, 0.05–0.54), difference was not statistically significant (P=0.81) (Table 4).
Although differences regarding lymphocytic infiltration, lympho-vascular invasion and peri-neural invasion were not statistically significant, findings were more favourable with fewer lymph node group (Table 4).
Surgical margin status
Positive circumferential radial margins were more common in patients with >12 lymph nodes (9.4% vs. 5.2%, P=0.26). The distal edge of the tumor was located lower in <12 lymph node group (median distance from anal verge 2.2 cm (range,0–5.3) compared to 2.4 cm (range, 0–6.9) in ≥12 lymph nodes group (P=0.56) (Table 4).
Discussion
Total number of lymph node harvested in the surgical specimen has paramount impact on prognosis in colorectal cancer and imitates the adequacy of lymph node surgical clearance: number of metastatic lymph nodes higher with increase the total number of lymph nodes examined. The standard guidelines for the minimum number of lymph nodes to be examined in colorectal specimen is mainly to avoid the probability of under-staging, which is an important prognostic factor (7,19-21). These guidelines have some drawbacks with rectal cancer specifically, and are more suitable for the colonic cancers. This could be explained as following. First, the length of the specimen is variable in rectal cancer compared to colon cancer, which leads to fewer number of total lymph nodes retrieved in rectal cancer (20). Second, lymph nodes in mesocolon are larger in size than those in mesorectum, which may be difficult to identify (22). And third, neoadjuvant treatment has an established role in locally advanced rectal cancer, but not in colon cancers, and thus, has become the standard treatment in rectal cancer (23,24).
The influence of minimum number of lymph nodes in rectal cancer is a matter of discussion for the surgeon and the pathologist both. The survival impact of the number of lymph nodes retrieved in rectal cancer is also a matter of debate, in contrast to colon cancer and non-irradiated rectal cancer.
In modern circumstances, preoperative radiotherapy is broadly established for locally advanced rectal cancers with stage T3–T4 or N-positive, to improve the local control of disease and facilitate margin negative resection and increase the probability of successful sphincter preserving surgery (15,25).
Total number of lymph nodes harvested, varies in each individual patient and depends up-on several factors including gender, age, location of tumor and use of preoperative radiotherapy or chemo-radiotherapy (26-28). In our study, the median age was significantly higher in group 2 patients with median age in 57 [32–74] years in comparison to group 1 was 51 [29–70] years (P=0.005). However, Shen et al. reported that the mean number of lymph nodes was lower in younger patients (P=0.002) (27,29). The location of the tumor in relation to the number of lymph nodes retrieved is also controversial as some authors have a notion that distal rectum has tendency to have higher lymph node retrieval and <12 lymph nodes reflects suboptimal radicality of the surgery (29). In contrast, other authors have observed that in the group of fewer lymph nodes tumor located at the lower level with similar results in our study (30,31).
There is obvious clinical importance of the number of lymph nodes in surgical specimen after chemo-radiation, and the association of fewer lymph nodes with poor oncological procedure and outcome should be declined. The disease control in the group of patients with low or nil lymph nodes retrieved is proved better as compared to ypN+, and is not inferior to ypN0 (32).
The reason behind this, lower lymph nodes retrieval might be radiation induced lymphocytes depletion and development of stromal fibrous tissue leading to decrease in the size of these lymph nodes, and thus less likely to have malignant cells (33). Down-staging in locally advanced rectal cancer after chemo-radiation has been universally accepted with respect to T as well as N stage (23). The normal mesorectal fibro-fatty tissue also atrophies due to radiation induced fibrosis. These factors confound to make it difficult to recognize lymph nodes in irradiated specimen by gross examination (17,32,34,35). In addition, the lymphoid tissue is highly sensitive to radiation and shows more rapid apoptosis, leading to more favourable response than rectal wall thickness (36-39).
Preoperative TNM staging is not a significant factor to affect the number of lymph node retrieval. The degree of decline in serum CEA level after chemo-radiation in patients with raised CEA, correlated with the grade of regression which was proved by the high conversion rate in group 2 (67% vs. 56%, P=0.24).
Only a few patients received concurrent chemotherapy in both the groups, almost in equal numbers. However, it is a limitation in our study that the additional chemotherapy was not given to all patients. The dose of the radiation was not uniformly used in study group, varied from 45 to 54 Gy. The drawback is overlooked with the non-significant difference between both groups.
Although, the standardized treatment including preoperative chemo-radiation followed by TME and complete pathological evaluation is unanimously followed worldwide, but the number of lymph nodes harvested varies greatly with ranging 29% to 72% (17,29-31,39,40).
To consider, a rectal cancer non-metastatic to regional lymph nodes, the World Congress of Gastroenterology, Sydney, formulated the guidelines that require a minimum of 12 lymph node to be examined because of the prognostic value (41). Preoperative irradiation has been recognized as a factor to decrease the number of lymph nodes in the specimen and questioned the diligence of surgeon while operating and pathologist during specimen assessment. Subsequently, several studies recommended to revise the guidelines about minimum number of lymph nodes to be reduced in irradiated patients for adequate staging (42,43).
Longer time interval between completion of neoadjuvant treatment and surgery is associated with a lower lymph node yield because of development of more stromal fibrosis. In our study, this factor was negligible because the difference of time interval from CRT to surgery was statistical insignificant (7 weeks, range: 4–11 vs. 8 weeks, range: 4–11; P>0.05).
Type of surgery, i.e., anterior resection or abdominal perineal resection was performed according to the status of lower edge of the tumor with respect to anal verge. Successively, proximal tumors underwent, in majority of cases, anterior resection or low anterior resection, and were associated with higher lymph node retrieval. In our study, both the groups were comparable regarding type of surgery performed (P=0.63) (Table 3).
Smaller tumor size had high association with <12 lymph nodes but statistically not proved to be a significant factor affecting lymph node harvest (mean size of lesion 3.07±1.59 vs. 3.43±1.97; P=0.35). However, smaller residual lesion size is an indirect indicator of the tumor response to neoadjuvant CRT, that supports our hypothesis that fewer lymph nodes correlate with treatment response (30,31).
Pathological TNM staging (ypTNM) showed that the patients in <12 lymph nodes group had significantly higher rate of complete response of the primary lesion (39.4% vs. 26.4%; P<0.05). This is an important prognostic factor in locally advanced rectal cancer after neoadjuvant CRT. We noticed a significant difference of the pCR in our study compared to previous studies. This could be due to some of the poor response patients not undergoing surgical intervention after neo-adjuvant treatment. Thus, complete pathological response in this group strongly suggests that low lymph node yield after neoadjuvant treatment in rectal cancer indicates the treatment response rather than an insufficient oncological resection or inappropriate pathological assessment (30,39,41).
Well differentiated tumors were more prevalent in patients with <12 lymph nodes. Poorly differentiated tumor usually showed low response and resulted in more residual tumor and lymph node retrieval.
Tumor regression was graded according to Mandard’s grading score, which found statistically significant higher grade 1–3 response in group of <12 lymph nodes (71.1% vs. 62.3%; P=0.05). Median number of the lymph nodes were significantly different between both the groups with 9 lymph nodes (range, 2–11) compared to 16 lymph nodes (range, 12–32) in group 2 and group 1, respectively. This wide variability of lymph nodes retrieval despite a high level constant standard practice of preoperative CRT, surgical and pathological techniques followed, which is proves the difference in biological response of the tumor to neoadjuvant treatment between the two groups. In this study, the level of difference in TRG between both groups strongly concludes our hypothesis.
However, the absolute minimum number of 12 lymph nodes to be examined, as proposed by AJCC and IUAC reports in colo-rectal cancers, is copiously reinforced worldwide. In contrast, this report strongly declines such approach in rectal cancer patients who have received neoadjuvant treatment. In addition to the total number of lymph nodes examined, the absolute number of metastatic lymph nodes and LNR of metastatic to total number of lymph nodes examined have been recognized as new prognostic factors for the survival in rectal cancer similar to other malignancies including breast, pancreas and gastric carcinoma (4,11,12,44-46). Moreover, LNR has been identified superior than pN stage in rectal cancer in view of reflecting the response of preoperative therapy as well as regulating the administration of post-operative adjuvant treatment (47-49).
This study also has a few limitations commonly seen in retrospective studies, such as lack of data of all patients, lack of absolute standardization of pre-operative treatment planning and pathological analysis, the pathologist might not be keen in a comprehensive search of lymph nodes in a specimen with evidence of complete response in the primary lesion. Relative small sample size was also a limitation. Introduction of chemotherapy in our study was not uniformly done. This report calls into question the current recommendation regarding minimum target of lymph node retrieval for the locally advanced rectal cancer treated with neo-adjuvant treatment and stresses to institute in future a large prospective study to endorse a similar correlation of TRG as well as cancer outcome with the number of lymph nodes examined.
Furthermore, we are concentrating on regular follow up of these patients to evaluate the correlation between lymph node yield and local recurrence, distant recurrence and survival and planning to document in the literature shortly.
Conclusions
Even with a few drawbacks in our study, the retrieval of fewer than 12 lymph nodes in surgical specimen of rectal cancer who had received neo-adjuvant radiotherapy with or without chemotherapy should be considered as a good indicator of tumor response with better local disease control, and a good prognostic factor, rather than as a pointer of poor diligence of the surgical oncologist and onco-pathologists.
Acknowledgements
We acknowledged to Department of Medical Records and Department of Epidemiology and statistics of our institute.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: Our study was proposed to Institutional Scientific Review Board on dated 26 March, 2016 and approved for the publication with No. KMIO/MEC/008-A/26/03/2016.
References
- Berger AC, Sigurdson ER, LeVoyer T, et al. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol 2005;23:8706-12. [Crossref] [PubMed]
- Lee HY, Choi HJ, Park KJ, et al. Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol 2007;14:1712-7. [Crossref] [PubMed]
- Johnson PM, Porter GA, Ricciardi R, et al. Increasing negative lymph node count is independently associated with improved long-term survival in stage IIIB and IIIC colon cancer. J Clin Oncol 2006;24:3570-5. [Crossref] [PubMed]
- Chang GJ, Rodriguez-Bigas MA, Skibber JM, et al. Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 2007;99:433-41. [Crossref] [PubMed]
- Baxter NN, Virnig DJ, Rothenberger DA, et al. Lymph node evaluation in colorectal cancer patient: a population-based study. J Natl Cancer Inst 2005;97:219-25. [Crossref] [PubMed]
- Caplin S, Cerottini JP, Bosman FT, et al. For patients with Dukes’ B (TNM stage II) colorectal carcinoma, examination of six or fewer lymph nodes is related to poor prognosis. Cancer 1998;83:666-72. [Crossref] [PubMed]
- Greene FL, Page DL, Fleming ID, et al. editors. AJCC Cancer Staging Manual. American Joint Committee. 7th ed. New York, NY: Springer, 2010.
- Sobin LH, Wittekind Ch. editors. TNM Classification of Malignant Tumors. 5th ed. New York, NY: Wiley, 1997:64-7.
- Nelson H, Petrelli N, Carlin A, et al. Guidelines 2000 for Colon and Rectal Cancer Surgery. J Natl Cancer Inst 2001;93:583-96. [Crossref] [PubMed]
- National Quality Forum Endorsed Commission on Cancer Measures for Quality of Cancer Care for Breast and Colorectal Cancers. ACS Press Release, May 14, 2007. Available online: www.facs.org/cancer/qualitymeasures.html. First Accessed March 9, 2008.
- Chang GJ, Rodriguez-Bigas MA, Eng C, et al. Lymph node status after neoadjuvant radiotherapy for rectal cancer is a biologic predictor of outcome. Cancer 2009;115:5432-40. [Crossref] [PubMed]
- Kim H, Chie EK, Ahn YC, et al. Impact on Loco-regional Control of Radio-chemotherapeutic Sequence and Time to Initiation of Adjuvant Treatment in Stage II/III Rectal Cancer Patients Treated with Postoperative Concurrent Radio-chemotherapy. Cancer Res Treat 2014;46:148-57. [Crossref] [PubMed]
- Kim TH, Chang HJ, Kim DY, et al. Pathologic nodal classification is the most discriminating prognostic factor for disease-free survival in rectal cancer patients treated with preoperative chemo-radiotherapy and curative resection. Int J Radiat Oncol Biol Phys 2010;77:1158-65. [Crossref] [PubMed]
- Wichmann MW, Muller C, Meyer G, et al. Effect of preoperative radio-chemotherapy on lymph node retrieval after resection of rectal cancer. Arch Surg 2002;137:206-10. [Crossref] [PubMed]
- Kapiteijn E, Marijnen C, Nagtegaal I, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 2001;345:638-46. [Crossref] [PubMed]
- Baxter NN, Morris AM, Rothenberger DA, et al. Impact of preoperative radiation for rectal cancer on subsequent lymph node evaluation: a population-based analysis. Int J Radiat Oncol Biol Phys 2005;61:426-31. [Crossref] [PubMed]
- Marks JH, Valsdottir EB, Rather AA, et al. Fewer than 12 lymph nodes can be expected in a surgical specimen after high-dose chemoradiation therapy for rectal cancer. Dis Colon Rectum 2010;53:1023-9. [Crossref] [PubMed]
- Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma. Clinicopathologic correlations. Cancer 1994;73:2680-6. [Crossref] [PubMed]
- Baxter NN. Is lymph node count an ideal quality indicator for cancer care? J Surg Oncol 2009;99:265-8. [Crossref] [PubMed]
- Wong JH, Severino R, Honnebier MB, et al. Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncol 1999;17:2896-900. [PubMed]
- McDonald JR, Renehan AG, O’Dwyer ST, et al. Lymph node harvest in colon and rectal cancer: current considerations. World J Gastrointest Surg 2012;4:9-19. [Crossref] [PubMed]
- Dworák O. Number and size of lymph nodes and node metastases in rectal carcinomas. Surg Endosc 1989;3:96-9. [Crossref] [PubMed]
- Francois Y, Nemoz CJ, Baulieux J, et al. Influence of the interval between preoperative radiation therapy and surgery on down-staging and on the rate of sphincter-sparing surgery for rectal cancer: The Lyon R90-01 randomized trial. J Clin Oncol 1999;17:2396-402. [PubMed]
- Legoux JL, Lehur PA, Penna C, et al. Rectal cancer. Gastroenterol Clin Biol 2006;30:2S43-2S51.
- Rullier E, Goffre B, Bonnel C, et al. Preoperative radio-chemotherapy and sphincter-saving resection for T3 carcinomas of the lower third of the rectum. Ann Surg 2001;234:633-40. [Crossref] [PubMed]
- Sarli L, Bader G, Iusco D, et al. Number of lymph nodes examined and prognosis of TNM stage II colorectal cancer. Eur J Cancer 2005;41:272-9. [Crossref] [PubMed]
- Shen SS, Haupt BX, Ro JY, et al. Number of lymph nodes examined and associated clinic-pathologic factors in colorectal carcinoma. Arch Pathol Lab Med 2009;133:781-6. [PubMed]
- Govindarajan A, Gonen M, Weiser MR, et al. Challenging the feasibility and clinical significance of current guidelines on lymph node examination in rectal cancer in the era of neoadjuvant therapy. J Clin Oncol 2011;29:4568-73. [Crossref] [PubMed]
- Rullier A, Laurent C, Capdepont M, et al. Lymph nodes after preoperative chemoradiotherapy for rectal carcinoma: Number, status, and impact on survival. Am J Surg Pathol 2008;32:45-50. [Crossref] [PubMed]
- Persiani R, Biondi A, Gambacorta MA, et al. Prognostic implications of the lymph node count after neoadjuvant treatment for rectal cancer. Br J Surg 2014;101:133-42. [Crossref] [PubMed]
- de Campos-Lobato LF, Stocchi L, de Sousa JB, et al. Less than 12 nodes in the surgical specimen after total mesorectal excision following neoadjuvant chemoradiation: It means more than you think! Ann Surg Oncol 2013;20:3398-406. [Crossref] [PubMed]
- Habr-Gama A, Perez RO, Proscurshim I, et al. Absence of lymph nodes in the resected specimen after radical surgery for distal rectal cancer and neoadjuvant chemoradiation therapy: what does it mean? Dis Colon Rectum 2008;51:277-83. [Crossref] [PubMed]
- Beresford M, Glynne-Jones R, Rickman P, et al. The reliability of lymph-node staging in rectal cancer after preoperative chemo-radiotherapy. Clin Oncol (R Coll Radiol) 2005;17:448-55. [Crossref] [PubMed]
- Lee WS, Lee SH, Baek JH, et al. What does absence of lymph node in resected specimen mean after neoadjuvant chemoradiation for rectal cancer. Radiat Oncol 2013;8:202. [Crossref] [PubMed]
- Ha YH, Jeong SY, Lim SB, et al. Influence of preoperative chemo-radiotherapy on the number of lymph nodes retrieved in rectal cancer. Ann Surg 2010;252:336-40. [Crossref] [PubMed]
- Marijnen CA, Nagtegaal ID, Klein Kranenbarg E, et al. For Pathology Review Committee and the Cooperative Clinical Investigators. No down-staging after short-term preoperative radiotherapy in rectal cancer patients. J Clin Oncol 2001;19:1976-84. [PubMed]
- Chou JF, Row D, Gonen M, et al. Clinical and pathologic factors that predict lymph node yield from surgical specimens in colorectal cancer: a population-based study. Cancer 2010;116:2560-70. [Crossref] [PubMed]
- Doll D, Gertler R, Maak M, et al. Reduced lymph node yield in rectal carcinoma specimen after neoadjuvant radiochemotherapy has no prognostic relevance. World J Surg 2009;33:340-7. [Crossref] [PubMed]
- Koo T, Song C, Kim JS, et al. Impact of Lymph Node Ratio on Oncologic Outcomes in ypStage III Rectal Cancer Patients Treated with Neoadjuvant Chemoradiotherapy followed by Total Mesorectal Excision, and Postoperative Adjuvant Chemotherapy. PLoS One 2015;10:e0138728. [Crossref] [PubMed]
- Kim WR, Han YD, Cho MS, et al. Oncologic Impact of Fewer Than 12 Lymph Nodes in Patients Who Underwent Neoadjuvant Chemoradiation Followed by Total Mesorectal Excision for Locally Advanced Rectal Cancer. Medicine (Baltimore) 2015;94:e1133. [Crossref] [PubMed]
- Fielding LP, Arsenault PA, Chapuis PH, et al. Clinicopathological staging for colorectal cancer: An International Documentation System (IDS) and an International Comprehensive Anatomical Terminology (ICAT). J Gastroenterol Hepatol 1991;6:325-44. [Crossref] [PubMed]
- Maurel J, Launoy G, Grosclaude P, et al. Lymph node harvest reporting in patient with carcinoma of the large bowel. Cancer 1998;82:1482-6. [Crossref] [PubMed]
- Cianchi F, Palomba A, Boddi V, et al. Lymph node recovery from colorectal tumor specimens: recommendations for a minimum number of lymph nodes to be examined. World J Surg 2002;26:384-9. [Crossref] [PubMed]
- Wu SG, Li Q, Zhou J, et al. Using the Lymph Node Ratio to Evaluate the Prognosis of Stage II/III Breast Cancer Patients Who Received Neoadjuvant Chemotherapy and Mastectomy. Cancer Res Treat 2015;47:757-64. [Crossref] [PubMed]
- Bhatti I, Peacock O, Awan AK, et al. Lymph node ratio versus number of affected lymph nodes as predictors of survival for resected pancreatic adenocarcinoma. World J Surg 2010;34:768-75. [Crossref] [PubMed]
- Sun Z, Zhu GL, Lu C, et al. The impact of N-ratio in minimizing stage migration phenomenon in gastric cancer patients with insufficient number or level of lymph node retrieved: results from a Chinese mono-institutional study in 2159 patients. Ann Oncol 2009;20:897-905. [Crossref] [PubMed]
- Moug SJ, Saldanha JD, McGregor JR, et al. Positive lymph node retrieval ratio optimises patient staging in colorectal cancer. Br J Cancer 2009;100:1530-3. [Crossref] [PubMed]
- Rosenberg R, Engel J, Bruns C, et al. The prognostic value of lymph node ratio in a population-based collective of colorectal cancer patients. Ann Surg 2010;251:1070-8. [Crossref] [PubMed]
- Tong LL, Gao P, Wang ZN, et al. Can lymph node ratio take the place of pN categories in the UICC/AJCC TNM classification system for colorectal cancer? Ann Surg Oncol 2011;18:2453-60. [Crossref] [PubMed]


