A case of esophageal squamous cell intraepithelial neoplasia with positivity for type 16 human papillomavirus successfully treated with radiofrequency ablation
Introduction
Esophageal cancer is the eighth most common cancer worldwide and the sixth cause of cancer related death (1-3). Squamous cell carcinoma (SCC) is the leading pathological type with mean rates of incidence of 2.5-5/100.000 cases among men and 1.5-2.5 cases among women but higher incidence rates are reported in high risk countries such as China, Iran, South Africa and France (4,5).
Principal risk factors for its development are alcohol consumption, smoking, nutritional deficiencies and physical injuries but several studies have evaluated the possible association with infections (6). The role of human papilloma virus (HPV) has been investigated with controversial results. Persistent HPV infection has been detected in benign esophageal squamous cells tumors (4) but there are no studies proving a clear causal association between HPV infection and cancer. Since 1982 at least 70 studies have reported detection rates of HPV in esophageal SCC ranging from 0% to 67% (7) with viral type 16 being the most common (8,9).
Given the lack of evidence regarding the significance of HPV in esophageal SCC, no specific indications or guidelines for possible endoscopic and surgical therapeutic approaches to this clinical scenario are available.
European Organization for Research and Treatment of Cancer (EORTC) treatments strategies for esophageal SCC suggest the use of endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) in early cancers with exclusive mucosal involvement with more aggressive surgical approaches indicated in those cases in which submucosal invasion is present (10).
Radiofrequency ablation (RFA) is an endoscopic technique that is currently used for the treatment of flat high-grade dysplasia in Barrett’s esophagus (11). Recently it has also been evaluated in the setting of esophageal SCC in small prospective studies (12-14).
We report a case of esophageal SCC in situ with histologic and microbiologic findings of genotype 16 HPV infection successfully treated with a single session of RFA.
Case report
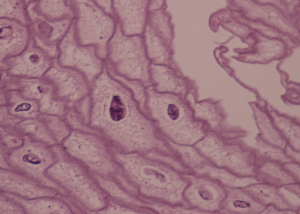
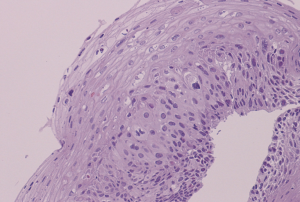
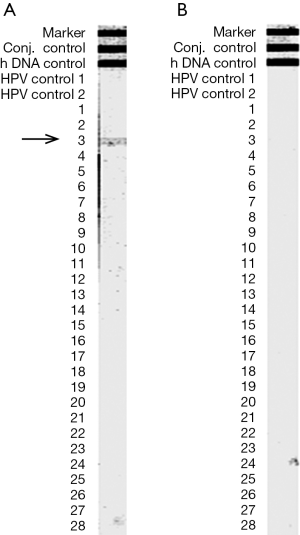
In November 2011, a 62-year-old white woman was referred to our unit because of dyspeptic syndrome. Past history included hypothyroidism treated with L-thyroxine, Irritable Bowel Syndrome and Gastroesophageal Reflux Disease managed with PPIs. Upper gastrointestinal endoscopy (UGIE) revealed the presence of a dyscromic area of about 2 cm in diameter which was located 30 cm from the incisors. Lugol staining confirmed the presence of an unstained area of about 30 mm involving half of the esophageal circumference. Histologic examination showed the presence of cytoarchitectural atypias of squamous epithelium with atypical mitosis, enlarged nuclei with nuclear alterations and parakeratotic hyperkeratosis (Figure 1). Specifically the presence of koilocytosis, giant and multinucleated cells, associated with hyperkeratosis, acanthosis, and koilocytic-like modifications suggested the possible association with an HPV infection. In March 2012 a second UGIE with multiple biopsies of the targeted area and the entire length of esophagus was performed. Histologic diagnosis of high grade intraepithelial neoplasia (HGIEN sec. WHO) was confirmed in biopsy samples obtained from the unstained area (Figure 2). Immunohistochemical staining for CMV and HSV were negative as well as histochemical PAS staining for fungal colonization. Assessment with INNO-LiPA assay for HPV revealed positivity for genotype 16 HPV only in the biopsies obtained from the HGIEN area (Figure 3A). The same test for HPV was negative in the remaining biopsies from the rest of esophagus. In April 2012 a session of RFA (RFA; HALO90 System, GI Solutions, Covidien, Sunnyvale, Calif) on the dysplastic esophageal area was performed. There were no complications during or after the procedure. An UGIE with Lugol staining was repeated after two months: a whitish semi-circumferential area suggestive of scarring was detected in the middle esophagus at the site of prior ablation, but no signs of dysplasia were evident. Microbiologic evaluation with INNO-LiPA assay excluded the persistence of HPV infection (Figure 3B). The same result was confirmed in the following UGIEs with biopsies performed in October 2012 and April 2013.
Discussion
HPV is a DNA virus whose association with anogenital and head and neck cancer has been clearly identified (15,16). HPV may be often detected in the squamous epithelium of the esophagus and is considered to be related to the appearance of benign lesions with no risk of progression. Several studies have tried to identify a potential role of HPV in esophageal SCC carcinogenesis but results have been non-conclusive yet (4). The first peculiar finding of our case report is that the presence of HPV was suspected on the basis of the histologic similarities between tissue from the neoplastic esophageal lesion and tissues from typical HPV related cervical neoplasms. Interestingly, HPV infection was then confirmed by microbiologic assays exclusively in the areas with neoplastic changes but not in the surrounding healthy esophageal epithelium. Moreover the most virulent HPV genotype was identified, which may have been associated with neoplastic progression of this HPV-related esophageal lesion. The second point of interest in this case is the efficacy of a single course of RFA on neoplastic change and HPV infection as well. Biopsy specimens from three subsequent endoscopic exams have demonstrated a complete histological response with absence of residual dysplasia and eradication of HPV colonization. Some small prospective studies have already suggested the potential role of RFA in patients with early squamous cell neoplasia of the esophagus but this therapeutic approach has never been evaluated in the setting of controlled trials (12-14). Our experience supports this possible new use of the HALO90 RFA procedure in patients with superficial early squamous cell neoplasia, suggesting the treatment can be effective with potential lower complications rates than more invasive techniques such as EMR, ESD and esophagectomy. Moreover, since the etiologic role of HPV in esophageal carcinogenesis is uncertain, our case may facilitate discussion regarding the appropriateness of regular endoscopic follow-up in patients with HPV esophageal colonization and of eventual prophylactic treatment of benign HPV-related lesions. Further investigations are warranted.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol 2006;24:2137-50. [PubMed]
- Jemal A, Bray F, Center MM, et al. Global cancer statistics. CA Cancer J Clin 2011;61:69-90. [PubMed]
- Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer 2010;127:2893-917. [PubMed]
- Syrjänen KJ. HPV infections and oesophageal cancer. J Clin Pathol 2002;55:721-8. [PubMed]
- Pennathur A, Gibson MK, Jobe BA, et al. Oesophageal carcinoma. Lancet 2013;381:400-12. [PubMed]
- Lambert R, Hainaut P.Esophageal cancer: cases and causes (part I). Endoscopy 2007;39:550-5. [PubMed]
- Dąbrowski A, Kwaśniewski W, Skoczylas T, et al. Incidence of human papilloma virus in esophageal squamous cell carcinoma in patients from the Lublin region. World J Gastroenterol 2012;18:5739-44. [PubMed]
- Dillner J, Knekt P, Schiller JT, et al. Prospective seroepidemiological evidence that human papillomavirus type 16 infection is a risk factor for oesophageal squamous cell carcinoma. BMJ 1995;311:1346. [PubMed]
- Han C, Qiao G, Hubbert NL, et al. Serologic association between human papillomavirus type 16 infection and esophageal cancer in Shaanxi Province, China. J Natl Cancer Inst 1996;88:1467-71. [PubMed]
- Lutz MP, Zalcberg JR, Ducreux M, et al. Highlights of the EORTC St. Gallen International Expert Consensus on the primary therapy of gastric, gastroesophageal and oesophageal cancer - differential treatment strategies for subtypes of early gastroesophageal cancer. Eur J Cancer 2012;48:2941-53. [PubMed]
- Bennett C, Vakil N, Bergman J, et al. Consensus statements for management of Barrett’s dysplasia and early-stage esophageal adenocarcinoma, based on a Delphi process. Gastroenterology 2012;143:336-46. [PubMed]
- Bergman JJ, Zhang YM, He S, et al. Outcomes from a prospective trial of endoscopic radiofrequency ablation of early squamous cell neoplasia of the esophagus. Gastrointest Endosc 2011;74:1181-90. [PubMed]
- van Vilsteren FG, Alvarez Herrero L, Pouw RE, et al. Radiofrequency ablation for the endoscopic eradication of esophageal squamous high grade intraepithelial neoplasia and mucosal squamous cell carcinoma. Endoscopy 2011;43:282-90. [PubMed]
- Becker V, Bajbouj M, Schmid RM, et al. Multimodal endoscopic therapy for multifocal intraepithelial neoplasia and superficial esophageal squamous cell carcinoma - a case series. Endoscopy 2011;43:360-4. [PubMed]
- Syrjänen S. The role of human papillomavirus infection in head and neck cancers. Ann Oncol 2010;21 Suppl 7:vii243-5. [PubMed]
- Zandberg DP, Bhargava R, Badin S, et al. The role of human papillomavirus in nongenital cancers. CA Cancer J Clin 2013;63:57-81. [PubMed]


