
Combination of neutrophil-to-lymphocyte ratio and serum CA 19-9 as a prognostic factor in pancreatic cancer
Highlight box
Key findings
• In patients with pancreatic ductal adenocarcinoma high-neutrophil-to-lymphocyte ratio (NLR) and high-carbohydrate antigen 19-9 (CA 19-9) levels at diagnosis are both independent prognostic factors for worse disease-free survival and overall survival. The combination of these two biomarkers (NLR and CA 19-9) seems to be better for predicting prognosis and stratifying patients.
What is known and what is new?
• Some biomarkers of systemic inflammation have been studied as possible prognostic factors in tumors.
• The classification we propose using NLR and serum CA 19-9 levels could be a better prognostic tool to guide and optimize treatment and follow-up strategies than used separately.
What is the implication, and what should change now?
• Identifying appropriate biomarkers to predict recurrence and survival is essential to improve the determination of prognosis and selection of the best treatment strategy in patients with pancreatic cancer.
• Both biomarkers (NLR and CA 19-9) are accessible, inexpensive, and easily measured, which may facilitate and expand their use.
Introduction
Background
Pancreatic cancer incidence is increasing and projected to be the second leading cause of cancer death by 2030 in the U.S. (1). Despite advances in recent years in the oncological management of pancreatic cancer, it remains one of the most lethal neoplasms with a 5-year survival rate from 5% to 15% and an overall survival (OS) rate of 6% (2), mainly due to early recurrence or progression of the disease despite optimal treatment; even in patients undergoing surgical resection the 5-year survival rate is around 20% (3). In general, pancreatic cancer is considered a systemic disease even if diagnosed in early stages, which occurs in only 10–15% of cases, and most cases are diagnosed with unresectable or metastatic disease. Because of poor outcomes in pancreatic cancer patients, biomarkers are necessary to better predict prognosis and improve treatment strategies.
Rationale and knowledge gap
Carbohydrate antigen 19-9 (CA 19-9) is a cell surface glycoprotein complex, produced by the ductal cells of the pancreas and other organs. It is overexpressed in a wide range of benign diseases such as cholestasis and malignant diseases, mainly in pancreatic ductal adenocarcinoma (PDAC) (4,5). It has been used as a useful biomarker in diagnosis, assessment of resectability, monitoring response to treatment, prognosis, and surveillance in pancreatic cancer (6-9). It reflects biological aggressiveness and is a predictor of hematogenous dissemination, micrometastatic, and metastatic disease since this biomarker plays a role in malignant cell-adhesion to endothelial cells and transmigration (10,11). CA 19-9 values are a valuable prognostic marker in patients undergoing curative resection or neoadjuvant chemotherapy. Previous studies have reported the association between CA 19-9 level and survival in pancreatic cancer. Therefore, postoperative follow-up is important since an increase in serum levels of CA 19-9 may predict recurrence of pancreatic cancer (12-14).
Neutrophil-to-lymphocyte ratio (NLR) is one of the most studied indicators of systemic inflammatory response. Neutrophils are known to infiltrate tumors, contributing to the tumor microenvironment for secretion of cytokines, while lymphocytes induce cell death. NLR has been increasingly validated as a fundamental prognostic factor in different stages of the disease, suggesting that high levels of NLR may reflect unresectable disease or progression depending on the case (15,16). NLR has shown to have a prognostic impact in some malignancies (17-22) including pancreatic cancer (23,24), while other studies have not demonstrated NLR to have a prognostic value in pancreatic cancer patients (25-27).
Previous studies and meta-analysis have shown high NLR to be a predictor of poor outcomes in pancreas cancer patients although a definitive cut-off value has not been established (28,29). Therefore, identifying appropriate biomarkers to predict recurrence and survival is essential to improve the determination of prognosis and selection of the best treatment strategy in patients with pancreatic cancer.
Objective
The aim of this study was to evaluate the role of pretreatment NLR and serum CA 19-9 values alone, and the combination of both values as prognostic factors in patients with PDAC of all stages. We present this article in accordance with the STROBE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-893/rc).
Methods
We conducted a retrospective cohort study in patients with pancreatic cancer at Instituto Nacional de Cancerología. We explored the prognosis impact of NLR, serum CA 19-9, and the combination of both values, with primary endpoints being OS and progression-free survival (PFS). The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This study was approved by the Research and Ethics Committee of Instituto Nacional de Cancerología (No. 2023/020). Informed consent from patients was waived due to the retrospective nature of this study.
Patients
From 2013 to 2018, all patients diagnosed with pancreatic cancer at our institution regardless of stage at diagnosis were retrospectively screened for inclusion. We included patients with histologically confirmed PDAC, over 18 years, complete files with serum levels of lymphocytes, neutrophils and CA 19-9. Patients with previous treatment at other institution, with metachronous or synchronous malignancies, and with missing data were excluded. A final cohort of 153 patients was analyzed.
Data collection
Clinical and pathological variables of patients were collected from electronic medical records. Serum lymphocyte and neutrophil levels at diagnosis were collected, as well as serum CA 19-9 levels at diagnosis. The NLR was calculated by dividing the absolute blood neutrophil count by the absolute blood lymphocyte count. All patients were staged according to the 8th edition American Joint Committee on Cancer tumor-node-metastasis (AJCC TNM) staging system. Information regarding patient status and disease progression was collected. Patients were followed up regularly (every 2 weeks while receiving chemotherapy and every 2 months otherwise). Follow-up included clinical examinations, laboratory testing, and imaging [computed tomography (CT) scan, positron emission tomography-CT (PET-CT), magnetic resonance imaging (MRI)], according to international guidelines. OS was defined as the time from the date of diagnosis to the date of death or last follow-up visit. PFS was defined as the time from the diagnosis to the date of documented recurrence or progression of the disease during follow-up.
Statistical analysis
Continuous variables were presented as median with 95% confidence interval (CI), categorical variables were presented as percentage and compared using Chi-squared or Fisher’s exact test. OS and PFS were calculated using the Kaplan-Meier method and compared with log-rank test. Differences were considered statistically significant when P<0.05. Additionally, multivariate Cox regression analysis was performed to identify association between each variable and survivals; hazard ratios (HRs) and their respective 95% CI were calculated. Only statistically significant variables in the univariate analysis were included in the subsequent multivariate analysis.
To determine the optimal cut-off values of NLR and CA 19-9 we used X-tile software (version 3.6.1, Yale University, U.S.). The cut-off with the lowest P value calculated from the Chi-squared test for OS was selected and patients were classified as having either low- or high-NLR and CA 19-9. The optimal cut-off values were first determined for the entire cohort and later it was identified independently within the subgroups. The best cutoff value of NLR was 2.4, and the cutoff value of CA 19-9 was 553 U/mL. The prognostic value of combined NLR and serum CA 19-9 levels at diagnosis was evaluated by the Cox model and presented as an HR. Statistical analysis was conducted using SPSS software (SPSS 27.0, IBM, Chicago, IL, USA).
Results
Determination of cut-off values for NLR and CA 19-9
The optimal cut-off point value in the whole cohort was set at 2.4 for NLR, and 553 U/mL for serum CA 19-9. Patients were classified as having low-NLR or low-CA 19-9 if their levels were equal to or below the cut-off points and high-NLR or high-CA 19-9 if their levels were above the cut-off points.
According to the cut-off values obtained for NLR and CA 19-9 and in order to explore the combined use of these biomarkers as a prognostic factor, the patients were divided into two groups: Group 1 when both values of NLR and CA 19-9 were low (low-NLR/low-CA 19-9), and Group 2 when either one or both values of NLR and CA 19-9 were high (low-NLR/high-CA 19-9, or high-NLR/low-CA 19-9, or high-NLR/high-CA 19-9).
Patient characteristics and clinical outcomes
One hundred and fifty-three patients were included. The median age was 60 years (95% CI: 28–82) and 52.9% were male. The median tumor size was 4.0 cm (95% CI: 1.6–11.0), the median CA 19-9 was 409 U/mL (95% CI: 2.5–280,000) and the median NLR value was 2.67 (95% CI: 0.12–34.0). Clinicopathologic baseline characteristics and comparisons between groups are shown in Table 1. There was a significant difference between the low-NLR (≤2.4) and high-NLR (>2.4) groups in Eastern Cooperative Oncology Group performance status (ECOG PS), node status, and systemic treatment received. Comparing the low-CA 19-9 (≤553 U/mL) and high-CA 19-9 (>553 U/mL) groups there was a significant difference in age, tumor size, and presence of metastases. According to the classification groups created combining both values of NLR and CA 19-9 there was a significant difference between Group 1 (both low-NLR and low-CA 19-9) and Group 2 (either one or both values of NLR and CA 19-9 high) in ECOG PS, vascular invasion, tumor size, presence of metastases, clinical stage, and global treatment received.
Table 1
| Characteristic | Total (n=153) | NLR | CA 19-9, U/mL | Groups | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤2.4 (n=60) | >2.4 (n=93) | P value | ≤553 (n=80) | >553 (n=73) | P value | Group 1 (n=40) | Group 2 (n=113) | P value | ||||
| Age, n (%) | 0.42 | 0.02* | 0.07 | |||||||||
| ≤65 years | 107 (69.9) | 43 (71.7) | 64 (68.8) | 62 (77.5) | 45 (61.6) | 32 (80.0) | 75 (66.4) | |||||
| >65 years | 46 (30.1) | 17 (28.3) | 29 (31.2) | 18 (22.5) | 28 (38.4) | 8 (20.0) | 38 (33.6) | |||||
| Gender, n (%) | 0.28 | 0.51 | 0.31 | |||||||||
| Female | 72 (47.1) | 26 (43.3) | 46 (49.5) | 38 (47.5) | 34 (46.6) | 17 (42.5) | 55 (48.7) | |||||
| Male | 81 (52.9) | 34 (56.7) | 47 (50.5) | 42 (52.5) | 39 (53.4) | 23 (57.5) | 58 (51.3) | |||||
| BMI (kg/m2), n (%) | 0.37 | 0.56 | 0.78 | |||||||||
| <18.5 | 5 (3.3) | 1 (1.7) | 4 (4.3) | 3 (3.8) | 2 (2.7) | 1 (2.5) | 4 (3.5) | |||||
| 18.5–24.9 | 83 (54.2) | 32 (53.3) | 51 (54.8) | 45 (56.2) | 38 (52.1) | 20 (50.0) | 63 (55.8) | |||||
| 25–29.9 | 44 (28.8) | 21 (35.0) | 23 (24.7) | 24 (30.0) | 20 (27.4) | 14 (35.0) | 30 (26.5) | |||||
| ≥30 | 21 (13.7) | 6 (10.0) | 15 (16.1) | 8 (10.0) | 13 (17.8) | 5 (12.5) | 16 (14.2) | |||||
| ECOG-PS, n (%) | 0.01* | 0.48 | 0.047* | |||||||||
| 0–1 | 127 (83.0) | 55 (91.7) | 72 (77.4) | 67 (83.8) | 60 (82.2) | 37 (92.5) | 90 (79.6) | |||||
| ≥2 | 26 (17.0) | 5 (8.3) | 21 (22.6) | 13 (16.2) | 13 (17.8) | 3 (7.5) | 23 (20.4) | |||||
| Tumor location, n (%) | 0.32 | 0.24 | 0.21 | |||||||||
| Head | 134 (87.6) | 54 (90.0) | 80 (86.0) | 72 (90.0) | 62 (84.9) | 37 (92.5) | 97 (85.8) | |||||
| Body-tail | 19 (12.4) | 6 (10.0) | 13 (14.0) | 8 (10.0) | 11 (15.1) | 3 (7.5) | 16 (14.2) | |||||
| Tumor differentiation, n (%) | 0.56 | 0.96 | 0.32 | |||||||||
| Well | 8 (5.2) | 4 (6.6) | 4 (4.3) | 4 (5.0) | 4 (5.5) | 3 (7.5) | 5 (4.4) | |||||
| Moderate | 47 (30.7) | 16 (26.6) | 31 (33.3) | 25 (31.2) | 22 (30.1) | 15 (37.5) | 32 (28.3) | |||||
| Poor | 24 (15.7) | 7 (11.6) | 17 (18.2) | 12 (15.0) | 12 (16.4) | 4 (40.0) | 20 (17.7) | |||||
| Vascular involvement, n (%) | 0.39 | 0.15 | 0.01* | |||||||||
| No | 61 (39.9) | 26 (43.3) | 35 (37.6) | 36 (45) | 25 (34.2) | 21 (52.5) | 40 (35.4) | |||||
| Venous | 37 (24.2) | 16 (26.7) | 21 (22.6) | 22 (27.5) | 15 (20.5) | 12 (30.0) | 25 (22.1) | |||||
| Arterial | 21 (13.7) | 9 (15.0) | 12 (12.9) | 8 (10.0) | 13 (17.8) | 5 (12.5) | 16 (14.2) | |||||
| Both | 34 (22.2) | 9 (15.0) | 25 (26.9) | 14 (17.5) | 20 (27.4) | 2 (5.0) | 32 (28.3) | |||||
| Tumor size, n (%) | 0.17 | 0.04* | 0.009* | |||||||||
| ≤4 cm | 73 (47.7) | 32 (53.3) | 41 (44.1) | 44 (55.0) | 29 (39.7) | 26 (65.0) | 47 (41.6) | |||||
| >4 cm | 80 (52.3) | 28 (46.7) | 52 (55.9) | 36 (45.0) | 44 (60.3) | 14 (35.0) | 66 (58.4) | |||||
| T, n (%) | 0.60 | 0.43 | 0.24 | |||||||||
| T1 | 10 (6.5) | 4 (6.7) | 6 (6.5) | 6 (7.5) | 4 (5.5) | 4 (10.0) | 6 (5.3) | |||||
| T2–T4 | 143 (93.5) | 56 (93.3) | 87 (93.5) | 74 (92.5) | 69 (94.5) | 36 (90.0) | 107 (94.7) | |||||
| N, n (%) | 0.04* | 0.44 | 0.052 | |||||||||
| N0 | 53 (34.6) | 28 (46.7) | 25 (26.8) | 31 (38.8) | 22 (30.1) | 20 (50.0) | 33 (29.2) | |||||
| N+ | 100 (65.4) | 32 (53.3) | 68 (73.2) | 49 (61.2) | 51 (69.9) | 20 (50.0) | 80 (70.8) | |||||
| M, n (%) | 0.19 | 0.03* | 0.046* | |||||||||
| M0 | 84 (54.9) | 36 (60.0) | 48 (51.6) | 50 (62.5) | 34 (46.6) | 27 (67.5) | 57 (50.4) | |||||
| M1 | 69 (45.1) | 24 (40.0) | 45 (48.4) | 30 (37.5) | 39 (53.4) | 13 (32.5) | 56 (49.6) | |||||
| Clinical stage, n (%) | 0.08 | 0.07 | 0.01* | |||||||||
| I–II | 48 (31.4) | 25 (41.7) | 23 (24.7) | 31 (38.8) | 17 (23.3) | 20 (50.0) | 28 (24.8) | |||||
| III | 38 (24.8) | 12 (20.0) | 26 (28.0) | 20 (25.0) | 18 (24.7) | 8 (20.0) | 30 (26.5) | |||||
| IV | 67 (43.8) | 23 (38.3) | 44 (47.3) | 29 (36.2) | 38 (52.1) | 12 (30.0) | 55 (48.7) | |||||
| Global treatment, n (%) | 0.13 | 0.06 | 0.03* | |||||||||
| Surgery followed by ChT | 20 (13.1) | 11 (18.3) | 9 (9.6) | 16 (20.0) | 4 (5.5) | 10 (25.0) | 10 (8.8) | |||||
| Neoadjuvant ChT +/− RT | 45 (29.4) | 20 (33.3) | 25 (26.8) | 22 (27.5) | 23 (31.5) | 12 (30.0) | 33 (29.2) | |||||
| Palliative ChT | 43 (28.1) | 17 (28.3) | 26 (28.0) | 21 (26.2) | 22 (30.1) | 11 (27.5) | 32 (28.3) | |||||
| Supportive care | 45 (29.4) | 12 (20.0) | 33 (35.5) | 21 (26.2) | 24 (32.9) | 7 (17.5) | 38 (33.6) | |||||
| Systemic treatment, n (%) | 0.04* | 0.54 | 0.06 | |||||||||
| None | 50 (32.7) | 14 (23.3) | 36 (38.7) | 26 (32.5) | 24 (32.9) | 9 (22.5) | 41 (36.3) | |||||
| Monotherapy (gemcitabine/capecitabine) | 54 (35.3) | 29 (48.3) | 25 (26.9) | 32 (40.0) | 22 (30.1) | 21 (52.5) | 33 (29.2) | |||||
| Doublet (Gemox/Xelox/GemNab) | 38 (24.8) | 14 (23.3) | 24 (25.8) | 17 (21.3) | 21 (28.8) | 8 (20.0) | 30 (26.5) | |||||
| Triplet (Folfirinox) | 11 (7.2) | 3 (5.0) | 8 (8.6) | 5 (6.2) | 6 (8.2) | 2 (5.0) | 9 (8.0) | |||||
Group 1, both values of NLR and CA 19-9 were low; Group 2, either one or both values of NLR and CA 19-9 were high. *, P<0.05 indicates statistically significant. NLR, neutrophil-to-lymphocyte ratio; CA 19-9, carbohydrate antigen 19-9; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; cm, centimeters; T, tumor; N, nodes; M, metastasis; ChT, chemotherapy; RT, radiotherapy; Gemox, gemcitabine and oxaliplatin; Xelox, capecitabine and oxaliplatin; GemNab, Gemcitabine and Nab-paclitaxel; Folfirinox, 5-fluorouracil, leucovorin, irinotecan and oxaliplatin.
For the entire cohort the median follow-up was 7.3 months (95% CI: 1.0–78.9), the median PFS was 6.2 months (95% CI: 5.4–7.0) and the median OS was 10.1 months (95% CI: 7.1–13.1). The 1-, 3- and 5-year OS rates were 42%, 11%, and 4.9% respectively, and the 1-, 3- and 5-years PFS were 23.3%, 3.2%, and 2.4% respectively.
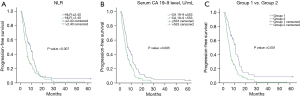
The median OS, 1-, 3- and 5-year survival rates were 13.2 months (95% CI: 11.2–15.1) and 58.7%, 15.1%, and 9.0% respectively in low-NLR group (≤2.4), and 6.7 months (95% CI: 5.6–7.8) and 30.8%, 8.1%, and 2.0% respectively in high-NLR group (>2.4) with a significant difference between two groups (P=0.008). According to CA 19-9 value the median OS, 1-, 3- and 5-year survival rates were 13.1 months (95% CI: 8.9–17.4) and 54.3%, 17.0%, and 8.5% respectively in low-CA 19-9 group (≤553 U/mL); 6.8 months (95% CI: 5.1–8.6) and 28.8%, 3.5%, and 0% respectively in high-CA 19-9 group (>553 U/mL) with a significant difference between both groups (P=0.002). According to the classification groups created combining both values of NLR and CA 19-9, the median OS, 1-, 3- and 5-year survival rates were 15.3 months (95% CI: 13.5–17.0) and 69.4%, 19.7%, and 11.8% respectively in Group 1 (both low-NLR and low-CA 19-9); 6.8 months (95% CI: 5.4–8.2), 31.8%, 7.5% and 1.9% respectively in Group 2 (either one or both high-NLR or CA 19-9) also with a significant difference between groups (P<0.001) (Figure 1A-1C).
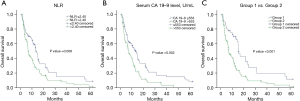
The median PFS, 1-, 3- and 5-year survival rates were 9.0 months (95% CI: 5.9–12), 30.6%, 5.7%, and 5.7% respectively in patients with low-NLR (≤2.4); and 5.6 months (95% CI: 4.6–6.5), 18.5%, 1.3%, and 0% respectively in patients with high-NLR (>2.4) with a significant difference between two groups (P=0.007). According to CA 19-9 value the median PFS, 1-, 3- and 5-year survival rates were 6.9 months (95% CI: 4.8–9.0) and 28.7%, 5.5%, and 4.1% respectively in patients with low-CA 19-9 (≤553 U/mL); and 5.0 months (95% CI: 3.9–6.2), 17.4%, 0% and 0% respectively in patients with high-CA 19-9 (>553 U/mL) with a significant difference between two groups (P=0.005). According to the classification groups created combining both values of NLR and CA 19-9, the median PFS, 1-, 3- and 5-year survival rates were 10.9 months (95% CI: 9.0–12.9), 39.9%, 8.6% and 8.6% respectively in Group 1 (both low-NLR and low-CA 19-9); and 5.4 months (95% CI: 4.6–6.3), 17.4%, 1.1%, and 0% respectively in Group 2 (either one or both high-NLR or CA 19-9) with a significant difference between groups (P=0.001) (Figure 2A-2C).
Univariate and multivariate survival analyses
Cox regression analysis was performed to determine factors associated with OS and PFS. In multivariate analysis ECOG-PS, tumor differentiation, presence of metastases, global treatment received, systemic treatment received, NLR value, serum CA 19-9 value and classification group combining NLR and CA 19-9 values were identified as independent prognostic factors for OS (Table 2).
Table 2
| Variable | Total (events) | Median OS (95% CI), months | Univariate analysis, P value | Multivariate analysis | |
|---|---|---|---|---|---|
| HR (95% CI) | P value | ||||
| Age, n (%) | 0.18 | ||||
| ≤65 years | 107 (69.9) | 10.7 (7.6–13.9) | |||
| >65 years | 46 (30.1) | 6.5 (1.4–11.6) | |||
| Gender, n (%) | 0.91 | ||||
| Female | 72 (47.1) | 9.3 (5.3–13.4) | |||
| Male | 81 (52.9) | 10.7 (6.0–15.5) | |||
| BMI (kg/m2), n (%) | 0.76 | ||||
| <18.5 | 5 (3.3) | 3.7 (0) | |||
| 18.5–24.9 | 83 (54.2) | 10.7 (5.7–15.8) | |||
| 25–29.9 | 44 (28.8) | 9.3 (4.9–13.8) | |||
| ≥30 | 21 (13.7) | 6.8 (1.4–12.2) | |||
| ECOG-PS, n (%) | 0.01 | 2.008 (1.235–3.265) | 0.005 | ||
| 0–1 | 127 (83.0) | 10.8 (7.8–13.7) | |||
| ≥2 | 26 (17.0) | 6.2 (3.0–9.4) | |||
| Tumor location, n (%) | 0.24 | ||||
| Head | 134 (87.6) | 10.7 (7.4–14.1) | |||
| Body-tail | 19 (12.4) | 8.0 (3.4–12.7) | |||
| Tumor differentiation, n (%) | 0.001 | 1.644 (1.249–2.164) | <0.001 | ||
| Well/moderate | 55 (35.9) | 12.8 (8.7–17.0) | |||
| Poor | 24 (15.6) | 6.5 (3.0–9.9) | |||
| Vascular invasion, n (%) | 0.28 | ||||
| No | 61 (39.9) | 10.7 (7.2–14.3) | |||
| Yes | 92 (60.1) | 8.6 (5.1–12.2) | |||
| Tumor size, n (%) | 0.37 | ||||
| ≤4 cm | 73 (47.7) | 10.5 (5.6–15.5) | |||
| >4 cm | 80 (52.3) | 8.6 (4.8–12.5) | |||
| T, n (%) | 0.06 | ||||
| T1 | 10 (6.5) | 16.7 (9.9–23.6) | |||
| T2–T4 | 143 (93.5) | 9.4 (6.6–12.3) | |||
| N, n (%) | 0.20 | ||||
| N0 | 53 (34.6) | 12.8 (9.7–16.0) | |||
| N+ | 100 (65.4) | 7.1 (3.7–10.4) | |||
| M, n (%) | <0.001 | 2.492 (1.415–4.389) | 0.002 | ||
| M0 | 84 (54.9) | 13.2 (9.3–17.0) | |||
| M1 | 69 (45.1) | 5.8 (4.1–7.6) | |||
| Global treatment, n (%) | <0.001 | 2.440 (1.763–3.378) | <0.001 | ||
| Surgery followed by ChT | 20 (13.1) | 21.6 (8.3–34.8) | |||
| Neoadjuvant ChT +/− RT | 45 (29.4) | 16.7 (12.0–21.4) | |||
| Palliative ChT | 43 (28.1) | 7.1 (1.4–12.7) | |||
| Supportive care | 45 (29.4) | 3.0 (2.4–3.6) | |||
| Systemic treatment, n (%) | <0.001 | 0.639 (0.507–0.806) | <0.001 | ||
| None | 50 (32.7) | 3.4 (2.6–4.1) | |||
| Monotherapy (gemcitabine/capecitabine) | 54 (35.3) | 14.2 (11.9–16.4) | |||
| Doublet (Gemox/Xelox/GemNab) | 38 (24.8) | 11.5 (8.7–14.3) | |||
| Triplet (Folfirinox) | 11 (7.2) | 17.8 (7.4–28.1) | |||
| NLR | 0.008 | 1.653 (1.135–2.408) | 0.009 | ||
| ≤2.4 | 60 (39.2) | 13.2 (11.2–15.1) | |||
| >2.4 | 93 (60.8) | 6.7 (5.6–7.8) | |||
| CA 19-9, U/mL | 0.002 | 1.787 (1.237–2.582) | 0.002 | ||
| ≤553 | 80 (52.3) | 13.1 (8.9–17.4) | |||
| >553 | 73 (47.7) | 6.8 (5.1–8.6) | |||
| Groups | <0.001 | 2.127 (1.383–3.272) | 0.001 | ||
| Group 1 | 40 (26.1) | 15.3 (13.5–17.0) | |||
| Group 2 | 113 (73.9) | 6.8 (5.4–8.2) | |||
Group 1, both values of NLR and CA 19-9 were low; Group 2, either one or both values of NLR and CA 19-9 were high. OS, overall survival; CI, confidence interval; HR, hazard ratio; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; cm, centimeters; T, tumor; N, nodes; M, metastasis; ChT, chemotherapy; RT, radiotherapy; Gemox, gemcitabine and oxaliplatin; Xelox, capecitabine and oxaliplatin; GemNab, gemcitabine and Nab-paclitaxel; Folfirinox, 5-fluorouracil, leucovorin, irinotecan and oxaliplatin; NLR, neutrophil-to-lymphocyte ratio; CA 19-9, carbohydrate antigen 19-9.
In multivariate analysis, presence of metastases, global treatment received, systemic treatment received, NLR value, CA 19-9 value and classification group combining NLR and CA 19-9 values were identified as independent prognostic factors for PFS (Table 3).
Table 3
| Variable | Total (events) | Median PFS (95% CI), months | Univariate analysis, P value | Multivariate analysis | |
|---|---|---|---|---|---|
| HR (95% CI) | P value | ||||
| Age, n (%) | 0.40 | ||||
| ≤65 years | 107 (69.9) | 6.2 (5.1–7.4) | |||
| >65 years | 46 (30.1) | 6.2 (3.9–8.5) | |||
| Gender, n (%) | 0.79 | ||||
| Female | 72 (47.1) | 5.7 (4.5–6.8) | |||
| Male | 81 (52.9) | 6.7 (5.0–8.5) | |||
| BMI (kg/m2), n (%) | 0.55 | ||||
| <18.5 | 5 (3.3) | 3.7 (1.7–5.8) | |||
| 18.5–24.9 | 83 (54.2) | 6.2 (5.4–7.1) | |||
| 25–29.9 | 44 (28.8) | 6.6 (3.6–9.5) | |||
| ≥30 | 21 (13.7) | 5.3 (4.7–5.8) | |||
| ECOG-PS, n (%) | 0.045 | 1.043 (0.434–2.506) | 0.92 | ||
| 0–1 | 127 (83.0) | 6.3 (5.1–7.6) | |||
| ≥2 | 26 (17.0) | 3.8 (0.6–7.0) | |||
| Tumor location, n (%) | 0.15 | ||||
| Head | 134 (87.6) | 6.3 (5.5–7.2) | |||
| Body-tail | 19 (12.4) | 5.3 (4.7–5.8) | |||
| Tumor differentiation, n (%) | 0.002 | 1.313 (0.977–1.764) | 0.07 | ||
| Well/moderate | 8 (5.2) | 8.6 (5.3–12.0) | |||
| Poor | 47 (30.7) | 4.9 (2.7–7.0) | |||
| Vascular invasion, n (%) | 0.02 | 0.823 (0.460–1.475) | 0.51 | ||
| No | 61 (39.9) | 6.9 (3.3–10.5) | |||
| Yes | 92 (60.1) | 5.6 (4.3–6.8) | |||
| Tumor size, n (%) | 0.02 | 1.210 (0.669–2.188) | 0.52 | ||
| ≤4 cm | 73 (47.7) | 6.9 (5.2–8.5) | |||
| >4 cm | 80 (52.3) | 5.6 (4.5–6.6) | |||
| T, n (%) | 0.04 | 0.923 (0.325–2.616) | 0.88 | ||
| T1 | 10 (6.5) | 16.4 (8.7–24.2) | |||
| T2–T4 | 143 (93.5) | 5.9 (5.1–6.7) | |||
| N, n (%) | 0.03 | 1.092 (0.596–2.000) | 0.77 | ||
| N0 | 53 (34.6) | 7.0 (4.2–9.7) | |||
| N+ | 100 (65.4) | 5.6 (4.6–6.6) | |||
| M, n (%) | <0.001 | 1.403 (0.991–1.987) | 0.049 | ||
| M0 | 84 (54.9) | 8.6 (6.3–10.9) | |||
| M1 | 69 (45.1) | 4.6 (3.4–5.8) | |||
| Global treatment, n (%) | <0.001 | <0.001 | |||
| Surgery followed by ChT | 20 (13.1) | 14.4 (9.5–19.1) | 1.983 (1.573–2.499) | ||
| Neoadjuvant ChT +/− RT | 45 (29.4) | 10.6 (8.2–13.0) | |||
| Palliative ChT | 43 (28.1) | 5.4 (4.4–6.5) | |||
| Supportive care | 45 (29.4) | 2.7 (2.4–3.0) | |||
| Systemic treatment, n (%) | <0.001 | 1.724 (1.100–2.703) | 0.01 | ||
| None | 50 (32.7) | 2.8 (2.3–3.2) | |||
| Monotherapy (gemcitabine/capecitabine) | 54 (35.3) | 8.12 (6.1–10.2) | |||
| Doublet (Gemox/Xelox/GemNab) | 38 (24.8) | 7.6 (2.6–12.5) | |||
| Triplet (Folfirinox) | 11 (7.2) | 11.8 (2.8–20.7) | |||
| NLR | 0.007 | 1.511 (1.074–2.126) | 0.01 | ||
| ≤2.4 | 60 (39.2) | 9.0 (5.9–12.0) | |||
| >2.4 | 93 (60.8) | 5.6 (4.6–6.5) | |||
| CA 19-9, U/mL | 0.005 | 1.606 (1.149–2.246) | 0.006 | ||
| ≤553 | 80 (52.3) | 6.9 (4.8–9.0) | |||
| >553 | 73 (47.7) | 5.0 (3.9–6.2) | |||
| Groups | 0.001 | 1.961 (1.327–2.897) | 0.001 | ||
| Group 1 | 40 (26.1) | 10.9 (9.0–12.9) | |||
| Group 2 | 113 (73.9) | 5.4 (4.6–6.3) | |||
Group 1, both values of NLR and CA 19-9 were low; Group 2, either one or both values of NLR and CA 19-9 were high. PFS, progression-free survival; CI, confidence interval; HR, hazard ratio; BMI, body mass index; ECOG, Eastern Cooperative Oncology Group; PS, performance status; cm, centimeters; T, tumor; N, nodes; M, metastasis; ChT, chemotherapy; RT, radiotherapy; Gemox, gemcitabine and oxaliplatin; Xelox, capecitabine and oxaliplatin; GemNab, gemcitabine and Nab-paclitaxel; Folfirinox, 5-fluorouracil, leucovorin, irinotecan and oxaliplatin; NLR, neutrophil-to-lymphocyte ratio; CA 19-9, carbohydrate antigen 19-9.
Discussion
Key findings
Pancreatic cancer is one of the leading causes of cancer-related deaths globally, and even in patients who receive optimal treatment for each stage, the prognosis is dismal. Therefore, it is of utmost importance to identify prognostic biomarkers that will help us to select patients who may benefit from more aggressive treatment strategies (neoadjuvant chemotherapy and/or radiation) and closer follow-up to prevent and diagnose early recurrences respectively.
The present study demonstrated that high-NLR (>2.4) and high-CA 19-9 (>553 U/mL) values used separately are both independently associated with poorer OS and PFS in patients with pancreatic cancer of all stages.
The classification of two groups we created by combining both NLR and serum CA 19-9 values showed better prognostic significance on OS and PFS than when both biomarkers are used separately.
Strengths and limitations
Limitations of this study are that it is a retrospective single-center study with a relatively small number of patients. A definitive optimal cut-off value for NLR and CA 19-9 has not been established and differences between studies may be explained by the different stages of pancreatic cancer and the number of patients included in studies. A larger prospective multicenter study is needed to determine and validate the optimal cut-off values of these biomarkers and their prognostic importance used separately and in combination.
Comparison with similar researches
The prognostic significance of NLR in pancreatic cancer was explored by another study and is matching with our cut-off (2.4), different levels in other studies ranged from 2.62 to 3.74. In general, all the results reveal that a high NLR at the time of diagnosis or post-treatment could be an independent indicator of poor prognosis and is associated with metastatic stage in patients with pancreatic cancer (15,16,30). Kim et al. identified a high NLR (>2.8) and CA 19-9 (>70 U/mL) as independent predictors of worse disease-free survival (DFS), but only high CA 19-9 and not high NLR as independent predictor of worse OS, combining both values they found patients with both high-NLR and high-CA 19-9 levels to have worse OS and recurrence rates, however this study only enrolled resected patients with pancreatic head cancer (31). Song et al. also demonstrated that high NLR (>3.75) and CA 19-9 (>626 U/mL) are independently associated with worse OS and that the combined use of both in similar classification groups to ours better predicts OS than when both values used separately, but this study was limited to metastatic patients and only analyzed association with OS and not with PFS (32). Asaoka et al. similarly to us demonstrated the prognostic utility of the combination of these two parameters, showing that when one of these parameters NLR or CA 19-9 was elevated above their cut-off values, OS and DFS were significantly poorer than those in patients with both low CA 19-9 and NLR, however, their analysis was restricted to a small group of surgically resected pancreatic head cancer patients (29).
Explanations of findings
In this study, we evaluated serum CA 19-9 and NLR values at diagnosis and the combination of these two values in a simple classification as prognostic factors for patients with pancreatic cancer of all stages in a single referral center and demonstrated that elevated CA 19-9 and NLR values were independent predictors of worse OS and PFS. Moreover, the combination of these two parameters seems to better predict prognosis according to multivariate analysis, and patients with both low-NLR and low-CA 19-9 (Group 1) showed better OS and DFS when compared with patients with either one or both high-NLR or high-CA 19-9 (Group 2).
The cut-off value obtained in our cohort for CA 19-9 was 553 U/mL, and patients with CA 19-9 above this level were associated with larger tumor size, higher proportion of metastatic disease at diagnosis, and worse PFS and OS. Several studies have demonstrated that high levels of serum CA 19-9 are associated with worse prognosis in pancreatic cancer patients in different clinical settings and with variable cut-off values reported (33,34). However, the main limitations in the use of CA 19-9 alone as a reliable biomarker in patients with pancreatic cancer are that up to 10% of the population does not produce it and the false positive elevation in patients with obstructive jaundice which could lead to a misinterpretation of serum CA 19-9 levels for prognosis purposes.
Regarding NLR, the cut-off value obtained in this study was 2.4 with patients showing worse PFS and OS when NLR was above this level and was also associated with poorer performance status, higher proportion of nodal disease at diagnosis, and lesser likelihood to receive oncologic treatment. Chen et al. reported a cut-off value of 2.78 for NLR in advanced pancreatic cancer, with high-NLR independently associated with worse OS (35). Luo et al. determined an NLR cut-off value of 3.1 as an independent prognostic factor for OS in patients with advanced pancreatic cancer undergoing chemotherapy (36). Similar to our study, Shin et al. reported an NLR cut-off value of 2.6 to have prognostic significance for both PFS and OS, but this study only included patients with advanced pancreatic cancer receiving first-line chemotherapy (15). Also, Dogan et al. reported NRL with a cut-off value of 3.0 to be an independent prognostic factor for OS and PFS but they included only patients with metastatic pancreatic cancer in their study (5). Previous meta-analysis demonstrated that pancreatic cancer patients with low NLR have longer OS and DFS compared to patients with high NLR (16,24,37,38) which is consistent with our results.
Cetin et al. showed that high NLR (>3.5) and CA 19-9 levels (>437 U/mL) are both independently associated with worse OS in patients with metastatic pancreas cancer (39). Similarly, Asaoka et al. demonstrated pretreatment serum CA 19-9 >230 U/mL and NLR >2.7 were independent risk factors for poorer OS and DFS in surgically resected pancreatic cancer patients (29).
Furthermore, the classification of two groups we created by combining both NLR and serum CA 19-9 values showed better prognostic significance on OS and PFS than when both biomarkers are used separately as demonstrated with survival analysis and multivariate analysis. Also using our classification groups, Group 2 patients (either one or both high-NLR or high-CA 19-9 levels) were significantly associated with poorer performance status, higher occurrence of tumor vascular involvement, larger tumor size, higher proportion of metastatic disease at diagnosis, more advanced clinical stage, and less proportion of patients undergoing surgery and more patients receiving best supportive care compared with Group 1 patients (both low-NLR and low-CA 19-9 levels).
Implications and actions needed
Currently CA 19-9 is the most widely used and endorsed biomarker for PDAC, useful for decision of initial treatment, monitoring of treatment response, prognosis and follow-up in PDAC patients (15). Nevertheless, up to 10% of patients do not produce and thus do not elevate CA 19-9 (40) and different biomarkers other than CA 19-9 would be useful and necessary in this group of patients to predict tumor recurrence or progression. Inflammation plays a role in cancer initiation and progression, and tumor suppression by immune cells such as lymphocytes is impaired by inflammatory cascade in addition to cancer cells (41). Moreover, PDAC specially seems to be associated with lymphocytopenia (42). The NLR, a biomarker that reflects the systemic immune and inflammatory responses, has demonstrated a prognostic significance in patients with pancreatic cancer in specific different clinical stages and scenarios (16,43-45). However, few studies have evaluated its prognostic impact in pancreatic cancer patients of all clinical stages regardless of the treatment received (29). NLR and serum CA 19-9 used independently and especially combined are useful as predictors of OS and PFS in patients with pancreatic cancer, the classification we propose using both NLR and serum CA 19-9 levels could be a better prognostic tool to guide and optimize treatment and follow-up strategies than NLR and serum CA 19-9 levels used separately. Also, both biomarkers are accessible, inexpensive and readily measurable which may facilitate and expand their use and the classification we propose is simple, practical and easy to apply.
Conclusions
Our results demonstrated that in patients with PDAC, regardless stage and treatment, high-NLR and high-CA 19-9 levels at diagnosis are both independent prognostic factors for worse DFS and OS when used separately and that the combination of these two biomarkers seems to better predict prognosis and stratify patients to guide treatment and surveillance strategies than when used separately. Although a specific cut-off value has not been established, our study has demonstrated the prognostic utility of the combination of NLR and CA 19-9, when both parameters are elevated, they have worse survival than patients with both parameters below the cut-off point and assume disease in advanced stages. Furthermore, the implementation of these parameters is a great option since they are very practical to calculate in daily clinical practice. Furthermore, the implementation of these parameters is a great option since they are very practical to calculate in daily clinical practice.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-893/rc
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-893/dss
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-893/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-23-893/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Ethics Committee of Instituto Nacional de Cancerología (No. 2023/020) and individual consent for this retrospective analysis was waived.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Rahib L, Smith BD, Aizenberg R, et al. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res 2014;74:2913-21. [Crossref] [PubMed]
- Puckett Y, Garfield K. Pancreatic Cancer. In: StatPearls. Treasure Island (FL): StatPearls Publishing; September 26, 2022.
- Ferrone CR, Pieretti-Vanmarcke R, Bloom JP, et al. Pancreatic ductal adenocarcinoma: long-term survival does not equal cure. Surgery 2012;152:S43-9. [Crossref] [PubMed]
- Lee T, Teng TZJ, Shelat VG. Carbohydrate antigen 19-9 - tumor marker: Past, present, and future. World J Gastrointest Surg 2020;12:468-90. [Crossref] [PubMed]
- Dogan M, Algin E, Guven ZT, et al. Neutrophil-lymphocyte ratio, platelet-lymphocyte ratio, neutrophil-platelet score and prognostic nutritional index: do they have prognostic significance in metastatic pancreas cancer? Curr Med Res Opin 2018;34:857-63. [Crossref] [PubMed]
- Goonetilleke KS, Siriwardena AK. Systematic review of carbohydrate antigen (CA 19-9) as a biochemical marker in the diagnosis of pancreatic cancer. Eur J Surg Oncol 2007;33:266-70. [Crossref] [PubMed]
- Sugiura T, Uesaka K, Kanemoto H, et al. Serum CA19-9 is a significant predictor among preoperative parameters for early recurrence after resection of pancreatic adenocarcinoma. J Gastrointest Surg 2012;16:977-85. [Crossref] [PubMed]
- Hartwig W, Strobel O, Hinz U, et al. CA19-9 in potentially resectable pancreatic cancer: perspective to adjust surgical and perioperative therapy. Ann Surg Oncol 2013;20:2188-96. [Crossref] [PubMed]
- Humphris JL, Chang DK, Johns AL, et al. The prognostic and predictive value of serum CA19.9 in pancreatic cancer. Ann Oncol 2012;23:1713-22. [Crossref] [PubMed]
- Kannagi R. Carbohydrate antigen sialyl Lewis a--its pathophysiological significance and induction mechanism in cancer progression. Chang Gung Med J 2007;30:189-209. [PubMed]
- Kishimoto T, Ishikura H, Kimura C, et al. Phenotypes correlating to metastatic properties of pancreas adenocarcinoma in vivo: the importance of surface sialyl Lewis(a) antigen. Int J Cancer 1996;69:290-4. [Crossref] [PubMed]
- Saad ED, Machado MC, Wajsbrot D, et al. Pretreatment CA 19-9 level as a prognostic factor in patients with advanced pancreatic cancer treated with gemcitabine. Int J Gastrointest Cancer 2002;32:35-41. [Crossref] [PubMed]
- Maisey NR, Norman AR, Hill A, et al. CA19-9 as a prognostic factor in inoperable pancreatic cancer: the implication for clinical trials. Br J Cancer 2005;93:740-3. [Crossref] [PubMed]
- Boeck S, Stieber P, Holdenrieder S, et al. Prognostic and therapeutic significance of carbohydrate antigen 19-9 as tumor marker in patients with pancreatic cancer. Oncology 2006;70:255-64. [Crossref] [PubMed]
- Shin K, Jung EK, Park SJ, et al. Neutrophil-to-lymphocyte ratio and carbohydrate antigen 19-9 as prognostic markers for advanced pancreatic cancer patients receiving first-line chemotherapy. World J Gastrointest Oncol 2021;13:915-28. [Crossref] [PubMed]
- Iwai N, Okuda T, Sakagami J, et al. Neutrophil to lymphocyte ratio predicts prognosis in unresectable pancreatic cancer. Sci Rep 2020;10:18758. [Crossref] [PubMed]
- Galizia G, Lieto E, Zamboli A, et al. Neutrophil to lymphocyte ratio is a strong predictor of tumor recurrence in early colon cancers: A propensity score-matched analysis. Surgery 2015;158:112-20. [Crossref] [PubMed]
- Dong YW, Shi YQ, He LW, et al. Prognostic significance of neutrophil-to-lymphocyte ratio in rectal cancer: a meta-analysis. Onco Targets Ther 2016;9:3127-34. [PubMed]
- Azab B, Bhatt VR, Phookan J, et al. Usefulness of the neutrophil-to-lymphocyte ratio in predicting short- and long-term mortality in breast cancer patients. Ann Surg Oncol 2012;19:217-24. [Crossref] [PubMed]
- Zhao QT, Yang Y, Xu S, et al. Prognostic role of neutrophil to lymphocyte ratio in lung cancers: a meta-analysis including 7,054 patients. Onco Targets Ther 2015;8:2731-8. [PubMed]
- Kim EY, Song KY. The preoperative and the postoperative neutrophil-to-lymphocyte ratios both predict prognosis in gastric cancer patients. World J Surg Oncol 2020;18:293. [Crossref] [PubMed]
- Li B, Xiong F, Yi S, et al. Prognostic and Clinicopathologic Significance of Neutrophil-to-Lymphocyte Ratio in Esophageal Cancer: An Update Meta-Analysis. Technol Cancer Res Treat 2022;21:15330338211070140. [Crossref] [PubMed]
- Wang DS, Luo HY, Qiu MZ, et al. Comparison of the prognostic values of various inflammation based factors in patients with pancreatic cancer. Med Oncol 2012;29:3092-100. [Crossref] [PubMed]
- Cheng H, Long F, Jaiswar M, et al. Prognostic role of the neutrophil-to-lymphocyte ratio in pancreatic cancer: a meta-analysis. Sci Rep 2015;5:11026. [Crossref] [PubMed]
- Watanabe J, Otani S, Sakamoto T, et al. Prognostic indicators based on inflammatory and nutritional factors after pancreaticoduodenectomy for pancreatic cancer. Surg Today 2016;46:1258-67. [Crossref] [PubMed]
- Chawla A, Huang TL, Ibrahim AM, et al. Pretherapy neutrophil to lymphocyte ratio and platelet to lymphocyte ratio do not predict survival in resectable pancreatic cancer. HPB (Oxford) 2018;20:398-404. [Crossref] [PubMed]
- Jamieson NB, Denley SM, Logue J, et al. A prospective comparison of the prognostic value of tumor- and patient-related factors in patients undergoing potentially curative surgery for pancreatic ductal adenocarcinoma. Ann Surg Oncol 2011;18:2318-28. [Crossref] [PubMed]
- Garcea G, Ladwa N, Neal CP, et al. Preoperative neutrophil-to-lymphocyte ratio (NLR) is associated with reduced disease-free survival following curative resection of pancreatic adenocarcinoma. World J Surg 2011;35:868-72. [Crossref] [PubMed]
- Asaoka T, Miyamoto A, Maeda S, et al. Prognostic impact of preoperative NLR and CA19-9 in pancreatic cancer. Pancreatology 2016;16:434-40. [Crossref] [PubMed]
- Onoe S, Maeda A, Takayama Y, et al. The Prognostic Impact of the Lymphocyte-to-Monocyte Ratio in Resected Pancreatic Head Adenocarcinoma. Med Princ Pract 2019;28:517-25. [Crossref] [PubMed]
- Kim WJ, Lim TW, Park PJ, et al. Prognostic impact of the combination of the neutrophil-to-lymphocyte ratio and serum carbohydrate antigen 19-9 in patients with pancreas head cancer. ANZ J Surg 2019;89:E302-E307. [Crossref] [PubMed]
- Song JY, Chen MQ, Guo JH, et al. Combined pretreatment serum CA19-9 and neutrophil-to-lymphocyte ratio as a potential prognostic factor in metastatic pancreatic cancer patients. Medicine (Baltimore) 2018;97:e9707. [Crossref] [PubMed]
- Combs SE, Habermehl D, Kessel KA, et al. Prognostic impact of CA 19-9 on outcome after neoadjuvant chemoradiation in patients with locally advanced pancreatic cancer. Ann Surg Oncol 2014;21:2801-7. [Crossref] [PubMed]
- Reitz D, Gerger A, Seidel J, et al. Combination of tumour markers CEA and CA19-9 improves the prognostic prediction in patients with pancreatic cancer. J Clin Pathol 2015;68:427-33. [Crossref] [PubMed]
- Chen Y, Yan H, Wang Y, et al. Significance of baseline and change in neutrophil-to-lymphocyte ratio in predicting prognosis: a retrospective analysis in advanced pancreatic ductal adenocarcinoma. Sci Rep 2017;7:753. [Crossref] [PubMed]
- Luo G, Guo M, Liu Z, et al. Blood neutrophil-lymphocyte ratio predicts survival in patients with advanced pancreatic cancer treated with chemotherapy. Ann Surg Oncol 2015;22:670-6. [Crossref] [PubMed]
- Mowbray NG, Griffith D, Hammoda M, et al. A meta-analysis of the utility of the neutrophil-to-lymphocyte ratio in predicting survival after pancreatic cancer resection. HPB (Oxford) 2018;20:379-84. [Crossref] [PubMed]
- Yang JJ, Hu ZG, Shi WX, et al. Prognostic significance of neutrophil to lymphocyte ratio in pancreatic cancer: a meta-analysis. World J Gastroenterol 2015;21:2807-15. [Crossref] [PubMed]
- Cetin S, Dede I. Prognostic value of the neutrophil-to-lymphocyte ratio and carbohydrate antigen 19-9 in estimating survival in patients with metastatic pancreatic cancer. J Cancer Res Ther 2020;16:909-16. [Crossref] [PubMed]
- Tempero MA, Uchida E, Takasaki H, et al. Relationship of carbohydrate antigen 19-9 and Lewis antigens in pancreatic cancer. Cancer Res 1987;47:5501-3. [PubMed]
- Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet 2001;357:539-45. [Crossref] [PubMed]
- Fogar P, Sperti C, Basso D, et al. Decreased total lymphocyte counts in pancreatic cancer: an index of adverse outcome. Pancreas 2006;32:22-8. [Crossref] [PubMed]
- Hasegawa S, Eguchi H, Tomokuni A, et al. Pre-treatment neutrophil to lymphocyte ratio as a predictive marker for pathological response to preoperative chemoradiotherapy in pancreatic cancer. Oncol Lett 2016;11:1560-6. [Crossref] [PubMed]
- Alagappan M, Pollom EL, von Eyben R, et al. Albumin and Neutrophil-Lymphocyte Ratio (NLR) Predict Survival in Patients With Pancreatic Adenocarcinoma Treated With SBRT. Am J Clin Oncol 2018;41:242-7. [Crossref] [PubMed]
- Reddy AV, Hill CS, Sehgal S, et al. High neutrophil-to-lymphocyte ratio following stereotactic body radiation therapy is associated with poor clinical outcomes in patients with borderline resectable and locally advanced pancreatic cancer. J Gastrointest Oncol 2022;13:368-79. [Crossref] [PubMed]


