
Fruquintinib in metastatic colorectal cancer: a multicenter real-world analysis on efficacy, safety, and predictive and prognostic factors
Highlight box
Key findings
• Fruquintinib showed encouraging antitumor activity and controllable safety in metastatic colorectal cancer. L3 skeletal muscle index (SMI), brain metastasis and carcinoembryonic antigen (CEA) could serve as potential markers for patient selection.
What is known and what is new?
• The real-world efficacy and safety of fruquintinib in advanced colorectal cancer patients are numerically superior to that in the previous phase III studies.
• Multivariate analysis suggested that brain metastasis, decreased L3 SMI >5%, and baseline CEA level as independent predictors of overall survival.
What is the implication, and what should change now?
• Due to the design bias and other limitations, additional trial with large samples is needed.
Introduction
Colorectal cancer (CRC) is one of the most common cancers, ranking second for cancer-related deaths worldwide (1). It is estimated that over 1.2 million new CRC cases are diagnosed annually and the disease-related mortality is about 33% (2). Although CRC ranks second in terms of incidence among the Chinese population, there is a trend of increasing incidence, with about 517,100 new cases per year in China (3).
Treatment of metastatic CRC (mCRC) is based on cytotoxic drugs and targeted agents. Currently, the standard first- and second-line treatment for mCRC is oxaliplatin, irinotecan, and fluoropyrimidine-based chemotherapy in combination with bevacizumab or cetuximab [KRAS wild-type, epidermal growth factor receptor (EGFR)-expressing] (2). The third-line treatment options in China include regorafenib, fruquintinib, and trifluridine/tipiracil (TAS-102).
Fruquintinib is a highly selective and orally administered tyrosine kinase inhibitor (TKI) targeting vascular endothelial growth factor receptors (VEGFRs), which inhibits VEGFR phosphorylation, endothelial cell proliferation, and tubule formation (4). Fruquintinib was approved in China for patients with metastatic CRC who had failed at least two prior systemic anti-neoplastic therapies, including fluorouracil, oxaliplatin, and irinotecan, with or without prior use of anti-VEGF or anti-EGFR therapy (5). The FRESCO and FRESCO-2 study, which are pivotal Phase III clinical trials, demonstrated that fruquintinib was well tolerated with consistent efficacy in mCRC patients in both China and worldwide (6). In the FRESCO study, median overall survival (mOS) was significantly prolonged with fruquintinib compared with placebo [9.3 months, 95% confidence interval (CI): 8.2–10.5 vs. 6.6 months, 95% CI: 5.9–8.1]; hazard ratio (HR) for death, 0.65 (95% CI: 0.51–0.83; P<0.001). Median progression-free survival (mPFS) was also significantly increased with fruquintinib (3.7 months, 95% CI: 3.7–4.6 vs. 1.8 months, 95% CI: 1.8–1.8 months); HR for progression or death, 0.26 (95% CI: 0.21–0.34; P<0.001) (7). In the FRESCO-2 study, the mOS was 7.4 months in the fruquintinib group (n=461) vs. 4.8 months in the placebo group (n=230) (HR 0.66; 95% CI: 0.55–0.80; P<0.001). mPFS was 3.7 months in the fruquintinib group vs. 1.8 months in the placebo group (HR 0.32; 95% CI: 0.27–0.39; P<0.001) (8).
Fruquintinib was approved in China by the National Medical Products Administration (NMPA) in 2018, and some retrospective studies have verified its clinical efficacy and safety (9,10). However, the sample size is relatively small or there is only a safety evaluation, and it remains unclear, how to identify the specific patients who are able to achieve significant survival benefits from fruquintinib. The aim of this study was to analyze efficacy, safety, and predictive and prognostic factors of fruquintinib; thus, we could assess its curative effect and create a prognosis prediction model. We present this article in accordance with the STROBE reporting checklist (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-559/rc).
Methods
Patients
This study analyzed mCRC patients who underwent fruquintinib therapy from seven cancer centers in Ningbo, Zhejiang Province. The inclusion criteria were as follows: histologically confirmed mCRC; Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–2; at least one completed course of fruquintinib. Baseline information were recorded, including patient demographics, clinical characteristics, drug dose, prior treatment lines, metastatic sites, and so on. Efficacy and safety data of the enrolled patients were also collected. The patients who met the enrollment criteria to receive fruquintinib, either as a single agent or in combination, with monthly follow-up including adverse reaction recording, and efficacy assessment every 2 months and L3 skeletal muscle index (SMI) recorded until disease progression or intolerable adverse effects.
Image collection and analysis
An experienced radiologist evaluated radiographic sarcopenia in this study. The skeletal muscle area in the third lumbar plane was used as the measurement criterion, including psoas, paraspinous, and abdominal wall muscles. Computed tomography (CT) scans acquired at the baseline were recorded as CT1, and the first follow up CT assessment during therapy was recorded as CT2. All CT examinations were required to have both plain and enhanced scan. L3 SMI is defined as skeletal muscle area (SMA; cm2) of the skeletal muscle at L3 level/square of the patient’s height (m2) on CT tomography (11,12).
Parameters and statistical analysis
Referring to cut-off values for sarcopenia in the Chinese population, it was defined as males 40.8 cm2/m2 and females 34.9 cm2/m2, and this was used for population analysis in this study (13). Predictive and prognostic value of baseline sarcopenia and subsequent skeletal muscle loss (SML) (at least 5% reduction in SMI compared to baseline) were analyzed. Tumor assessment was performed every 2 cycles according to the Response Evaluation Criteria in Solid Tumors (RECIST) v1.1, and adverse effects (AEs) were classified and graded according to Common Terminology Criteria for Adverse Events (CTCAE) v 5.0. The software SPSS 20.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis; chi-square test was used for univariate analysis, factors influencing progression-free survival (PFS) and overall survival (OS) after primary screening, followed by Cox regression for multivariate analysis, to find independent factors related to prediction and prognosis. mPFS and mOS were calculated using the Kaplan-Meier method and survival curves were plotted.
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ningbo No. 2 Hospital Human Research Ethics Committee (No. PJ-NBEY-KY-2019-146-01) and informed consent was taken from all the patients. All participating hospitals/institutions were informed and agreed with this study.
Results
Clinical characteristics of patients
From January 2020 to January 2022, a total of 140 patients were selected and included in this study. The cut-off date was 30 July 2022. The median follow-up time 18.3 months (range, 6–29.3 months) and the median age was 63 years (range, 32–81 years). Most patients had good performance status (ECOG PS 0–1: 85%). The primary tumor site was mainly rectal cancer (51.4%), and metastases sites were as follows: liver metastasis (55.7%), lung metastasis (58.6%), lymph node metastasis (37.1%), brain metastasis (8.9%), and bone metastasis (11.3%). The median initial dose was 3.85 mg and the median relative dose intensity was 80%.
A total of 76 patients with completed CT1 and CT2 results were included in SMI analysis. The median SMI values for CT1 and CT2 were 40.3 (range, 23.1–62) and 39.2 (range, 21.1–53.9), respectively. According to the predefined criteria, 43 (56.6%) patients were identified as sarcopenia at the baseline measurements. During follow-up, SMI remained relatively stable, the majority of patients (74.3%) having decreases in SMI of ≤5% (as shown in Table 1).
Table 1
| Characteristics | No. patients (%) |
|---|---|
| Age | |
| <70 years | 106 (75.7) |
| ≥70 years | 34 (24.3) |
| Gender | |
| Male | 92 (65.7) |
| Female | 48 (34.3) |
| PS score | |
| 0 to 1 | 119 (85.0) |
| 2 | 21 (15.0) |
| BMI, kg/m2 | |
| <18.5 | 11 (7.9) |
| ≥18.5 | 129 (92.1) |
| Liver metastases | |
| Yes | 78 (55.7) |
| No | 62 (44.3) |
| Lung metastases | |
| Yes | 82 (58.6) |
| No | 58 (41.4) |
| Lymphatic metastasis | |
| Yes | 52 (37.1) |
| No | 88 (62.9) |
| Pelvic metastasis | |
| Yes | 32 (22.9) |
| No | 108 (77.1) |
| Brain metastasis | |
| Yes | 5 (3.6) |
| No | 135 (96.4) |
| Bone metastasis | |
| Yes | 25 (17.9) |
| No | 115 (82.1) |
| Peritoneal metastasis | |
| Yes | 14 (10.0) |
| No | 126 (90.0) |
| Primary tumor site | |
| Rectum | 72 (51.4) |
| Colon | 64 (45.7) |
| Small intestine | 4 (2.9) |
| Gene | |
| KRAS mutant | 89 (65.4) |
| KRAS wild type | 47 (34.6) |
| SMI baseline | |
| Male ≥40.8, female ≥34.9 | 33 (43.3) |
| Male <40.8, female <34.9 | 43 (56.5) |
| SMI change | |
| Decrease ≤5% | 55 (74.3) |
| Decrease >5% | 19 (25.7) |
| CEA | |
| ≤5 ng/L | 56 (40.0) |
| >5 ng/L | 84 (60.0) |
| CA19-9 | |
| ≤34 U/mL | 49 (52.1) |
| >34 U/mL | 45 (47.9) |
| Therapeutic drug | |
| <3rd line | 21 (22.6) |
| ≥3rd line | 72 (77.4) |
| Dose administered | |
| 2 mg | 2 (1.4) |
| 3 mg | 64 (45.7) |
| 4 mg | 27 (19.3) |
| 5 mg | 47 (33.6) |
During the data statistics, it was found that some baselines were missing, resulting in a non-uniform total number of cases. PS, performance status; BMI, body mass index; SMI, skeletal muscle mass index; CEA, carcinoembryonic antigen; CA19-9, carbohydrate antigen 19-9.
Efficacy
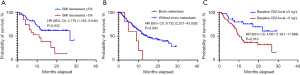
Efficacy evaluation results of the 76 patients are shown in Table 2. The clinical partial response (PR) rate was 15.8% and the disease control rate (DCR) was 90.8%, which suggests that most patients could benefit from fruquintinib treatment. The mOS for the 140 patients was 12.6 months (Figure 1A), and the mPFS was 6.3 months (Figure 1B). In addition, the mOS for the 76 patients was 12.0 months (Figure 1C), and the mPFS was 6.0 months (Figure 1D).
Table 2
| Tumor response criteria by RECIST v.1.1 | No. patients (%) |
|---|---|
| CR | 0 |
| PR | 12 (15.8) |
| SD | 57 (75.0) |
| PD | 7 (9.2) |
| DCR | 69 (90.8) |
CT, computed tomography; CR, complete response; PR, partial response; SD, stable disease; PD, progressive disease; DCR, disease control rate.

By univariate analysis, we noticed that multiple parameters were associated with PFS, such as PS score, body mass index (BMI), brain metastasis, SMI decrease of >5%, baseline carcinoembryonic antigen (CEA) level (Table 3). Further multivariate analysis identified that brain metastasis, and baseline CEA level (>5 ng/L) were independent predictors of PFS (Figure 2). Univariate and multivariate analysis regarding prognostic prediction of OS was performed. The results of univariate analysis indicated that PS score, BMI, primary tumor site, brain metastasis, nutritional prognostic index, SMI decrease of >5%, baseline CEA and carbohydrate antigen 19-9 (CA 19-9) levels (Table 4) can predict patients’ prognosis and survival. Multivariate analysis of these predictors suggested brain metastasis, decrease in SMI of >5%, and baseline CEA level as independent predictors of OS (Figure 3).
Table 3
| Variables | No. patients (%) | Median survival (months) | χ² value | P value |
|---|---|---|---|---|
| Age | 0.172 | 0.67 | ||
| <70 years | 106 (75.7) | 7.90 | ||
| ≥70 years | 34 (24.3) | 7.67 | ||
| Gender | 1.002 | 0.31 | ||
| Male | 92 (65.7) | 8.60 | ||
| Female | 48 (34.3) | 6.30 | ||
| BMI, kg/m2 | 6.093 | 0.01 | ||
| <18.5 | 11 (7.9) | 2.80 | ||
| ≥18.5 | 129 (92.1) | 8.60 | ||
| PS score | 9.155 | 0.002 | ||
| 0 to 1 | 119 (85.0) | 9.00 | ||
| 2 | 21 (15.0) | 2.33 | ||
| Lung metastases | 0.063 | 0.80 | ||
| Yes | 82 (58.6) | 6.77 | ||
| No | 58 (41.4) | 8.60 | ||
| Pelvic metastasis | 0.857 | 0.35 | ||
| Yes | 32 (22.9) | 6.43 | ||
| No | 108 (77.1) | 7.67 | ||
| Brain metastasis | 5.533 | 0.01 | ||
| Yes | 5 (3.6) | 3.30 | ||
| No | 135 (96.4) | 8.60 | ||
| Bone metastasis | 0.958 | 0.32 | ||
| Yes | 25 (17.9) | 6.77 | ||
| No | 115 (82.1) | 8.60 | ||
| Peritoneal metastasis | 0.510 | 0.47 | ||
| Yes | 14 (10.0) | 10.13 | ||
| No | 126 (90.0) | 6.93 | ||
| Primary tumor site | 4.010 | 0.13 | ||
| Rectum | 72 (51.4) | 9.37 | ||
| Colon | 64 (45.7) | 5.70 | ||
| Small intestine | 4 (2.9) | – | ||
| Gene | 0.757 | 0.38 | ||
| KRAS mutant | 89 (65.4) | 7.67 | ||
| KRAS wild type | 47 (34.6) | 9.00 | ||
| NLR | 0.330 | 0.56 | ||
| <3 | 55 (54.5) | 10.13 | ||
| ≥3 | 46 (45.5) | 7.67 | ||
| NLR | 0.023 | 0.88 | ||
| <5 | 83 (82.2) | 7.90 | ||
| ≥5 | 18 (17.8) | 10.90 | ||
| LMR | 0.771 | 0.38 | ||
| <3.75 | 86 (85.1) | 7.90 | ||
| ≥3.75 | 15 (14.9) | 10.13 | ||
| Albumin | 3.308 | 0.06 | ||
| <35 g/L | 19 (19.4) | 4.80 | ||
| ≥35 g/L | 79 (80.6) | 10.13 | ||
| PNI | 2.601 | 0.10 | ||
| <40 | 24 (23.5) | 6.00 | ||
| ≥40 | 78 (76.5) | 10.13 | ||
| SMI baseline | 0.128 | 0.72 | ||
| Male ≥40.8, female ≥34.9 | 33 (43.4) | 10.90 | ||
| Male <40.8, female <34.9 | 43 (56.6) | 7.90 | ||
| SMI change | 4.730 | 0.03 | ||
| Decrease ≤5% | 55 (74.3) | – | ||
| Decrease >5% | 19 (25.7) | 6.43 | ||
| CEA | 8.084 | 0.004 | ||
| ≤5 ng/L | 30 (31.3) | – | ||
| >5 ng/L | 66 (68.8) | 6.23 | ||
| CA19-9 | 2.683 | 0.10 | ||
| ≤34 U/mL | 49 (52.1) | 10.13 | ||
| >34 U/mL | 45 (47.9) | 5.80 | ||
| Therapeutic drug | 0.005 | 0.94 | ||
| <3rd line | 21 (22.6) | 7.67 | ||
| ≥3rd line | 72 (77.4) | 7.90 | ||
| Dose | 6.054 | 0.10 | ||
| 2 mg | 2 (1.4) | 0.70 | ||
| 3 mg | 64 (45.7) | 10.13 | ||
| 4 mg | 27 (19.3) | 8.60 | ||
| 5 mg | 47 (33.6) | 6.00 | ||
During the data statistics, it was found that some baselines were missing, resulting in a non-uniform total number of cases. Because of the different domain values explored, the NLR grouping is repeated. BMI, body mass index; PS, performance status; NLR, neutrophil-to-lymphocyte ratio; LMR, lymphocyte-to-monocyte ratio; PNI, prognostic nutritional index; SMI, skeletal muscle mass index; CEA, carcinoembryonic antigen; CA19-9, carbohydrate antigen 19-9.

Table 4
| Variables | No. patients (%) | Median survival (months) | χ² value | P value |
|---|---|---|---|---|
| Age | 1.933 | 0.16 | ||
| <70 years | 106 (75.7) | 14.47 | ||
| ≥70 years | 34 (24.3) | 11.37 | ||
| Gender | 0.969 | 0.32 | ||
| Male | 92 (65.7) | 14.47 | ||
| Female | 48 (34.3) | 12.37 | ||
| PS score | 11.731 | 0.001 | ||
| 0 to 1 | 119 (85.0) | 15.83 | ||
| 2 | 21 (15.0) | 8.90 | ||
| BMI, kg/m2 | 5.951 | 0.015 | ||
| <18.5 | 11 (7.9) | 6.93 | ||
| ≥18.5 | 129 (92.1) | 14.43 | ||
| Lung metastases | 1.027 | 0.31 | ||
| Yes | 82 (58.6) | 13.17 | ||
| No | 58 (41.4) | 12.37 | ||
| Pelvic metastasis | 2.360 | 0.12 | ||
| Yes | 32 (22.9) | 8.43 | ||
| No | 108 (77.1) | 14.43 | ||
| Brain metastasis | 5.044 | 0.02 | ||
| Yes | 5 (3.6) | 8.90 | ||
| No | 135 (96.4) | 14.07 | ||
| Bone metastasis | 0.589 | 0.44 | ||
| Yes | 25 (17.9) | 11.03 | ||
| No | 115 (82.1) | 13.17 | ||
| Peritoneal metastasis | 0.029 | 0.86 | ||
| Yes | 14 (10.0) | 19.57 | ||
| No | 126 (90.0) | 12.57 | ||
| Primary tumor site | 8.081 | 0.01 | ||
| Rectum | 72 (51.4) | 17.13 | ||
| Colon | 64 (45.7) | 9.83 | ||
| Small intestine | 4 (2.9) | – | ||
| Gene | 0.002 | 0.96 | ||
| KRAS mutant | 89 (65.4) | 14.43 | ||
| KRAS wild type | 47 (34.6) | 13.17 | ||
| NLR | 0.216 | 0.64 | ||
| <3 | 55 (54.5) | 17.13 | ||
| ≥3 | 46 (45.5) | 12.57 | ||
| NLR | 0.005 | 0.94 | ||
| <5 | 83 (82.2) | 12.57 | ||
| ≥5 | 18 (17.8) | 26.73 | ||
| LMR | 0.515 | 0.47 | ||
| <3.75 | 86 (85.1) | 17.13 | ||
| ≥3.75 | 15 (14.9) | 11.90 | ||
| Albumin | 3.640 | 0.05 | ||
| <35 g/L | 19 (19.4) | 8.80 | ||
| ≥35 g/L | 79 (80.6) | 19.57 | ||
| PNI | 4.798 | 0.02 | ||
| <40 | 24 (23.5) | 8.80 | ||
| ≥40 | 78 (76.5) | 19.57 | ||
| SMI baseline | 0.127 | 0.72 | ||
| Male ≥40.8, female ≥34.9 | 33 (43.4) | 26.73 | ||
| Male <40.8, female <34.9 | 43 (56.6) | 17.13 | ||
| SMI change | 6.038 | 0.01 | ||
| Decrease ≤5% | 55 (74.3) | 26.73 | ||
| Decrease >5% | 19 (25.7) | 11.37 | ||
| CEA | 9.119 | 0.003 | ||
| ≤5 ng/L | 56 (40.0) | – | ||
| >5 ng/L | 84 (60.0) | 10.20 | ||
| CA19-9 | 3.832 | 0.050 | ||
| ≤34 U/mL | 49 (52.1) | 22.03 | ||
| >34 U/mL | 45 (47.9) | 9.90 | ||
| Therapeutic drug | 0.003 | 0.95 | ||
| <3rd line | 21 (22.6) | 12.37 | ||
| ≥3rd line | 72 (77.4) | 12.57 | ||
| Dose administered | 5.850 | 0.11 | ||
| 2 mg | 2 (1.4) | 7.57 | ||
| 3 mg | 64 (45.7) | 15.83 | ||
| 4 mg | 27 (19.3) | 19.57 | ||
| 5 mg | 47 (33.6) | 9.83 |
During the data statistics, it was found that some baselines were missing, resulting in a non-uniform total number of cases. Because of the different domain values explored, the NLR grouping is repeated. PS, performance status; BMI, body mass index; NLR, neutrophil-to-lymphocyte ratio; LMR, lymphocyte-to-monocyte ratio; PNI, prognostic nutritional index; SMI, skeletal muscle mass index; CEA, carcinoembryonic antigen; CA19-9, carbohydrate antigen 19-9.
According to the above full-sample analysis and statistical results in this study, a total of two characteristics established the nomogram, brain metastasis, and baseline CEA level (>5 ng/L) with statistical significance (Figure 4A). According to the above full-sample analysis and statistical results in this study, a total of 3 characteristics established the nomogram: brain metastasis, SMI decrease of >5%, and baseline CEA level (>5 ng/L) with statistical significance (Figure 4B).

Safety
According to CTCAE v 5.0, 78 (55.7%) of the 140 patients experienced at least 1 any grade treatment-emergent adverse event (TEAE), among whom, 12 (8.6%) experienced ≥ grade 3 TEAE. Some 78 (55.7%) of the 140 patients experienced at least 1 treatment-related adverse event (TRAE), among whom 8 (5.7%) experienced ≥ grade 3 TEAE. The most common TEAEs were hypertension (24, 17.1%), hand-foot syndrome (20, 14.3%), fatigue (21, 15%), oropharyngeal pain (10, 7.1%), and decreased appetite (10, 7.1%). The most common TRAEs were hypertension (24, 17.1%), fatigue (21, 15%), hand-foot syndrome (20, 14.3%), oropharyngeal pain (10, 7.1%), and decreased appetite (10, 7.1%) (Table 5). There were 9 (13.6%) patients who had a dose reduction due to TRAEs, and 15 (10.7%) patients had treatment discontinuation due to TRAEs. Cox regression analysis showed that hand-foot syndrome, asthenia, and oral mucositis were associated with OS; asthenia, hoarseness, and mucositis oral were associated with PFS prognosis (Table 6).
Table 5
| Adverse events | TEAE, n (%) | TRAE, n (%) | |||
|---|---|---|---|---|---|
| All grade | Grade 3–4 | All grade | Grade 3–4 | ||
| All adverse events | 78 (55.7) | 12 (8.6) | 78 (55.7) | 8 (5.7) | |
| Hypertension | 24 (17.1) | 6 (4.3) | 24 (17.1) | 4 (2.9) | |
| Hand-foot syndrome | 20 (14.3) | 1 (0.7) | 20 (14.3) | 1 (0.7) | |
| Fatigue | 21 (15) | 0 | 21 (15) | 0 | |
| Hoarseness | 12 (8.6) | 0 | 5 (3.6) | 0 | |
| Oropharyngeal pain | 10 (7.1) | 2 (1.4) | 10 (7.1) | 2 (1.4) | |
| Appetite decreased | 10 (7.1) | 0 | 10 (7.1) | 0 | |
| Diarrhea | 8 (5.7) | 0 | 8 (5.7) | 0 | |
| Dysphonia | 7 (5) | 0 | 7 (5) | 0 | |
| Mucositis oral | 5 (3.6) | 1 (0.7) | 5 (3.6) | 0 | |
| Proteinuria | 4 (2.9) | 1 (0.7) | 4 (2.9) | 0 | |
| Abdominal pain | 4 (2.9) | 0 | 4 (2.9) | 0 | |
| Myalgia | 4 (2.9) | 0 | 4 (2.9) | 0 | |
| Constipation | 3 (2.1) | 0 | 2 (1.4) | 0 | |
| Arthralgia | 3 (2.1) | 0 | 3 (2.1) | 0 | |
| Weight decreased | 3 (2.1) | 0 | 3 (2.1) | 0 | |
| Fever | 2 (1.4) | 1 (0.7) | 1 (0.7) | 0 | |
| Platelet count decreased | 2 (1.4) | 1 (0.7) | 2 (1.4) | 1 (0.7) | |
| Peripheral sensory nerve disorder | 2 (1.4) | 0 | 2 (1.4) | 0 | |
| Eczema | 2 (1.4) | 0 | 2 (1.4) | 0 | |
| Myocardial infarction | 1 (0.7) | 1 (0.7) | 0 | 0 | |
| Diabetes | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Intestinal obstruction | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Cold | 1 (0.7) | 0 | 0 | 0 | |
| Anorectal infection | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Hyperuricemia | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Testicular pain | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Hypothyroidism | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Urinary tract infection | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Pruritus | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Cognitive disorder | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Headache | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Vertigo | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Alopecia | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Hematuria | 1 (0.7) | 0 | 1 (0.7) | 0 | |
| Back pain | 1 (0.7) | 0 | 1 (0.7) | 0 | |
TEAE, treatment-emergent adverse event; TRAE, treatment-related adverse event.
Table 6
| Variables | Median survival (months) | χ² value | P value |
|---|---|---|---|
| Univariate analysis of adverse reactions and OS | |||
| Hand-foot syndrome | 4.428 | 0.03 | |
| Yes | 22.03 | ||
| None | 11.90 | ||
| Asthenia | 3.986 | 0.04 | |
| Yes | 7.60 | ||
| None | 14.07 | ||
| Oral mucositis | 5.417 | 0.02 | |
| Yes | 8.43 | ||
| None | 14.07 | ||
| Univariate analysis of adverse reactions and PFS | |||
| Asthenia | 5.003 | 0.02 | |
| Yes | 2.97 | ||
| None | 8.60 | ||
| Hoarseness | 4.340 | 0.03 | |
| Yes | 2.13 | ||
| None | 8.60 | ||
| Oral mucositis | 8.976 | 0.003 | |
| Yes | 2.50 | ||
| None | 9.00 | ||
OS, overall survival; PFS, progression-free survival.
Discussion
The latest Chinese cancer epidemiology study reported that CRC ranks second with 517,100 new cases per year (3). When it comes to such a huge patient population, the treatment of CRC patients is particularly important. Fruquintinib is used as the standard third-line treatment regimen for advanced CRC (4). The FRESCO (7) and FRESCO-2 (14) studies demonstrated a consistent PFS of 3.7 months in the fruquintinib group, and the PFS observed in other small-sample real-world studies is around 5–7 months (15,16). In this study, a PFS of 6.3 months and an OS of 12.6 months was achieved, which may be related to individualized treatment strategy, and experienced AE management in our centers. Patients have a higher average duration and intensity of medication, thus resulting in better efficacy and survival prognosis. We aimed to identify the specific patients who can achieve significant survival benefits from fruquintinib treatment. This study analyzed 140 real-world cases of advanced CRC treated with fruquintinib, and for the first time analyzed the prognostic predictive relationship between sarcopenia and fruquintinib, identifying independent predictors associated with prognosis through Cox regression, forming an effective predictive model.
Sarcopenia is an important marker of malnutrition and a study has used the SMI of the third lumbar spine to diagnose sarcopenia in patients (17). Sarcopenia is a syndrome characterized by progressive, generalized SML and hypofunction. The European Working Group on Sarcopenia in the Elderly Patients considered that sarcopenia is a progressive, systemic skeletal muscle disorder that may increase the likelihood of adverse outcomes such as falls, fractures, physical disability, and death (18). Tumor-associated sarcopenia not only affects the normal metabolism of body components, but also reduces the therapeutic efficacy, quality of life, and survival of patients (19). Studies have suggested that release of inflammatory cytokines such as interleukin 1 (IL-1), tumor necrosis factor-α (TNF-α), and interleukin 6 (IL-6) may be associated with sarcopenia, and alterations in these parameters may affect the prognosis of advanced CRC (20,21).
Several small studies have indicated that patients with advanced CRC who developed sarcopenia after treatment with TAS-102 or regorafenib had a lower 1-year survival rate. Sarcopenia is considered a poor prognostic factor in patients with CRC (22-24), but no studies have confirmed any specific values or proportion of muscle decrease can predict the survival prognosis of patients with CRC. The analysis in this study showed that sarcopenia and other clinical indicators were associated with survival prognosis in advanced CRC treated with fruquintinib. In prognosis prediction of PFS and OS, PS score 2, BMI <18.5 kg/m2, and SMI decrease >5% all showed shorter OS; conversely, PFS and OS were significantly prolonged by PS scores 0–1, BMI ≥18.5 kg/m2, and SMI reduction ≤5%, which means that good general condition and good maintenance of nutritional status during treatment will bring longer survival benefits. Further multivariate analysis identified that SMI reduction >5% was an independent predictor of OS. Therefore, during fruquintinib treatment, we should continuously monitor the nutritional status of patients, conduct timely nutritional risk assessment and intervention, and maintain a good SMI, to ensure that patients are keep benefiting from the treatment.
As a classical tumor marker in CRC patients, the application value of CEA is widely known in clinical practice. Subgroup analysis of the FRESCO study noticed that early alterations in CEA might be a potential predictor (25). In this study, we noticed that baseline CEA may associate with the PFS and OS of patients who underwent fruquintinib treatment: baseline CEA levels ≤5 ng/L compared with >5 ng/L, mOS: not yet reached (NR) vs. 10.2 months (P=0.003), mPFS: NR vs. 6.23 months (P=0.004); further multivariate analysis identified baseline CEA level as an independent predictor of fruquintinib treatment in patients with advanced CRC.
From the clinical characteristics of patients, primary tumor site, brain metastasis could affect the OS, whereas brain metastasis was independent predictors of PFS and OS. This means that patients with this clinical characteristic can receive early interventional therapy with fruquintinib to improve their condition.
In this study, the incidence of any grade or ≥ grade 3 TEAEs and TRAEs is lower than that in the FRESCO and other studies (7,9,10). This difference could be explained by the nature of real-world studies. A prospective randomized trial requires a very specific follow up visit plan, in which the regular laboratory test can help physicians identify many asymptomatic AEs, such as proteinuria, elevated transaminases, abnormal blood cells, and so on. In the real-world setting, patients are not strictly followed and most of the AEs are collected from their chief complaint during follow up consultation. The most common TEAEs in this study were hypertension (24, 17.1%), hand-foot syndrome (20, 14.3%), and fatigue (21, 15%) the incidences of which were similar to those in a previous report (7). Patients with an underlying medical history had a higher incidence and grade of TEAEs. Therefore, very careful AE monitoring and management is particularly required for this population. In addition, this study found that the occurrence of fatigue and oral mucositis was associated with PFS and OS, but the incidence of this two AEs were low and independent predictive factor analysis could not be performed, which could be used as a clinical prompt. When this AE occurs in the future treatment process, patients should be encouraged to adhere to the medication and cannot arbitrarily discontinue the drug or reduce the dose, to ensure the efficacy of the treatment.
Conclusions
In conclusion, the real-world efficacy and safety are numerically superior to those in the FRESCO study. This study firstly clarified the relationship between sarcopenia and prognosis prediction of these patients. We also noticed that brain metastasis, SMI decrease of >5%, and baseline CEA level (>5 ng/L) may indicate prognosis.
Acknowledgments
Thanks to the following hospitals for their contributions: The Affiliated Lihuili Hospital of Ningbo University, Ningbo Medical Center Lihuili Hospital, The Affiliated People’s Hospital of Ningbo University, The First Affiliated Hospital of Ningbo University, Ningbo Municipal Hospital of Traditional Chinese Medicine, Affiliated Hospital of Zhejiang Chinese Medical University.
Funding: This study was supported by
Footnote
Reporting Checklist: The authors have completed the STROBE reporting checklist. Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-559/rc
Data Sharing Statement: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-559/dss
Peer Review File: Available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-559/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jgo.amegroups.com/article/view/10.21037/jgo-24-559/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Ningbo No. 2 Hospital Human Research Ethics Committee (No. PJ-NBEY-KY-2019-146-01) and informed consent was taken from all the patients. All participating hospitals/institutions were informed and agreed with this study.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2024;74:229-63. [Crossref] [PubMed]
- Benson AB, Venook AP, Al-Hawary MM, et al. Colon Cancer, Version 2.2021, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2021;19:329-59. [Crossref] [PubMed]
- Zheng RS, Chen R, Han BF, et al. Cancer incidence and mortality in China, 2022. Zhonghua Zhong Liu Za Zhi 2024;46:221-31. [PubMed]
- Chen Z, Jiang L. The clinical application of fruquintinib on colorectal cancer. Expert Rev Clin Pharmacol 2019;12:713-21. [Crossref] [PubMed]
- Deng Y, Li X. Fruquintinib and its use in the treatment of metastatic colorectal cancer. Future Oncol 2019;15:2571-6. [Crossref] [PubMed]
- Li J, Guo W, Bai Y, et al. Safety Profile and Adverse Events of Special Interest for Fruquintinib in Chinese Patients with Previously Treated Metastatic Colorectal Cancer: Analysis of the Phase 3 FRESCO Trial. Adv Ther 2020;37:4585-98. [Crossref] [PubMed]
- Li J, Qin S, Xu RH, et al. Effect of Fruquintinib vs Placebo on Overall Survival in Patients With Previously Treated Metastatic Colorectal Cancer: The FRESCO Randomized Clinical Trial. JAMA 2018;319:2486-96. [Crossref] [PubMed]
- Dasari A, Sobrero A, Yao J, et al. FRESCO-2: a global Phase III study investigating the efficacy and safety of fruquintinib in metastatic colorectal cancer. Future Oncol 2021;17:3151-62. [Crossref] [PubMed]
- Li J, Wang Z, Zhong H, et al. A phase IV study to evaluate the safety of fruquintinib in Chinese patients in real-world clinical practice. Oncologist 2024;29:e1012-9. [Crossref] [PubMed]
- Li L, Wang T, Wu Z, et al. Fruquintinib in combination with sintilimab or TAS-102 as third-line or above treatment in patients with metastatic colorectal cancer: a real-world study. Transl Cancer Res 2023;12:3034-44. [Crossref] [PubMed]
- Gomez-Perez SL, Haus JM, Sheean P, et al. Measuring Abdominal Circumference and Skeletal Muscle From a Single Cross-Sectional Computed Tomography Image: A Step-by-Step Guide for Clinicians Using National Institutes of Health ImageJ. JPEN J Parenter Enteral Nutr 2016;40:308-18. [Crossref] [PubMed]
- Prado CM, Lieffers JR, McCargar LJ, et al. Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 2008;9:629-35. [Crossref] [PubMed]
- Zhuang CL, Huang DD, Pang WY, et al. Sarcopenia is an Independent Predictor of Severe Postoperative Complications and Long-Term Survival After Radical Gastrectomy for Gastric Cancer: Analysis from a Large-Scale Cohort. Medicine (Baltimore) 2016;95:e3164. [Crossref] [PubMed]
- Dasari A, Yao JC, Sobrero AF, et al. FRESCO-2: A global phase III study of the efficacy and safety of fruquintinib in patients (pts) with metastatic colorectal cancer (mCRC). J Clin Oncol 2021;39:TPS154. [Crossref]
- Zhang Q, Chen M, Wang Z, et al. Efficacy and Safety Comparison of Regorafenib and Fruquintinib in Metastatic Colorectal Cancer-An Observational Cohort Study in the Real World. Clin Colorectal Cancer 2022;21:e152-61. [Crossref] [PubMed]
- Jin Y, Li J, Shen L, et al. A multi-center effectiveness comparison study of fruquintinib with constructed external control cohort of other targeted kinase inhibitors using real-world data in third-line treatment of metastatic colorectal cancer. Front Oncol 2022;12:1044328. [Crossref] [PubMed]
- Keshoofi P, Schindler P, Rennebaum F, et al. Imaging-based diagnosis of sarcopenia for transplant-free survival in primary sclerosing cholangitis. BMC Gastroenterol 2024;24:145. [Crossref] [PubMed]
- Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019;48:16-31. [Crossref] [PubMed]
- Yokoi K, Watanabe A, Yokota K, et al. Low skeletal muscle radiodensity is a risk factor for adjuvant chemotherapy discontinuation in colorectal cancer. Int J Clin Oncol 2024;29:276-85. [Crossref] [PubMed]
- Di W, Luyao Y, Chengwei Y, et al. Exploring the causal link between circulating cytokines and sarcopenia traits: A Mendelian randomization analysis. Environ Toxicol 2024;39:3434-47. [Crossref] [PubMed]
- Pei J, Gao Y, Wu A. An inflammation-related subtype classification for analyzing tumor microenvironment and clinical prognosis in colorectal cancer. Front Immunol 2024;15:1369726. [Crossref] [PubMed]
- Bekir Hacioglu M, Kostek O, Kurt N, et al. Comparison of skeletal muscle mass loss in patients with metastatic colorectal cancer treated with regorafenib or TAS-102. J BUON 2019;24:2198-204. [PubMed]
- Huemer F, Schlintl V, Hecht S, et al. Regorafenib Is Associated With Increased Skeletal Muscle Loss Compared to TAS-102 in Metastatic Colorectal Cancer. Clin Colorectal Cancer 2019;18:159-166.e3. [Crossref] [PubMed]
- Malik M, Michalak M, Radecka B, et al. Prognostic Value of Sarcopenia in Metastatic Colorectal Cancer Patients Treated with Trifluridine/Tipiracil. J Clin Med 2021;10:5107. [Crossref] [PubMed]
- Bai Y, Qin S, Li J, et al. Early carcinoembryonic antigen (CEA) dynamics to predict fruquintinib efficacy in FRESCO, a 3+ line metastatic colorectal carcinoma (mCRC) phase III trial. J Clin Oncol 2020;38:e16001. [Crossref]
(English Language Editor: J. Jones)


