
Anorectal manometry after rectal surgery: a case report with rectal bleeding and perforation
Introduction
Anorectal manometry (ARM) is primarily used to assess anorectal sensorimotor function (1). ARM provides comprehensive information about the anal sphincter and rectal sensation (2) in patients with constipation (3) or fecal incontinence. Generally, ARM can be applied to both adults and children (4). ARM rarely induces colorectal perforation in patients after rectal cancer surgery; however, it still has the possibility to induce death (3,5,6). Assessment of anorectal function after combined laparoscopic transanal total mesorectal resection is an indication for AMR (7). Organic lesions are a relative contraindication to ARM (8). To date, there have been no reports of cases in which ARM simultaneously induced colonic bleeding and perforation in patients with no history of rectal cancer surgery either at home or abroad.
In this article, we report the case of a patient who suffered from ARM-induced rectal bleeding and perforation, and was treated by timely and aggressive surgery. After treatment, the patient did not experience any complications. This is the first reported case of a patient with no history of rectal cancer surgery suffering from ARM-induced rectal bleeding and perforation. The objective of our report is to provide a reference for the treatment of patients who undergo ARM after rectal surgery. We present the following article in accordance with the CARE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-784/rc).
Case presentation
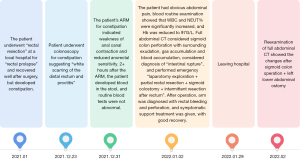
A 58-year-old female patient was admitted to our hospital due to hematochezia after the completion of ARM for 2+ hours. The patient had received ARM to treat constipation, and after 2+ hours, bloody stool, accompanied by blood clots, was observed, but the patient did not report any discomfort, such as abdominal pain, abdominal distension, chills, or a fever. The patient was ultimately admitted to the Anorectal Department for treatment.
During treatment, the patient continued to fast and was in normal spirits, her sleep was slightly poor, but her urine volume was normal, and she showed no significant weight loss or gain. The patient had a history of hypertension and cerebral infarction for >2 years,11+ months ago, the patient visited “Zheng’an County People's Hospital” for a swelling that prolapsed from the anus during defecation, diagnosis of “rectal prolapse” and “laparoscopic combined transanal rectal resection”. The patient recovered well after surgery and was discharged after 10+ days of treatment, but developed constipation. Usually, using glycerol enemas to treat constipation, there is no discomfort such as anal cessation of defecation and fecal incontinence. However, the constipation did not improve, and the patient was referred to our hospital.
The patient’s physical examination results at admission were as follows: (I) stable vital signs; (II) height: 150 cm; weight, 60+ kg; (III) distended abdomen, without gastrointestinal type or peristaltic waves, without tenderness, rebound tenderness, or muscular tension, liver and spleen not palpable, negative shifting dullness, and normal bowel sounds; (IV) in the genucubital position, hemorrhoids were observed at the anal verge, but the inner rectal wall was smooth, no mass or rupture was palpable, and the finger covers could be observed the blood when withdrawal from the anus. As for the auxiliary examination, the results of a colonoscopy 1 week before this admission revealed white scars and proctitis in the distal rectum, and the water-perfused catheters for the ARM 2+ hours ago showed decreased anorectal sensitivity and poor anal canal contraction.
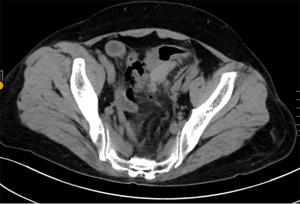
After admission, the examinations revealed no abnormalities in the routine blood, routine urine, blood biochemistry, and coagulation function results, and the patient was required to fast and given symptomatic and supportive treatment. On the 2nd day of admission, routine blood examinations revealed that the patient’s hemoglobin (Hb) was 104 g/L and hematocrit (HCT) was 33.40%. On the 3rd day after admission, the patient had no relief from her hematochezia and suffered abdominal pain, and the routine blood examination revealed a white blood cell (WBC) of 16.70×109/L, a neutrophil percentage (NEUT%) of 89.70%, a red blood cell (RBC) count of 3.65×1012/L, Hb of 97 g/L, and HCT of 31.80%. Computed tomography (CT) of the whole abdomen was performed, and sigmoid colon perforation with surrounding exudation, pneumatosis, hematocele, and abdominal aortic sclerosis were observed (Figure 1).
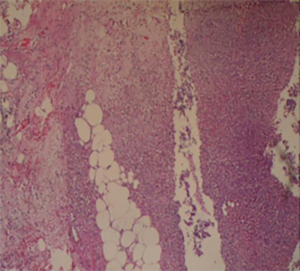
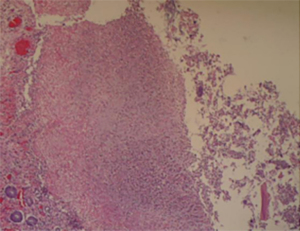
After excluding surgical contraindications, the patient received an emergency exploratory laparotomy, partial rectal resection, sigmoidostomy, and intermittent retrorectal resection. The postoperative specimens are shown in Figure 2, and the pathological biopsies are shown in Figures 3,4. After surgery, the patient’s vital signs were monitored, fasting was required, symptomatic and supportive treatment was administered, her routine blood, blood biochemistry, sepsis, high-sensitivity C-reactive protein, and thyroid function results were monitored, and whole abdominal CT, and other relevant examinations were conducted. After the above treatment, the patient experienced some discomfort, such as occasional anal itching and anal pendant expansion, but her exhaust and defecation were normal, and blood supply was good at the intestinal end of the abdominal stoma. After ARM, the patient suffered from rectal bleeding and perforation. A whole abdominal CT reexamination 1 month after surgery showed postoperative changes in the patient after the sigmoidostomy and left lower quadrant colostomy. The whole diagnosis, treatment and prognosis of this case as shown in Figure 5.
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
ARM provides comprehensive information about the anal sphincter and rectal sensation in patients with constipation (2) or fecal incontinence (3). Generally, the main parameters of ARM include the resting anal pressure, the anal canal maximum squeeze pressure, the spontaneous continuous squeeze time of the anal canal, the length of the anal sphincter, the initial sensory threshold, the initial defecation sensory threshold, the defecation distress threshold, the maximum volume sensory threshold, paradoxical contraction, and the anorectal inhibitory reflex. Despite the few cases of ARM-induced colorectal perforation after rectal cancer surgery, it still has the possibility to induce death (5). To date, individuals without a history of rectal cancer surgery have not been reported to suffer simultaneously from ARM-induced colonic bleeding and perforation either at home or abroad. The patient in this case denied any history of rectal cancer, but she still displayed rectal bleeding and perforation after ARM. We suspected that the bleeding and perforation were induced by the routine maximum tolerated volume. First, the patient had a history of rectal prolapse surgery and the colonoscopy examination results indicated white scars and proctitis at the distal rectum. Second, administering a glycerol enema to the patient may have aggravated the proctitis. Finally, the patient had a medical history of hypertension and cerebral infarction, and the abdominal CT also suggested abdominal aortic sclerosis and a high possibility of vascular sclerosis in the rectal wall. The above factors led to an abnormal rectal sensation, altered the local anatomy of the rectum, and decreased the compliance of the rectal bowel wall in the patient. Thus, after rectal resection, patients, especially those with hypertension and proctitis, should carefully undergo ARM and the maximum tolerated volume should not be routinely measured.
In the treatment of iatrogenic colonoscopic perforations, endoscopic therapy may be useful for colonic perforations with a diameter of 20 mm in the well-cleansed intestinal tract (9). In fact, conservative treatment may be the appropriate choice for hemodynamically stable patients without peritonitis and with only small perforations. For patients with severe sepsis, large perforations, diffuse peritonitis, and in whom conservative treatment has failed, surgical treatment is preferred (10). ARM-induced colorectal perforation has the same treatment principles as colonoscopy-induced colonic perforation. Due to the poor bowel cleaning of the patient in this study, endoscopic treatment was not considered. Conservative treatment may be considered if the patient suffers from perforation in the mesenteric space, has little spillage of bowel contents, and does not have any symptoms of peritonitis. However, in this case, the elderly female patient had a history of hypertension, cerebral infarction, and rectal surgery. Additionally, in the course of the disease, the patient had symptoms of hematochezia and abdominal pain. Additionally, routine blood tests showed that the WBC count and NEUT% were increased, and Hb and HCT were decreased. Combined with the results of the whole abdominal CT, it was concluded that it was unlikely that the rectal bleeding and perforation would heal spontaneously. Further, it has been reported that adverse factors, such as advanced age, comorbidities, and excessive bleeding, may increase the risk of peritonitis and sepsis, prolong patient hospitalization, and increase mortality (11). Thus, we first performed active surgery and successfully treated this patient who was suffering from ARM-induced rectal bleeding and perforation after rectal surgery without any complications.
ARM is an invasive test, a detailed medical history (especially surgical history) and a thorough physical examination prior to the operation are necessary for us to assess the risk of ARM. Do not routinely measure the maximum tolerated volume (300 mL), and in patients with concomitant proctitis, it is not even recommended to inflate the balloon more than 200 ml; the gas in the balloon should be withdrawn immediately upon completion of the operation to reduce the compression of the balloon on the intestinal wall, and the patient's reaction needs to be closely observed during the operation. Based on our experience, caution must be exercised during balloon inflations for patients who require ARM after rectal surgery, particularly those with comorbidities. Notably, a prompt and aggressive surgical intervention is needed when bleeding and perforation occur in the anorectal canal of the patients.
Conclusions
At present, there is little literature on ARM teaching courses (12). To improve the operation level of ARM and reduce the incidence of complications, we should extend understandings of ARM, develop a systematic management plan, and continuously summarize ARM-related experiences.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-784/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-22-784/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bharucha AE, Basilisco G, Malcolm A, et al. Review of the indications, methods, and clinical utility of anorectal manometry and the rectal balloon expulsion test. Neurogastroenterol Motil 2022;34:e14335. [Crossref] [PubMed]
- Milosavljevic T, Popovic DD, Mijac DD, et al. Chronic Constipation: Gastroenterohepatologist's Approach. Dig Dis 2022;40:175-80. [Crossref] [PubMed]
- Lee KH, Kim JY, Sul YH. Colorectal Perforation After Anorectal Manometry for Low Anterior Resection Syndrome. Ann Coloproctol 2017;33:146-9. [Crossref] [PubMed]
- Poojari VS, Mirani S, Shetty NS, et al. Evaluation of constipation in children using high-resolution anorectal manometry. Trop Doct 2021;51:527-31. [Crossref] [PubMed]
- Park JS, Kang SB, Kim DW, et al. Iatrogenic colorectal perforation induced by anorectal manometry: report of two cases after restorative proctectomy for distal rectal cancer. World J Gastroenterol 2007;13:6112-4. [Crossref] [PubMed]
- Cho YB, Lee WY, Yun HR, et al. Colonic perforation caused by anorectal manometry. Int J Colorectal Dis 2008;23:219-20. [Crossref] [PubMed]
- López-Sánchez A, Morandeira-Rivas A, Moreno-Sanz C, et al. Long-Term Anorectal Manometry Outcomes After Laparoscopic and Transanal Total Mesorectal Excision. J Laparoendosc Adv Surg Tech A 2021;31:395-401. [Crossref] [PubMed]
- Scott SM, Carrington EV. The London Classification: Improving Characterization and Classification of Anorectal Function with Anorectal Manometry. Curr Gastroenterol Rep 2020;22:55. [Crossref] [PubMed]
- Ryu JY, Park BK, Kim WS, et al. Endoscopic closure of iatrogenic colon perforation using dual-channel endoscope with an endoloop and clips: methods and feasibility data (with videos). Surg Endosc 2019;33:1342-8. [Crossref] [PubMed]
- de'Angelis N, Di Saverio S, Chiara O, et al. 2017 WSES guidelines for the management of iatrogenic colonoscopy perforation. World J Emerg Surg 2018;13:5. [Crossref] [PubMed]
- Ospina-Pérez CG, Álvarez-Acuña AM, López-Álvarez LM, et al. Broken beer bottle as a cause of sigmoid perforation: A summary of causes and predictors in the management of traumatic and non-traumatic colorectal perforation. Int J Surg Case Rep 2021;85:106261. [Crossref] [PubMed]
- Cohen DL, Richter V, Malikov I, et al. The Effect of a Didactic Course on Gastroenterology Nurses' Knowledge and Interest in Anorectal Manometry. Gastroenterol Nurs 2021;44:412-7. [Crossref] [PubMed]
(English Language Editor: L. Huleatt)



